Difference between revisions of "Parathyroid hyperplasia"
Jump to navigation
Jump to search
(→Microscopic: tweak) |
|||
| Line 47: | Line 47: | ||
**Increased parenchymal cells. | **Increased parenchymal cells. | ||
***Chief cells - usually predominant.<ref name=pmid8090603/> | ***Chief cells - usually predominant.<ref name=pmid8090603/> | ||
***"Water-clear" cells - may not be apparent: | ***"Water-clear" cells - may not be apparent: | ||
****Abundant foamy or granular cytoplasm. | ****Abundant foamy or granular cytoplasm.<ref name=pmid7487410/> | ||
****Mild [[nuclear pleomorphism]]. | ****Mild [[nuclear pleomorphism]]. | ||
***Other parenchymal cells include: oxyphil cells and transitional oxyphil cells. | ***Other parenchymal cells include: oxyphil cells and transitional oxyphil cells. | ||
Revision as of 06:44, 26 February 2016
| Parathyroid hyperplasia | |
|---|---|
| Diagnosis in short | |
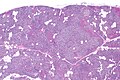
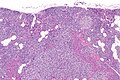
 Parathyroid hyperplasia. H&E stain. | |
|
| |
| LM | hypercellular - usu. chief cell predominant, decreased adipose tissue, +/-"water-clear" cells (cells with abundant granular/foamy cytoplasm, mild nuclear pleomorphism) |
| LM DDx | parathyroid adenoma, parathyroid carcinoma |
| Gross | all parathyroid glands are enlarged |
| Site | parathyroid gland |
|
| |
| Associated Dx | chronic renal failure |
| Syndromes | MEN 1, MEN 2A |
|
| |
| Prevalence | uncommon |
| Blood work | elevated PTH, +/-elevated calcium |
| Clin. DDx | parathyroid adenoma |
| Treatment | surgical removal of all parathyroid glands & re-implantation of half of one parathyroid in the forearm |
Parathyroid hyperplasia is an abnormal proliferation of the parathyroid glands and a relatively common cause of hyperparathyroidism that is typically associated with chronic renal failure.[1]
General
- Common cause of hyperparathyroidism.
- Usually associated with chronic renal failure.
- May be syndromic - chief cell hyperplasia - associated with MEN 1, MEN 2A.[2]
Gross
- Parathyroid gland enlargement - classically all parathyroid glands are involved; however, some may be spared making it difficult to differentiate this from parathyroid adenoma.[3]
Microscopic
Features:
- Hyperplastic/hypercellular appearance:
- Decreased adipose tissue.[4]
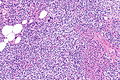
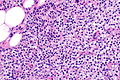
- Increased parenchymal cells.
- Chief cells - usually predominant.[4]
- "Water-clear" cells - may not be apparent:
- Abundant foamy or granular cytoplasm.[5]
- Mild nuclear pleomorphism.
- Other parenchymal cells include: oxyphil cells and transitional oxyphil cells.
Note:
- Generally, it is impossible to discern between parathyroid adenomas and parathyroid hyperplasias by histology alone.[6]
- One requires information of the size of the other glands to make the diagnosis.
- Water-clear cells may be seen in an adenoma.[5]
DDx:
- Parathyroid adenoma - classically have a rim of normal parathyroid gland around it.
- Parathyroid carcinoma - has invasive tissue destruction or far away metastases.
Images
Sign out
Clinical history is suggestive
A. Right Superior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. B. Right Inferior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. C. Portion of Left Inferior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. D. Left Superior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia.
See also
References
- ↑ Jamal, SA.; Miller, PD.. "Secondary and tertiary hyperparathyroidism.". J Clin Densitom 16 (1): 64-8. doi:10.1016/j.jocd.2012.11.012. PMID 23267748.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2. Accessed on: 29 July 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1128. ISBN 978-1416031215.
- ↑ 4.0 4.1 Yong, JL.; Vrga, L.; Warren, BA. (Apr 1994). "A study of parathyroid hyperplasia in chronic renal failure.". Pathology 26 (2): 99-109. PMID 8090603.
- ↑ 5.0 5.1 Grenko, RT.; Anderson, KM.; Kauffman, G.; Abt, AB. (Nov 1995). "Water-clear cell adenoma of the parathyroid. A case report with immunohistochemistry and electron microscopy.". Arch Pathol Lab Med 119 (11): 1072-4. PMID 7487410.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 191. ISBN 978-0781767798.