Fibroadenoma
| Fibroadenoma | |
|---|---|
| Diagnosis in short | |
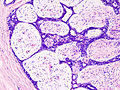
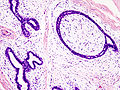
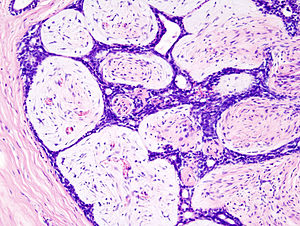 Fibroadenoma. H&E stain. | |
|
| |
| LM | abundant (intralobular) stroma usu. white/pale +/-hyalinization, typically paucicellular, compression of glandular elements with perserved myoepithelial cells |
| Subtypes | juvenile, complex, myxoid, cellular, tubular adenoma of the breast |
| LM DDx | phyllodes tumour, sarcoma, pseudoangiomatous stromal hyperplasia, adenomyoepithelioma for tubular adenoma of the breast |
| Gross | well-circumscribed, rubbery, tan/white, +/-lobulated appearance, +/-short slit-like spaces, +/-calcifications |
| Site | breast |
|
| |
| Prevalence | very common |
| Prognosis | benign |
| Clin. DDx | other breast tumours - esp. phyllodes tumour |
| Treatment | conservative excision |
Fibroadenoma is a common benign tumour of the breast.
General
- Very common benign finding.
- The pathology is in the stroma; so, the lesion is really a misnomer by the naming rules.
- It ought to be called adenofibroma (as a few occasionally do[1]), as the glandular component is benign and the stromal component lesional; there is no truth in names in pathology.
Management:
- Local excision -- without a large margin.
Gross
Features:[2]
- Well-circumscribed.
- Rubbery - classic descriptor.
- Tan/white.
- +/-Lobulated appearance.
- +/-Slit-like spaces - short.
- +/-Calcification.
Images
- Fibroadenoma - slit-like spaces (webpathology.com).
- Fibroadenoma - lobulated appearance (webpathology.com).
- Fibroadenoma (surgical-tutor.org).
Microscopic
Features:[3]
- Abundant (intralobular) stroma - most key feature.
- Stroma is usually:
- White/pale, i.e. myxoid, on H&E (normal stroma is pink).
- May be hyalinized (dark pink) if infarcted.
- Paucicellular - typical.
- White/pale, i.e. myxoid, on H&E (normal stroma is pink).
- Stroma is usually:
- Compression of glandular elements - very commonly seen.
- Glandular elements have at least two cell layers - epithelial and myoepithelial.
Notes:
- There is stuff about intracanalicular vs. pericanalicular.[4] It is irrelevant; there is no prognostic difference between the two.
- Do not comment on the margin - it is irrelevant.
DDx:
- Phyllodes tumour - long slit-like spaces (seen grossly), stroma is more cellular.
- +/-Mitoses,
- +/-"Stromal overgrowth" = large area where there is a 'loss of glands'.
- Sarcoma.
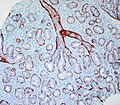
- Pseudoangiomatous stromal hyperplasia.
- Small capillary-like structures in the stroma.
- Epithelial component often not compressed - as in fibroadenoma.
- Small capillary-like structures in the stroma.
- Adenomyoepithelioma - for tubular adenoma of the breast.
Images
www:
Variants
Four variants are described by the Washington Manual:[7]
- Juvenile.
- Complex.
- Myxoid.
- Cellular.
Considered a variant of fibroadenoma by many authorities:[8]
Juvenile fibroadenoma
- As the name suggests, is typically found in younger patients.
- Classic history: rapid growth.
Features (juvenile variant):[9]
- Stromal and epithelial hyperplasia - key feature.
- +/-Tapering, thin micropapillae (gynecomastoid hyperplasia).[8]
- Mitoses uncommon.
Myxoid fibroadenoma
- May be associated with Carney's complex.
Features:
Cellular fibroadenoma
Features (cellular variant):
- Cellular.
- Mitoses.
Complex fibroadenoma
- Contain proliferative epithelium which outside and inside a fibroadenoma is associated with an increased risk of malignancy.
Features:[10]
- Apocrine metaplasia.
- Cysts > 3 mm.
- Calcification.
- Sclerosing adenosis.
Memory devices:
- FACS: complex fibroadenoma, apocrine metaplasia, calcs & cysts, sclerosing adenosis.
- CAMS: calcs, apocrine metaplasia, microcysts, sclerosing adenosis.
Tubular adenoma of the breast
- Considered by many a variant of fibroadenoma.
Features:[8]
- Fibromyxoid stroma (like in a fibroadenoma).
- Small round glands.
Images:
Sign out
Right Breast, Lumpectomy: - Complex fibroadenoma with apocrine metaplasia. - Negative for carcinoma in situ and negative for malignancy.
See also
References
- ↑ Guinebretière, JM.; Menet, E.; Tardivon, A.; Cherel, P.; Vanel, D. (Apr 2005). "Normal and pathological breast, the histological basis.". Eur J Radiol 54 (1): 6-14. doi:10.1016/j.ejrad.2004.11.020. PMID 15797289.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 550. ISBN 978-1416054542.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 110. ISBN 978-0443066801.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970216-9. Accessed on: 16 March 2011.
- ↑ Sabate, JM.; Clotet, M.; Torrubia, S.; Gomez, A.; Guerrero, R.; de las Heras, P.; Lerma, E. (Oct 2007). "Radiologic evaluation of breast disorders related to pregnancy and lactation.". Radiographics 27 Suppl 1: S101-24. doi:10.1148/rg.27si075505. PMID 18180221.
- ↑ URL: http://www.imagingpathways.health.wa.gov.au/includes/dipmenu/image/image.html. Accessed on: 15 February 2012.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 262. ISBN 978-0781765275.
- ↑ 8.0 8.1 8.2 O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 116. ISBN 978-0443066801.
- ↑ URL: http://www.breastpathology.info/fibro_variants.html#juvenile. Accessed on: 3 October 2011.
- ↑ URL: http://www.breastpathology.info/fibro_variants.html#complex. Accessed on: 3 October 2011.
- ↑ Maiorano, E.; Albrizio, M. (Dec 1995). "Tubular adenoma of the breast: an immunohistochemical study of ten cases.". Pathol Res Pract 191 (12): 1222-30. PMID 8927570.