Hepatocellular carcinoma
Jump to navigation
Jump to search
Hepatocellular carcinoma, abbreviated HCC, is a common primary malignant liver tumour that most often arises in the context of cirrhosis.
| Hepatocellular carcinoma | |
|---|---|
| Diagnosis in short | |
 Hepatocellular carcinoma. | |
|
| |
| LM | architectural changes - liver plate thickness >3 cells thick, +/-nuclear changes of malignancy (very common), variable architecture (pseudoglandular, trabecular, fibrolamellar, solid) |
| Subtypes | sclerosing HCC, fibrolamellar HCC |
| LM DDx | cholangiocarcinoma, occasionally liver metastasis, high-grade dysplasia |
| Stains | reticulin (thickened liver plate) |
| IHC | CD34 +ve sinusoids, HepPar-1 +ve (usu.), AFP +ve (usu.), CK8/18 +ve, glypican-3 +ve |
| Gross | usu. cirrhosis (micronodular or macronodular) |
| Site | liver - see liver neoplasms |
|
| |
| Associated Dx | causes of cirrhosis, e.g. chronic alcoholism, Hepatitis C, Hepatitis B, hereditary hemochromatosis, others |
| Prevalence | most common malignant primary liver tumour, less common than metastases |
| Blood work | +/-AFP elevation |
| Prognosis | moderate to poor |
| Clin. DDx | liver metastasis, other liver tumours |
General
Clinical:
- Serum AFP elevated - in approx. 50% of patients.[1]
- Treatments: RFA (radiofrequency ablation), ethanol ablation, liver resection, liver transplant.[2]
- Mean survival at time of diagnosis ~6 months.[2]
Epidemiology:
- Highest where prevalence of hepatitis B virus (HBV) is high.[3]
- HCC generally arises in the setting of cirrhosis.
- Cirrhosis may be regressed and therefore not appreciated.
HCCs without cirrhosis:
- Hepatitis B virus.[3]
- Hemochromatosis.
- Fibrolamellar HCC.
- Chronic alcoholism.
- Hepatitis C virus (HCV) - chronic infection.
- Hepatitis B virus (HBV) - chronic infection.
- Aflatoxins (food contaminant - mould).[2]
- Hereditary tyrosinemia.
- Hereditary hemochromatosis.
Gross
Features:[5]
- Unifocal, multifocal or diffusely infiltrative.
- Pale in relation to surrounding liver or green (due to bile secretion).
Images
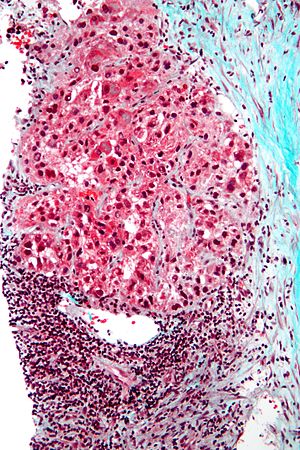
Microscopic
Requirements:[8]
- Architectural changes.
- Liver plate more than 3 cells thick - key feature.
- Loss of reticulin scaffold - incomplete loss is considered significant.
- CD34+ staining cells, suggesting loss of epithelial cells that form the sinusoids.
- Loss of structures seen in a normal liver lobule (bile ductules, portal triad).
- Invasion of the portal tract - useful in well-diff. lesions.[9]
Additional findings:[10]
- Nuclear changes.
- Increased NC ratio - key feature if present.
- Nuclear hyperchromasia.
- Abnormal nuclear contour.
- Mitoses.
- Cytoplasmic changes.
- Cytoplasmic hyperchromasia, clearing or lighter staining.
Varied architecture - may be:[11]
- Pseudoglandular - can be confused with adenocarcinoma.
- Trabecular.
- Fibrolamellar.
- Solid.
Notes:
- HCC with trabecular morphology has some resemblance to normal liver - but has extra cells.
- Fibrolamellar - better prognosis, classically in young adults.
- Stroma is usually scant.[12]
ASIDE:
- Trabecula = little beam.
DDx:
- Cholangiocarcinoma.
- Combined HCC-CC.[13]
- high-grade dysplasia.
Images
Fibrolamellar hepatocellular carcinoma
- Abbreviated fibrolamellar HCC, FL-HCC, and FHCC.
General
- Rare variant.
- Classically afflicts younger patients.
- Mean age at onset ~27 years in one study.[14]
- Individuals usually do not have the classic risk factors for HCC, i.e. no cirrhosis, no hepatitis.[14]
Clinical:
- AFP usu. not elevated.[14]
Microscopic
Features:[15]
- Large polygonal tumours cells with:
- Graunular eosinophilic cytoplasm.
- Low NC ratio.[16]
- Layered dense collagen bundles.
DDx:
Note:
- If conventional HCC is seen focally within the tumour, it is conventional HCC.
Images
Sclerosing HCC
Features:
- Fibrosis. (???)
Notes:
- Seen in non-cirrhotic livers.
Grading
Edmondson-Steiner grading system:[17][18]
- Well-differentiated.
- Some say "it cannot be diagnosed on biopsy,"[19] as it cannot be reliably differentiated from a regenerative nodule.
- Moderately differentiated.
- Round, regular nuclei, some hyperchromatism, nucleoli present, increase NC ratio.
- Poor differentiated.
- Very prominent nucleoli, pronounced nuclear irregularity.
- Undifferentiated.
- Anaplastic giant cells.
Simplified description - based on MacSween:[18]
- Well-differentiated = cytologically near normal.
- Moderate = looks like a cancer, small nucleoli.
- Poor = bad cancer, raisin-like (irregular) nuclear membrane, large nucleoli (~1/3 of nucleus).
- Undifferentiated = death on a slide, huge cells (3-4x the size of other cells).
IHC
- CD34 +ve sinusoids; sinusoids in normal liver are CD34 -ve.
- HepPar-1 +ve; may be neg. in high grade tumours.
- AFP +ve; may be neg. even if the serum AFP is elevated.
- CK8/18 +ve.[20]
- Glypican-3 +ve (cytoplasmic, granular cytoplasmic or membranous).[21]
Bile canaliculi:
Image:
Sign out
Negative core biopsy
LIVER CORE, BIOPSY: - CIRRHOSIS. - HEPATOCYTE CYTOLOGY WITHIN NORMAL LIMITS.
See also
References
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 588. ISBN 978-0443066573.
- ↑ 2.0 2.1 2.2 2.3 http://emedicine.medscape.com/article/282814-overview
- ↑ 3.0 3.1 3.2 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 924. ISBN 0-7216-0187-1.
- ↑ Leong TY, Leong AS (2005). "Epidemiology and carcinogenesis of hepatocellular carcinoma". HPB (Oxford) 7 (1): 5–15. doi:10.1080/13651820410024021. PMC 2023917. PMID 18333156. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023917/.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 925. ISBN 0-7216-0187-1.
- ↑ Yusuf MA, Badar F, Meerza F, et al. (2007). "Survival from hepatocellular carcinoma at a cancer hospital in Pakistan". Asian Pac. J. Cancer Prev. 8 (2): 272–4. PMID 17696722.
- ↑ Sharieff S, Burney KA, Ahmad N, Salam A, Siddiqui T (October 2001). "Radiological features of hepatocellular carcinoma in Southern Pakistan". Trop Doct 31 (4): 224–5. PMID 11676064.
- ↑ Adapted from STC (19 Jan 2009).
- ↑ Kojiro, M.; Wanless, IR.; Alves, V.; Badve, S.; Balabaud, C.; Bedossa, P.; Bhathal, P.; Bioulac-Sage, P. et al. (Feb 2009). "Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia.". Hepatology 49 (2): 658-64. doi:10.1002/hep.22709. PMID 19177576. http://onlinelibrary.wiley.com/doi/10.1002/hep.22709/pdf.
- ↑ Adapted from STC (19 Jan 2009).
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 590-1. ISBN 978-0443066573.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 591. ISBN 978-0443066573.
- ↑ Walther, Z.; Jain, D. (2011). "Molecular pathology of hepatic neoplasms: classification and clinical significance.". Patholog Res Int 2011: 403929. doi:10.4061/2011/403929. PMC 3090128. PMID 21559202. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3090128/.
- ↑ 14.0 14.1 14.2 Stipa, F.; Yoon, SS.; Liau, KH.; Fong, Y.; Jarnagin, WR.; D'Angelica, M.; Abou-Alfa, G.; Blumgart, LH. et al. (Mar 2006). "Outcome of patients with fibrolamellar hepatocellular carcinoma.". Cancer 106 (6): 1331-8. doi:10.1002/cncr.21703. PMID 16475212.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 595-6. ISBN 978-0443066573.
- ↑ STC. 6 December 2010.
- ↑ Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. EDMONDSON HA, STEINER PE. Cancer. 1954 May;7(3):462-503. PMID 13160935.
- ↑ 18.0 18.1 Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 783. ISBN 978-0-443-10012-3.
- ↑ Pollet A. 28 May 2009.
- ↑ Stroescu, C.; Herlea, V.; Dragnea, A.; Popescu, I. (Mar 2006). "The diagnostic value of cytokeratins and carcinoembryonic antigen immunostaining in differentiating hepatocellular carcinomas from intrahepatic cholangiocarcinomas.". J Gastrointestin Liver Dis 15 (1): 9-14. PMID 16680226.
- ↑ Shirakawa, H.; Kuronuma, T.; Nishimura, Y.; Hasebe, T.; Nakano, M.; Gotohda, N.; Takahashi, S.; Nakagohri, T. et al. (Mar 2009). "Glypican-3 is a useful diagnostic marker for a component of hepatocellular carcinoma in human liver cancer.". Int J Oncol 34 (3): 649-56. PMID 19212669. http://www.spandidos-publications.com/serveFile/ijo_34_3_649_PDF.pdf?type=article&article_id=ijo_34_3_649&item=PDF.
- ↑ Shousha, S.; Gadir, F.; Peston, D.; Bansi, D.; Thillainaygam, AV.; Murray-Lyon, IM. (Oct 2004). "CD10 immunostaining of bile canaliculi in liver biopsies: change of staining pattern with the development of cirrhosis.". Histopathology 45 (4): 335-42. doi:10.1111/j.1365-2559.2004.01927.x. PMID 15469471.
- ↑ Porcell, AI.; De Young, BR.; Proca, DM.; Frankel, WL. (Jul 2000). "Immunohistochemical analysis of hepatocellular and adenocarcinoma in the liver: MOC31 compares favorably with other putative markers.". Mod Pathol 13 (7): 773-8. PMID 10912937.
- ↑ Goodman, ZD. (Feb 2007). "Neoplasms of the liver.". Mod Pathol 20 Suppl 1: S49-60. doi:10.1038/modpathol.3800682. PMID 17486052.