Medical liver disease
This article deals with medical liver disease. An introduction to the liver and approach is found in the liver article.
Every differential in liver pathology has "drugs"[1] -- if it isn't clearly malignancy.
Liver neoplasms are dealt with in the liver neoplasms article.
Review of liver blood work
Inflammation activity
- ALT.
- AST.
Cholestatic markers
- ALP.
- GGT - used to assess whether the ALP is an "honest" value, elevated in cirrhosis.
Cirrhosis/decompensation
- PLT - low is suggestive of dysfunction.
- INR - high is bad, unless anticoagulated.
Other
- Bilirubin.
- Direct (AKA conjugated).
- Indirect (AKA unconjugated).
A short DDx of elevated:[2]
- Indirect:
- Gilbert syndrome.
- Crigler-Najjar syndrome type 1.
- Crigler-Najjar syndrome type 2.
- Direct:
- Rotor syndrome.
- Dubin-Johnson syndomre.
Viral hepatitis
- HBV DNA.
- HCV RNA.
- HBs Ag, HBs Ab, HBe Ag, HBe Ab.
- HCV Ab.
Others:
- Epstein-Barr virus (EBV).
- Cytomegalovirus (CMV) - especially in the immune incompetent.
Hepatitis B
Meaning & utility of the various Hepatitis B tests:[3][4]
| Test name | Location | Positive test | Negative test | Usual question |
|---|---|---|---|---|
| HBs Ag | Surface | Virus active | No active infection | Active infection? |
| HBs Ab | Surface | Exposed OR vaccinated | No exposure OR no vaccine OR loss of Ab | Immunization status? |
| HBe Ag | Virus core | Infect. w/ viral replication | No active infection | Active infect. w/ viral replication? |
| HBe Ab | Virus core | Exposed to virus | Infect. w/o antibody response OR not exposed | Immune response to infection? |
| HBV DNA | - | Active | Not active/no exposure | Viral load/how active? |
| HBc Ab | Virus core | Virus active/previous exposure | No exposure | Early active infection? |
Notes:
- HBc Ab may test for acute (IgM) or chronic infection - dependent on specific antibody test; it is often used to look for early infection.[4]
- Carriers of hepatitis B: HBs Ag +ve, HBs Ab -ve, HBc Ag -ve, HBc Ab +ve, HBe Ag -ve, HBe Ab +ve.[5]
Markers for rare liver diseases
- Ceruloplasm - low think Wilson's disease; typical value for Wilson's ~ 0.12 g/L.
- <0.20 g/L is a criteria for Wilson's disease.[6]
- Alpha-1 antitrypsin - if low think deficiency.
Hemosiderosis
- Ferritin - high.
- Iron saturation - high.
Causes:
- Hemochromatosis.
- Hemolysis, chronic.
- Cirrhosis.
Medical imaging
Blood flow:[7]
- Hepatopedal flow = normal portal vein flow.
- Hepatofugal flow = reversed portal vein flow.
Interventional measurements
Wedged to free hepatic venous pressure:[8]
- Normal = 1-4 mmHg.
- Elevated in portal hypertension.
Liver biopsy
Medical liver biopsy adequacy
Liver biopsy specimens should be:[9]
- 2.0 cm in length and contain 11-15 portal tracts,
- The core should be deeper than 1.0 cm from the liver capsule; specimens close to the capsule may lead to over grading of fibrosis.
Reporting
Specimen, procedure: - Diagnosis.
The diagnosis usually contains grading and staging information, e.g. activity 2 /4, Laennec fibrosis stage 1 /4.
In the context of medical liver disease:
- Grade = inflammation/activity.
- Stage = severity of fibrosis/architectural changes.
Notes:
- The term "acute" is infrequently used in liver pathology.
- In the liver: neutrophils is not acute -- unlike most elsewhere in the body.[10]
A microscopic checklist
Size of biopsy: Adequate Fragmentation: Absent Fibrosis: Stage 2-3/4, mostly stage 2 Fibrous septa: Present Septa with curved contours: Present – focally only Large droplet steatosis (% of hepatocytes): Present, moderate 60% Ballooning of hepatocytes: Present, rare Mallory-Denk bodies: Present, rare Portal inflammation: Present Interface activity: Minimal (0-1/4) Lobular necroinflammation: Minimal Ducts: Present in normal numbers Duct injury: Absent Ductular reaction: Absent Cholestasis: Absent Terminal hepatic venules: Present Iron stain: Absent Ground glass cells with routine stains: Absent PASD for alpha-1 antitrypsin droplets: Negative
Viral hepatitis
These are common. The diagnoses are based on serology. The serology is covered in the viral hepatitis section in the liver pathology article.
Typically classified as:[11][12]
- Acute < 6 months duration.
- Chronic > 6 months duration.
Hepatitis A
- Infection is self-limited, i.e. not persistent.
- May present as fulminant hepatic necrosis.
- Usually asymptomatic in children.[13]
- Serology is diagnostic.
Hepatitis B
- Hepatitis B virus, abbreviated HBV, redirects here.
General
- May lead to hepatocellular carcinoma without cirrhosis.
- High prevalence.
- Diagnosis is by serology.
- A vaccination is available and done routinely in a many jurisdictions.[14]
Associated pathology:
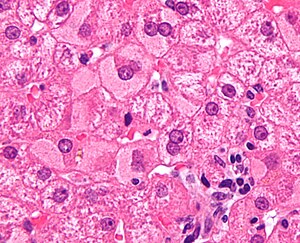
Microscopic
Features:
- Lobular inflammation - this is non-specific finding.
- Hepatocyte necrosis:
- Necrotic hepatocytes look a lot like neutrophils - however:
- Cytoplasm is more pink.
- Round apoptotic bodies.
- Necrotic hepatocytes look a lot like neutrophils - however:
- Hepatocyte necrosis:
- Ground glass hepatocytes - see liver pathology article.
DDx:
Image
IHC
- Hepatitis B +ve.
Hepatitis C
General
- Leads to hepatocellular carcinoma in the setting of cirrhosis.
- Tends to be chronic; the "C" in "hepatitis C" stands for chronic.
- Diagnosis is by serology.
Associated pathology:
Microscopic
Features:
- Lobular inflammation - this is non-specific finding.
- Usually Grade 1, rarely Grade 2 and almost never Grade 3 or Grade 4.[15]
- Periportal steatosis in genotype 3.[16]
- Steatosis in hepatitis C is usually a secondary pathology, i.e. a separate pathologic process.[17]
DDx:
- Hepatitis B (without ground glass hepatocytes).
- Autoimmune hepatitis.
- Primary biliary cirrhosis without granulomas.
- Drug reaction.
Other infections
- Hydatid disease (Hydatid cyst).
- Ascaris.
- Fasciola
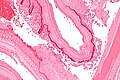
Hydatid disease
- AKA hydatid cyst.
General
- Etiology: Echinococcus.
Microscopic
Features:
- Laminated wall +/- calcification.[18]
- Organisms -- see Echinococcus.
Images
www:
Metabolic and toxic
Alcoholic liver disease
General
- Acute and/or chronic liver changes due to excessive alcohol use - includes:
Classic lab findings in EtOH abusers
- AST & ALT elevated with AST:ALT=2:1.
- GGT elevated.
- MCV increased.
Gross pathology/radiologic findings
- Classically micronodular pattern.
- May be macronodular.
Microscopic
See:
- Steatohepatitis section and ballooning degeneration section.
Features:
- Often zone III damage.
- Cholestatsis common, i.e. yellow staining.
- NASH (non-alcoholic steatohepatitis) usu. does not have cholestasis.[21]
- Fibrosis starts at central veins.
- Neutrophils (often helpful) -- few other things have PMNs. (???)
- Neutrophils cluster around cells with Mallory hyaline.
Notes:
- If portal inflammatory infiltrates more than mild, r/o other causes i.e. viral hepatitis.
- Mallory bodies once thought to be characteristic; now considered non-specific and generally poorly understood.[22]
- Some consider alcoholic liver disease a clinical diagnosis, i.e. as a pathologist one does not diagnose it.[23]
Non-alcoholic fatty liver disease
- Abbreviated NAFLD.
- Fatty liver that is not due to alcohol; includes obesity-related fatty liver, metabolic disease/diabetes-related fatty liver.
NASH
- Non-alcoholic steatohepatitis - see steatohepatitis section.
- Histologically indistinguishable from ASH.
- NASH is a clinical diagnosis based on exclusion of alcohol.
Steatohepatitis
Autoimmune
Autoimmune hepatitis
- Abbreviated AIH.
Primary biliary cirrhosis
- Abbreviated PBC.
Autoimmune hepatitis-primary biliary cirrhosis overlap syndrome
- Abbreviation AIH-PBC OS.
General
Epidemiology:
- Rare.
Serology:[24]
- AMA +ve.
- Anti-dsDNA +ve.
Microscopic
Primary sclerosing cholangitis
- Abbreviated PSC.
Hereditary
Caroli disease
General
- Genetic disease.
- Frequently associated with autosomal recessive polycystic kidney disease (ARPKD).[25]
- May be seen in isolation.[26]
Clinical:[27]
- Recurrent cholangitis.
- Recurrent cholelithiasis.
- Cholangiocarcinoma[28] - seen in ~7% of cases.[29]
Note:
- Caroli syndrome = Caroli disease + congenital hepatic fibrosis.[30]
Gross
- Dilated bile ducts.[25]
Microscopic
Features:[27]
- Dilated bile ducts.
- Periductal fibrosis. (???)
- +/-Fibrosis.
Image:
Hereditary hemochromatosis
- For secondary causes see secondary hemochromatosis.
Wilson disease
Alpha-1 antitrypsin deficiency
- AKA alpha1-antiprotease inhibitor deficiency.
Other
Budd-Chiari syndrome
- AKA hepatic vein obstruction.
General
- Hepatic outflow obstruction.
Clinical triad:[32]
- Ascites.
- Abdominal pain.
- Hepatomegaly.
Etiology:
- ~50% have a myeloproliferative disease.[33]
- May be due to mass effect from a tumour.
Clinical DDx:
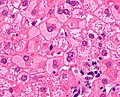
Microscopic
Features:[34]
- Sinusoidal dilation in zone III (congestion).
- +/-Hepatocyte drop-out.
- +/-Centrilobular fibrosis.
DDx congestion:
- Congestive heart failure (congestive hepatopathy).
- Constrictive pericarditis.
Vanishing bile duct syndrome
General
- Fatal.
DDx:[36]
- Primary biliary cirrhosis.
- Primary sclerosing cholangitis.
- GVHD.[37]
- Drugs.[38]
- Chronic rejection.[35]
Microscopic
Features:[36]
- Loss of intrahepatitic bile ducts - key feature.
- Cholestasis.
Note:
- May occur without fibrosis and inflammation; thus, can be easy to miss.
IHC
- CK7 -ve.
- Marks bile ducts.
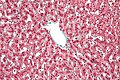
Congestive hepatopathy
General
- Liver failure due to (right) heart failure.
- AKA cardiac cirrhosis - a term used by clinicians.
- Generally, it does not satisfy pathologic criteria for cirrhosis.[39]
Gross
- "Nutmeg" liver - yellow spotted appearance.
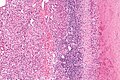
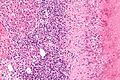
Microscopic
Features:[40]
- Zone III atrophy.
- Portal venule (central vein) distension.
- Perisinusoidal fibrosis - progresses to centrilobular fibrosis and then diffuse fibrosis.
- Dilation of sinusoids in all zone III areas - key feature.[41]
DDx:
- Hemangioma of the liver - should be focal lesion.
Images
Drug-induced liver disease
- AKA drug-induced liver toxicity.
Focal nodular hyperplasia
- Abbreviated FNH.
Nodular regenerative hyperplasia
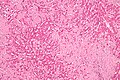
General
- Associated with renal transplants, bone marrow transplants and vasculitides.[42]
- Can lead to portal hypertension and many of the associated complications.[43]
Etiology
- Arterial hypervascularity secondary to loss of hepatic vein radicles (loss of central venule in hepatic lobule).[42]
ASIDE: radicle = ramulus - smallest branch or vessel or nerve.[44]
Gross
- Diffuse nodularity - whole liver.
Microscopic
Features:[42]
- "Plump" hepatocytes surrounded by atrophic ones.
- No fibrosis.
Sinuosoidal obstruction syndrome
- May be referred to as Hepatic veno-occlusive disease.[45]
General
Clinical DDx:
Microscopic
Features:[34]
- Subendothelial swelling in hepatic venules.
Negatives:
- No thrombosis.
Polycystic kidney disease and the liver
General
Complications of PKD in the liver:[47]
- Infected cyst.
- Cholangiocarcinoma.
- Cholestasis/obstruction due to duct compression.[48]
Cysts:
- Cysts in the liver, like the kidney, are thought to enlarge with age.
Microscopic
Features:[49]
- Von Meyenburg complexes (bile duct hamartoma):
- Cluster of dilated ducts with "altered" bile.
- Surrounded by collagenous stroma.
- Separate from the portal areas.[50]
Images:
Notes:
Peliosis hepatis
General
- Associated with:
- Infections.
- Malignancy.
- Other stuff.
- Rarely biopsied.
Microscopic
Features:
- Cyst lined by endothelium.
- Usu. incomplete.
- Blood.
Total parenteral nutrition
- Abbreviated TPN.
General
- Indication: short gut syndrome, others.
Microscopic
Variable - may range from: steatosis, steatohepatitis, cholestasis, fibrosis and cirrhosis.[53]
- Steatosis (periportal) - early.
- Cholestasis - late.
Giant cell hepatitis
- AKA neonatal giant cell hepatitis.
- See: Giant cell hepatitis.
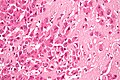
Hepatic amyloidosis
General
- Diffuse abundant amyloid within the space of Disse is associated with portal hypertension.[8]
Microscopic
Features:
- Amorphous extracellular pink stuff on H&E - see amyloid article.
DDx:
Images
Stains
- Congo red +ve.
Fulminant hepatic necrosis
General
Etiology:
- Viral, i.e. Hepatitis A, Hepatitis B; Hepatitis C - extremely rare.
- Trauma.
- Shock.
Microscopic
Features:
- Hepatocyte necrosis.
- Bile duct proliferation.
DDx:
Secondary hemochromatosis
- For the hereditary one see hereditary hemochromatosis.
General
- Iron overload secondary to blood transfusions for hereditary or acquired anemia.[56]
- Primary hemochromatosis due to a defect in iron processing - called hereditary hemochromatosis.
- Imaging considered the best test, as iron deposition is patchy.[56]
Selected hereditary causes:[56]
- Thalassemia.
- Sickle cell anemia.
- Hereditary sideroblastic anemia.
Selected acquired causes:[56]
- Myelodysplastic syndromes
- Myelofibrosis
- Aplastic anemia, intractable.
Microscopic
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 441. ISBN 978-1416054542.
- ↑ URL: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/hepatology/hepatitis-B/. Accessed on: 16 May 2011.
- ↑ 4.0 4.1 URL: http://www.labtestsonline.org/understanding/analytes/hepatitis_b/test.html. Accessed on: 16 May 2011.
- ↑ URL: http://labtestsonline.org/understanding/analytes/hepatitis-b/tab/test. Accessed on: 3 May 2012.
- ↑ Diagnostic accuracy of serum ceruloplasmin in Wilson disease: determination of sensitivity and specificity by ROC curve analysis among ATP7B-genotyped subjects. Mak CM, Lam CW, Tam S. Clin Chem. 2008 Aug;54(8):1356-62. Epub 2008 Jun 12. PMID 18556333. URL: http://www.clinchem.org/cgi/reprint/54/8/1356.pdf. Accessed on: 28 September 2009.
- ↑ URL: http://insidesurgery.com/2010/12/hepatopedal-hepatofugal-flow/. Accessed on: 2 December 2011.
- ↑ 8.0 8.1 Bion, E.; Brenard, R.; Pariente, EA.; Lebrec, D.; Degott, C.; Maitre, F.; Benhamou, JP. (Feb 1991). "Sinusoidal portal hypertension in hepatic amyloidosis.". Gut 32 (2): 227-30. PMC 1378815. PMID 1864548. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1378815/.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 418. ISBN 978-0-443-10012-3.
- ↑ OA. September 2009.
- ↑ "Terminology of chronic hepatitis, hepatic allograft rejection, and nodular lesions of the liver: summary of recommendations developed by an international working party, supported by the World Congresses of Gastroenterology, Los Angeles, 1994.". Am J Gastroenterol 89 (8 Suppl): S177-81. Aug 1994. PMID 8048409.
- ↑ URL: http://familydoctor.org/familydoctor/en/diseases-conditions/hepatitis-b.html. Accessed on: 2 May 2012.
- ↑ Jeong SH, Lee HS (2010). "Hepatitis A: clinical manifestations and management". Intervirology 53 (1): 15–9. doi:10.1159/000252779. PMID 20068336.
- ↑ Leuridan, E.; Van Damme, P. (Jul 2011). "Hepatitis B and the need for a booster dose.". Clin Infect Dis 53 (1): 68-75. doi:10.1093/cid/cir270. PMID 21653306.
- ↑ STC. 6 December 2010.
- ↑ Yoon EJ, Hu KQ. Hepatitis C virus (HCV) infection and hepatic steatosis. Int J Med Sci. 2006;3(2):53-6. Epub 2006 Apr 1. PMID 16614743. Avialable at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1415843. Accessed on: September 9, 2009.
- ↑ OA. September 2009.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ URL: http://emedicine.medscape.com/article/170539-overview. Accessed on: 3 May 2012.
- ↑ STC. 6 December 2010.
- ↑ STC. 6 December 2010.
- ↑ Jensen K, Gluud C (November 1994). "The Mallory body: theories on development and pathological significance (Part 2 of a literature survey)". Hepatology 20 (5): 1330-42. PMID 7927269.
- ↑ MG. September 2009.
- ↑ Muratori, P.; Granito, A.; Pappas, G.; Pendino, GM.; Quarneti, C.; Cicola, R.; Menichella, R.; Ferri, S. et al. (Jun 2009). "The serological profile of the autoimmune hepatitis/primary biliary cirrhosis overlap syndrome.". Am J Gastroenterol 104 (6): 1420-5. doi:10.1038/ajg.2009.126. PMID 19491855.
- ↑ 25.0 25.1 Online 'Mendelian Inheritance in Man' (OMIM) 263200
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 600643
- ↑ 27.0 27.1 Yonem, O.; Bayraktar, Y. (Apr 2007). "Clinical characteristics of Caroli's syndrome.". World J Gastroenterol 13 (13): 1934-7. PMID 17461493.
- ↑ Yonem, O.; Bayraktar, Y. (Apr 2007). "Clinical characteristics of Caroli's disease.". World J Gastroenterol 13 (13): 1930-3. PMID 17461492.
- ↑ Karim, AS. (Aug 2004). "Caroli's disease.". Indian Pediatr 41 (8): 848-50. PMID 15347876.
- ↑ Brancatelli, G.; Federle, MP.; Vilgrain, V.; Vullierme, MP.; Marin, D.; Lagalla, R.. "Fibropolycystic liver disease: CT and MR imaging findings.". Radiographics 25 (3): 659-70. doi:10.1148/rg.253045114. PMID 15888616.
- ↑ URL: http://www.meddean.luc.edu/lumen/MedEd/orfpath/develop.htm. Accessed on: 1 December 2011.
- ↑ Fox, MA.; Fox, JA.; Davies, MH. (2011). "Budd-Chiari syndrome--a review of the diagnosis and management.". Acute Med 10 (1): 5-9. PMID 21573256.
- ↑ Plessier, A.; Valla, DC. (Aug 2008). "Budd-Chiari syndrome.". Semin Liver Dis 28 (3): 259-69. doi:10.1055/s-0028-1085094. PMID 18814079.
- ↑ 34.0 34.1 34.2 Aydinli, M.; Bayraktar, Y. (May 2007). "Budd-Chiari syndrome: etiology, pathogenesis and diagnosis.". World J Gastroenterol 13 (19): 2693-6. PMID 17569137. http://www.wjgnet.com/1007-9327/full/v13/i19/2693.htm.
- ↑ 35.0 35.1 Inomata, Y.; Tanaka, K. (2001). "Pathogenesis and treatment of bile duct loss after liver transplantation.". J Hepatobiliary Pancreat Surg 8 (4): 316-22. doi:10.1007/s0053410080316. PMID 11521176.
- ↑ 36.0 36.1 Reau, NS.; Jensen, DM. (Feb 2008). "Vanishing bile duct syndrome.". Clin Liver Dis 12 (1): 203-17, x. doi:10.1016/j.cld.2007.11.007. PMID 18242505.
- ↑ Yeh, KH.; Hsieh, HC.; Tang, JL.; Lin, MT.; Yang, CH.; Chen, YC. (Aug 1994). "Severe isolated acute hepatic graft-versus-host disease with vanishing bile duct syndrome.". Bone Marrow Transplant 14 (2): 319-21. PMID 7994249.
- ↑ Chitturi, S.; Farrell, GC. (Apr 2001). "Drug-induced cholestasis.". Semin Gastrointest Dis 12 (2): 113-24. PMID 11352118.
- ↑ URL: http://emedicine.medscape.com/article/151792-overview. Accessed on: 17 June 2010.
- ↑ URL: http://emedicine.medscape.com/article/151792-diagnosis. Accessed on: 17 June 2010.
- ↑ Suggested by OA. September 2009.
- ↑ 42.0 42.1 42.2 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 922. ISBN 0-7216-0187-1.
- ↑ Bissonnette, J.; Généreux, A.; Côté, J.; Nguyen, B.; Perreault, P.; Bouchard, L.; Pomier-Layrargues, G. (Aug 2012). "Hepatic hemodynamics in 24 patients with nodular regenerative hyperplasia and symptomatic portal hypertension.". J Gastroenterol Hepatol 27 (8): 1336-40. doi:10.1111/j.1440-1746.2012.07168.x. PMID 22554152.
- ↑ Dorland's Medical Dictionary. 30th Ed.
- ↑ DeLeve, LD.; Shulman, HM.; McDonald, GB. (Feb 2002). "Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease).". Semin Liver Dis 22 (1): 27-42. doi:10.1055/s-2002-23204. PMID 11928077..
- ↑ Helmy, A. (Jan 2006). "Review article: updates in the pathogenesis and therapy of hepatic sinusoidal obstruction syndrome.". Aliment Pharmacol Ther 23 (1): 11-25. doi:10.1111/j.1365-2036.2006.02742.x. PMID 16393276.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 174-5. ISBN 978-0-443-10012-3.
- ↑ URL: http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=9184868. Accessed on: 23 September 2009.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 176. ISBN 978-0-443-10012-3.
- ↑ Meyenburg complex. Stedman's Medical Dictionary. 27th Ed.
- ↑ Bile duct hamartomas--the von Meyenburg complex. Salles VJ, Marotta A, Netto JM, Speranzini MB, Martins MR. Hepatobiliary Pancreat Dis Int. 2007 Feb;6(1):108-9. PMID 17287178.
- ↑ [The von Meyenburg complex] Schwab SA, Bautz W, Uder M, Kuefner MA. Rontgenpraxis. 2008;56(6):241-4. German. PMID 19294869.
- ↑ Guglielmi FW, Boggio-Bertinet D, Federico A, et al. (September 2006). "Total parenteral nutrition-related gastroenterological complications". Dig Liver Dis 38 (9): 623–42. doi:10.1016/j.dld.2006.04.002. PMID 16766237.
- ↑ Li, SJ.; Nussbaum, MS.; McFadden, DW.; Gapen, CL.; Dayal, R.; Fischer, JE. (Aug 1988). "Addition of glucagon to total parenteral nutrition (TPN) prevents hepatic steatosis in rats.". Surgery 104 (2): 350-7. PMID 3135627.
- ↑ Stanko, RT.; Nathan, G.; Mendelow, H.; Adibi, SA. (Jan 1987). "Development of hepatic cholestasis and fibrosis in patients with massive loss of intestine supported by prolonged parenteral nutrition.". Gastroenterology 92 (1): 197-202. PMID 3096806.
- ↑ 56.0 56.1 56.2 56.3 Gattermann, N. (Jul 2009). "The treatment of secondary hemochromatosis.". Dtsch Arztebl Int 106 (30): 499-504, I. doi:10.3238/arztebl.2009.0499. PMC 2735704. PMID 19727383. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2735704/.