Meningioma
Meningioma a very common tumour in neuropathology.
| Meningioma | |
|---|---|
| Diagnosis in short | |
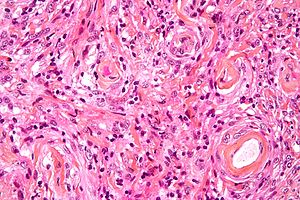 Meningioma. H&E stain. | |
|
| |
| LM | whorled appearance, calcification - psammomatous, +/-nuclear pseudoinclusions |
| Subtypes | Grade I (meningothelial, fibrous, transistional, psammomatous, angiomatous, microcystic, secretory, lymphoplasmacyte-rich, metaplastic), Grade II (invasive, clear cell, chordoid), Grade III (papillary, rhabdoid) |
| LM DDx | schwannoma, solitary fibrous tumour, others |
| IHC | EMA +ve, keratins usu. -ve, CD34 -ve/+ve, S-100 -ve (usu.), PR +ve (-ve in more aggressive ones) |
| Site | see CNS tumours |
|
| |
| Syndromes | neurofibromatosis 2, nevoid basal cell carcinoma syndrome,Cowden syndrome |
|
| |
| Clinical history | +/-radiation |
| Prevalence | common |
| Radiology | extra-axial, intradural lesion |
| Prognosis | usually benign, dependent on grade |
| Clin. DDx | dependent on site - see CNS tumours |
| Treatment | surgical removal |
General
Prevalence
Prognosis
- Most are benign - usu. a good prognosis.
- May be malignant - bad prognosis.
Genetics
- May be seen in genetic disorders such as:
- Neurofibromatosis 2 (NF2).[3]
- Nevoid basal cell carcinoma syndrome (Gorlin syndrome).[4][5]
- Cowden syndrome.
Gross/Radiology
- Extra-axial, intradural.
- Can be extradural - very rare.[6]
Microscopic
Features (memory device WCN):
- Whorled appearance - key feature.
- Calcification, psammomatous (target-like appearance; (tight) onion skin).
- +/-Nuclear pseudoinclusions - focal nuclear clearing with a sharp interface to unremarkable chromatin.
Notes:
- May involute into benign sclerotic tissue.[7]
- Thick-walled blood vessels -> think schwannoma.
DDx:
- Schwannoma - especially at CP angle.
- Solitary fibrous tumour.
- Hemangiopericytoma.
- Others - see subtypes.
Images
www:
Morphologic subtypes
- Many subtypes exist.[8]
- The histologic subtypes generally don't have much prognostic significance.
- Some subtypes are high grade by definition; also see histologic grading.
Grade I
Meningothelial meningioma
- Most common.
Microscopic:
- Syncytial, nuclear clearing (pseudoinclusions).
Fibrous meningioma
- AKA fibroblastic meningioma.
- Not collagen... but looks like it.
- It is really laminin or fibronectin.
Transistional meningioma
- Rare.
Psammomatous meningioma
Microscopic:
Angiomatous meningioma
- AKA vascular.
- May bleed like stink.
Microcystic meningioma
Microscopic:
- Cystic appearance.
Secretory meningioma
- Associated with brain edema; may have a worse outcome.
Microscopic:[9]
- Eosinophilic intracytoplasmic inclusions that are CEA +ve and PAS +ve.
DDx:
- Metastatic mucinous adenocarcinoma.
Images:
Lymphoplasmacyte-rich meningioma
Microscopic:
- Lymphocytes.
- Plasma cells.
Images:
- Lymphoplasmacyte-rich meningioma - case 1 - several images (upmc.edu).
- Lymphoplasmacyte-rich meningioma - case 2 - several images (upmc.edu).
- Lymphoplasmacyte-rich meningioma - case 3 - several images (upmc.edu).
Metaplastic meningioma
- Much talked about... but very rare.
Microscopic:
- Cartilage or bone formation.
Grade II
Invasive meningioma
- Invades the brain.
Images:
Clear cell meningioma
Epidemiology:
- Usu. spinal cord.[11]
Microscopic:
- Clear cells - contain glycogen (PAS +ve).
Images:
Chordoid meningioma
- Chordoma-like.
Microscopic:
- Myxoid appearance.
Image:
Grade III
Papillary meningioma
Microscopic:
- True papillae.
Rhabdoid meningioma
Microscopic:
- Rhabdoid appearance (abundant cytoplasm).
- Cross-striations.
Images:
- Rhabdoid meningioma - case 1 - several images (upmc.edu).
- Rhabdoid meningioma - case 2 - several images (upmc.edu).
Histologic grading
Grading:[8]
- Grade 1:
- Low mitotic rate (< 4 mitoses/10 HPF - for whatever HPF means, see HPFitis).
- Excludes clear cell, chordoid, papillary, and rhabdoid subtypes.
- Grade 2 (either #1, #2 or #3):
- Brain-invasive meningioma.
- Protrusion of meningioma into brain.
- Meninogioma with entraped GFAP +ve tissue.
- Protrusion of meningioma into brain.
- Atypical meningioma (by histomorphology) - either A or B.
- A. Intermediate mitotic rate (>= 4 mitoses/10 HPF - for whatever HPF means, see HPFitis.)
- B. Three of the following five features:
- Clear cell or chordoid subtype.
- Brain-invasive meningioma.
- Grade 3 (either of the following):
- High mitotic rate (>=20 mitoses/10 HPF - for whatever HPF means, see HPFitis.)
- "Frank anaplasia"; marked nuclear atypia.
- Papillary or rhabdoid subtype.
Notes:
- Grade II soft criteria memory device HMNs: hypercellular, macronucleoli, NC ratio increased, necrosis, sheeting.
IHC
- EMA +ve.[12]
- Other CKs usually -ve.
DDx of meningioma & IHC[13]
- S-100 +ve - schwannoma.
- +ve in ~80% of fibrous meningiomas.
- CD34 +ve - solitary fibrous tumour.
- +ve in ~60% of fibrous meningiomas.
- EMA +ve in ~30% of hemangiopericytoma.
- Claudin-1 - new kid on the block: +ve in meningioma, but low sensitivity.
Standard work-up (UHN)
See also
References
- ↑ Rogers, L.; Barani, I.; Chamberlain, M.; Kaley, TJ.; McDermott, M.; Raizer, J.; Schiff, D.; Weber, DC. et al. (Oct 2014). "Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review.". J Neurosurg: 1-20. doi:10.3171/2014.7.JNS131644. PMID 25343186.
- ↑ Baldi, I.; Engelhardt, J.; Bonnet, C.; Bauchet, L.; Berteaud, E.; Grüber, A.; Loiseau, H. (Sep 2014). "Epidemiology of meningiomas.". Neurochirurgie. doi:10.1016/j.neuchi.2014.05.006. PMID 25249493.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm. Accessed on: 26 October 2010.
- ↑ Kimonis, VE.; Mehta, SG.; Digiovanna, JJ.; Bale, SJ.; Pastakia, B.. "Radiological features in 82 patients with nevoid basal cell carcinoma (NBCC or Gorlin) syndrome.". Genet Med 6 (6): 495-502. doi:10.109701.GIM.0000145045.17711.1C. PMID 15545745.
- ↑ Lee, CW.; Tan, TC. (Feb 2014). "Meningioma associated with Gorlin's syndrome.". J Clin Neurosci 21 (2): 349-50. doi:10.1016/j.jocn.2013.02.033. PMID 24100109.
- ↑ URL: http://path.upmc.edu/cases/case702.html. Accessed on: 2 February 2012.
- ↑ URL: http://radiographics.rsna.org/content/23/3/785.long. Accessed on: 3 November 2010.
- ↑ 8.0 8.1 Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 194. ISBN 978-0443069826.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com04/Com405-1-Diss.htm. Accessed on: 12 October 2011.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com04/Com405-1-Diss.htm. Accessed on: 3 January 2012.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 200. ISBN 978-0443069826.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 13. ISBN 978-0443069826.
- ↑ Hahn HP, Bundock EA, Hornick JL (February 2006). "Immunohistochemical staining for claudin-1 can help distinguish meningiomas from histologic mimics". Am. J. Clin. Pathol. 125 (2): 203–8. doi:10.1309/G659-FVVB-MG7U-4RPQ. PMID 16393681. http://ajcp.ascpjournals.org/content/125/2/203.full.pdf.
- ↑ Croul, SE. 8 November 2010.
- ↑ Takei, H.; Buckleair, LW.; Powell, SZ. (Feb 2008). "Immunohistochemical expression of apoptosis regulating proteins and sex hormone receptors in meningiomas.". Neuropathology 28 (1): 62-8. doi:10.1111/j.1440-1789.2007.00852.x. PMID 18021195.
- ↑ Tao, Y.; Liang, G.; Li, Z.; Wang, Y.; Wu, A.; Wang, H.; Lu, Y.; Liu, Z. et al. (May 2012). "Clinical features and immunohistochemical expression levels of androgen, estrogen, progesterone and Ki-67 receptors in relationship with gross-total resected meningiomas relapse.". Br J Neurosurg. doi:10.3109/02688697.2012.685780. PMID 22616825.