High-grade prostatic intraepithelial neoplasia
Jump to navigation
Jump to search
| High-grade prostatic intraepithelial neoplasia | |
|---|---|
| Diagnosis in short | |
 High-grade prostatic intraepithelial neoplasia. H&E stain. | |
|
| |
| Synonyms | prostatic intraepithelial neoplasia |
|
| |
| LM | nuclear changes (hyperchromatic nuclei, nucleoli present, +/-increased NC ratio, mild-to-moderate nuclear enlargement), medium-to-large glands with the architecture of HGPIN (tufted, micropapillary, cribriform, flat) |
| LM DDx | basal cell hyperplasia, prostatic adenocarcinoma, PIN-like prostatic ductal adenocarcinoma, atypical small acinar proliferation (biopsy only) |
| IHC | AMACR +ve, basal cells present (p63 +ve, CK34betaE12 +ve) |
| Gross | not evident |
| Site | prostate gland |
|
| |
| Associated Dx | prostate adenocarcinoma |
| Signs | none |
| Symptoms | none |
| Prevalence | common |
| Blood work | +/-PSA elevated |
| Radiology | not identifiable |
| Prognosis | benign |
| Clin. DDx | prostate carcinoma |
| Treatment | follow-up +/-re-biopsy |
High-grade prostatic intraepithelial neoplasia, abbreviated as HGPIN, is considered the precursor for prostate carcinoma.
It may be referred to as prostatic intraepithelial neoplasia, abbreviated PIN.
General
- Thought to be a precursor lesion for prostate adenocarcinoma.
- Incidence ~5-8% on core biopsy.[1]
- Multifocal HGPIN considered a risk for prostate cancer on re-biopsy.[2][3]
- A small focus of HGPIN does not appear to be associated with an increased risk for prostate cancer on re-biopsy at one year if the initial biopsy had 8 or more cores.[4]
Low-grade prostatic intraepithelial neoplasia:
- Should not be reported.[1]
- Believed to be irrelevant biologically/clinically.
- PIN not otherwise specified refers to HGPIN.
- Low-grade PIN has the architecture of HGPIN but lacks the nuclear atypia.
HGPIN and cancer on follow-up biopsy
Prostate cancer on follow-up biopsy by number of HGPIN sites from Merrimen et al.:[3]
| Number of cores with HGPIN |
Odds ratio of cancer on follow-up (95% CI) |
|---|---|
| 0 | 1.00 (reference) |
| 1 | 1.02 (0.73-1.40) |
| 2 | 1.55 (1.08-2.21) |
| 3 | 1.99 (1.16-3.40) |
| 4 | 2.66 (1.10-6.40) |
Gross
- Not evident on gross.
Microscopic
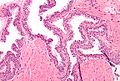
- Medium to large glands with architectural changes - see HGPIN architecture below.
- Described as "epithelial hyperplasia".
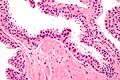
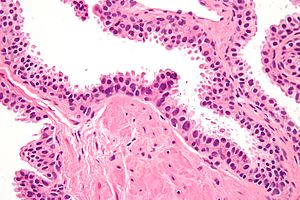
- Diagnosed on basis of nuclear changes.
- Hyperchromatic nuclei - key (low power) feature.
- Nucleoli present - key (high power) feature.
- Often increased NC ratio.
- Nuclear enlargement.
Notes:
- Nucleoli should be visible with the 20x objective.
- If one uses the 40x objective... one over calls.
- May need IHC for cancer versus HGPIN.
- Nucleoli should be present in >= 10% of cells in a gland to call it HGPIN.[7]
- This criterium is not required by all pathologists.
DDx:
- Basal cell hyperplasia of the prostate.
- Intraductal carcinoma of the prostate.
- Prostatic adenocarcinoma - glands with HGPIN have two or more distinct cells layers.
- PIN-like prostatic ductal adenocarcinoma - glands crowded.
- Benign prostate - HPGIN has nuclear changes.
HGPIN architecture
There are several forms:[8][9]
- Flat - uncommon.
- Tufting - common.
- Micropapillary - common.
- Cribriform - rare.
Note:
- The architectural pattern is not thought to have any prognostic significance; however, it may be useful for differentiating it from benign prostate.
Images
IHC
- HGPIN: AMACR +ve, p63 +ve, HMWCK +ve.
- Cancer: AMACR +ve, p63 -ve, HMWCK -ve.
- Normal: AMACR -ve, p63 +ve, HMWCK +ve.
Sign out
A. PROSTATE, RIGHT LATERAL SUPERIOR, BIOPSY: - HIGH-GRADE PROSTATIC INTRAEPITHELIAL NEOPLASIA; - NEGATIVE FOR MALIGNANCY.
If there is (isolated) HGPIN in more than 3 or 4 cores:
COMMENT: As high-grade prostatic intraepithelial neoplasia is found in multiple cores, close follow-up is suggested, with a re-biopsy when indicated.
See also
References
- ↑ 1.0 1.1 Epstein, JI.; Herawi, M. (Mar 2006). "Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications for patient care.". J Urol 175 (3 Pt 1): 820-34. doi:10.1016/S0022-5347(05)00337-X. PMID 16469560.
- ↑ Srigley, JR.; Merrimen, JL.; Jones, G.; Jamal, M. (Dec 2010). "Multifocal high-grade prostatic intraepithelial neoplasia is still a significant risk factor for adenocarcinoma.". Can Urol Assoc J 4 (6): 434. PMID 21191509.
- ↑ 3.0 3.1 Merrimen, JL.; Jones, G.; Walker, D.; Leung, CS.; Kapusta, LR.; Srigley, JR. (Aug 2009). "Multifocal high grade prostatic intraepithelial neoplasia is a significant risk factor for prostatic adenocarcinoma.". J Urol 182 (2): 485-90; discussion 490. doi:10.1016/j.juro.2009.04.016. PMID 19524976.
- ↑ Herawi, M.; Kahane, H.; Cavallo, C.; Epstein, JI. (Jan 2006). "Risk of prostate cancer on first re-biopsy within 1 year following a diagnosis of high grade prostatic intraepithelial neoplasia is related to the number of cores sampled.". J Urol 175 (1): 121-4. doi:10.1016/S0022-5347(05)00064-9. PMID 16406886.
- ↑ Amin, Mahul B. (2010). Diagnostic Pathology: Genitourinary (1st ed.). Amirsys. pp. 3-56. ISBN 978-1931884280.
- ↑ Chin, AI.; Dave, DS.; Rajfer, J. (2007). "Is repeat biopsy for isolated high-grade prostatic intraepithelial neoplasia necessary?". Rev Urol 9 (3): 124-31. PMC 2002502. PMID 17934569. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2002502/.
- ↑ Amin, Mahul B. (2010). Diagnostic Pathology: Genitourinary (1st ed.). Amirsys. pp. 3-55. ISBN 978-1931884280.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 380. ISBN 978-0781765275.
- ↑ Bostwick, DG.; Qian, J. (Mar 2004). "High-grade prostatic intraepithelial neoplasia.". Mod Pathol 17 (3): 360-79. doi:10.1038/modpathol.3800053. PMID 14739906. http://www.nature.com/modpathol/journal/v17/n3/pdf/3800053a.pdf.