Crohn's disease
Jump to navigation
Jump to search
Crohn's disease, abbreviated as CD, is a type of inflammatory bowel disease. It is the bread and butter of gastroenterology, and is often seen by pathologists.
| Crohn's disease | |
|---|---|
| Diagnosis in short | |
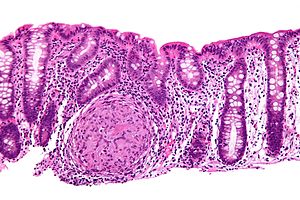 Crohn's disease. H&E stain. | |
| LM DDx | ulcerative colitis, infectious colitis, ischemic colitis, Diverticular disease-associated colitis, others |
| Gross | aphthous ulcer, transmural inflammation, creeping fat, cobblestone appearance, serpiginous ulcers, classically with patchy involvement (unlike UC) |
| Site | small bowel (esp. terminal ileum), colon, rectum, stomach, duodenum, esophagus, others |
|
| |
| Associated Dx | colorectal adenocarcinoma (increased risk) |
| Clinical history | +/-family history of inflammatory bowel disease |
| Signs | +/-diarrhea, +/-blood per rectum |
| Symptoms | +/-abdominal pain |
| Radiology | segmental bowel wall changes, classically with terminal ileum involvement |
| Endoscopy | cobblestone appearance, serpiginous ulcers, patchy involvement, terminal ileum classically affected |
| Clin. DDx | infectious colitis, ulcerative colitis |
General
- Autoimmune disease.
- Increased risk for cancer - usu. rectal cancer; classically mucinous adenocarcinoma.
Associations:[1]
- High socioeconomic status.
- Family history of IBD.
- City dwellers.
- Not breastfed.
Treatment:
- Immune suppression.
- Surgery considered treatment of last resort.
Gross
- Aphthous ulcer - first gross finding of IBD.
- Transmural inflammation, i.e. full thickness of bowel wall.
- Creeping fat (also "fat wrapping" and "fat hypertrophy"[2]) - abundant fat, fat on anti-mesenteric side of the bowel.[3]
- Definition: fat on more than 50% of the intestinal surface.[2]
- LP understands this as fat on 50% of the circumference.
- DDx of creeping fat: ulcerative colitis, sclerosing mesenteritis, mesenteric panniculitis, epiploic appendagitis, omental infarction, gastrointestinal complication a renal transplant, idiopathic segmental ureteritis.[4]
- Can be seen radiologically.
- Definition: fat on more than 50% of the intestinal surface.[2]
- Cobblestone appearance -- may be described as such on endoscopy; due to edema.
- Serpiginous ulcers.
Notes:
- Grossly, the margins should be clear of disease; the surgical clearance and microscopic involvement are not considered important.[5]
- The term creeping fat may be used in the context of a vasculitis outside of the abdominal cavity.[4]
Microscopic
Features:[6]
- Segmental crypt architectural abnormalities.
- Mucin depletion -- less goblet cells. (???)[7]
- Mucin preservation at the active sites.
- Focal chronic inflammation without crypt atrophy.
- Pseudopyloric mucous glands (AKA pyloric gland metaplasia).[8]
- Round glands with abundant pale cytoplasm - stubby champagne flute.
- Usually in the deep aspect of the mucosa.
- Look somewhat similar to Brunner's glands.
- Granulomas - esp. deep (non-mucosal).
- Superficial granulomas in the mucosa are non-specific (especially if they are beside an inflamed crypt); they may be present in ulcerative colitis.[9][10]
DDx:
- Infectious colitis:
- Ulcerative colitis.
- Diverticular disease-associated colitis - only in areas with diverticular disease.
- NSAID-induced small bowel injury.[12]
- Others - a long DDx is here.[13]
Images
www:
Sign-out
Biopsies
TERMINAL ILEUM, BIOPSY - PATCHY MILD ACTIVE ILEITIS. COMMENT: No granulomas are identified. An infective etiology should be considered, as it cannot be excluded on pathologic grounds.
TERMINAL ILEUM, BIOPSY: - MILD PATCHY ACTIVE ILEITIS WITH MILD CHRONIC CHANGES. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomata are identified. The villous architecture is largely preserved. Pseudopyloric mucous glands are present focally. The changes are compatible with Crohn's disease; however, other causes of inflammation should be considered clinically.
Classic
A. TERMINAL ILEUM, BIOPSY - MODERATE GRANULOMATOUS ILEITIS. B. CECUM, BIOPSY: - MILD PATCHY ACTIVE CECITIS. C. SIGMOID COLON, BIOPSY: - CHRONIC INFLAMMATORY CHANGES. NO ACTIVE COLITIS. COMMENT: The histomorphological findings (patchy inflammation, granulomas, ileitis, paneth cell metaplasia, crypt loss and crypt elongation) are suggestive of Crohn's disease. An infective etiology should be considered, as it cannot be excluded on pathologic grounds.
Quiescent Crohn's disease
DESCENDING COLON, BIOPSY: - COLONIC MUCOSA WITH PROMINENT LAMINA PROPRIA PLASMA CELLS. - NEGATIVE FOR ACTIVE COLITIS. COMMENT: Minimal architectural changes consistent with chronic inflammation are present. There are no granulomas. No dysplasia is identified. The findings are compatible with quiescent Crohn's disease.
Resection
TERMINAL ILEUM, CECUM, AND APPENDIX, CECUM-ILEUM RESECTION: - CHRONIC ACTIVE GRANULOMATOUS ILEITIS -- INCLUDING: -- MURAL MICROABSCESS FORMATION. -- SEROSITIS. -- A STRICTURE. -- DEEP ULCERATION (AT LEAST THROUGH THE MUSCULARIS PROPRIA). - PERIAPPENDICITIS, NEGATIVE FOR APPENDICITIS. - CECUM WITHIN NORMAL LIMITS. - TEN LYMPH NODES NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 10 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The sections show patchy transmural inflammation and skip lesions. The findings are consistent with Crohn's disease.
TERMINAL ILEUM, CECUM, APPENDIX, AND ASCENDING COLON, RIGHT HEMICOLECTOMY: - CHRONIC ACTIVE ILEITIS -- INCLUDING: -- INFLAMMATORY PSEUDOPOLYP. -- STRICTURE ASSOCIATED WITH LARGE LYMPHOID AGGREGATE. - THIRTEEN LYMPH NODES NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 13 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The sections show patchy transmural inflammation and skip lesions. Submucosal fibrosis is present. Focal ulceration and abscess formation is identified. No granulomas are identified. The findings are consistent with Crohn's disease.
ILEUM, COLON, ILEO-COLIC RESECTION: - SEVERE FOCAL ILEITIS WITH ULCERATION AND TRANSMURAL INFLAMMATION. - BENIGN STRICTURE ASSOCIATED WITH A LARGE LYMPHOID AGGREGATE. - FIBROUS ADHESION. - COLON WITHIN NORMAL LIMITS. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with chronic, active Crohn's disease.
See also
References
- ↑ Gearry, RB.; Richardson, AK.; Frampton, CM.; Dodgshun, AJ.; Barclay, ML. (Feb 2010). "Population-based cases control study of inflammatory bowel disease risk factors.". J Gastroenterol Hepatol 25 (2): 325-33. doi:10.1111/j.1440-1746.2009.06140.x. PMID 20074146.
- ↑ 2.0 2.1 Schäffler, A.; Herfarth, H. (Jun 2005). "Creeping fat in Crohn's disease: travelling in a creeper lane of research?". Gut 54 (6): 742-4. doi:10.1136/gut.2004.061531. PMID 15888774.
- ↑ Schäffler, A.; Herfarth, H. (Jun 2005). "Creeping fat in Crohn's disease: travelling in a creeper lane of research?". Gut 54 (6): 742-4. doi:10.1136/gut.2004.061531. PMID 15888774.
- ↑ 4.0 4.1 Golder, WA. (Jan 2009). "The "creeping fat sign"-really diagnostic for Crohn's disease?". Int J Colorectal Dis 24 (1): 1-4. doi:10.1007/s00384-008-0585-y. PMID 18815796.
- ↑ Hamilton, SR. (1983). "Pathologic features of Crohn's disease associated with recrudescence after resection.". Pathol Annu 18 Pt 1: 191-203. PMID 6348672.
- ↑ Tanaka, M.; Riddell, RH.; Saito, H.; Soma, Y.; Hidaka, H.; Kudo, H. (Jan 1999). "Morphologic criteria applicable to biopsy specimens for effective distinction of inflammatory bowel disease from other forms of colitis and of Crohn's disease from ulcerative colitis.". Scand J Gastroenterol 34 (1): 55-67. PMID 10048734.
- ↑ McCormick DA, Horton LW, Mee AS (February 1990). "Mucin depletion in inflammatory bowel disease". J. Clin. Pathol. 43 (2): 143–6. PMC 502296. PMID 2318990. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC502296/.
- ↑ 8.0 8.1 8.2 URL: http://www.medunigraz.at/22698. Accessed on: 6 August 2013.
- ↑ Shepherd, NA. (Aug 2002). "Granulomas in the diagnosis of intestinal Crohn's disease: a myth exploded?". Histopathology 41 (2): 166-8. PMID 12147095.
- ↑ Mahadeva, U.; Martin, JP.; Patel, NK.; Price, AB. (Jul 2002). "Granulomatous ulcerative colitis: a re-appraisal of the mucosal granuloma in the distinction of Crohn's disease from ulcerative colitis.". Histopathology 41 (1): 50-5. PMID 12121237.
- ↑ Karlitz, JJ.; Li, ST.; Holman, RP.; Rice, MC. (Jan 2011). "EBV-associated colitis mimicking IBD in an immunocompetent individual.". Nat Rev Gastroenterol Hepatol 8 (1): 50-4. doi:10.1038/nrgastro.2010.192. PMID 21119609.
- ↑ Hayashi, Y.; Yamamoto, H.; Taguchi, H.; Sunada, K.; Miyata, T.; Yano, T.; Arashiro, M.; Sugano, K. (2009). "Nonsteroidal anti-inflammatory drug-induced small-bowel lesions identified by double-balloon endoscopy: endoscopic features of the lesions and endoscopic treatments for diaphragm disease.". J Gastroenterol 44 Suppl 19: 57-63. doi:10.1007/s00535-008-2277-3. PMID 19148795.
- ↑ Dilauro, S.; Crum-Cianflone, NF. (Aug 2010). "Ileitis: when it is not Crohn's disease.". Curr Gastroenterol Rep 12 (4): 249-58. doi:10.1007/s11894-010-0112-5. PMID 20532706.
- ↑ Goldstein, N.; Dulai, M. (Sep 2006). "Contemporary morphologic definition of backwash ileitis in ulcerative colitis and features that distinguish it from Crohn disease.". Am J Clin Pathol 126 (3): 365-76. doi:10.1309/UAXMW3428PGN9HJ3. PMID 16880149.