Difference between revisions of "P16"
Jump to navigation
Jump to search

(→Benign) |
|||
| Line 41: | Line 41: | ||
</gallery> | </gallery> | ||
==Positive== | ==Positive== | ||
*[[Squamous cell carcinoma]] - esp. cervical SCC, anal SCC, penile SCC, HPV-associated head and neck SCC. | *[[Squamous cell carcinoma]] - esp. [[cervical SCC]], anal SCC, penile SCC, [[HPV-associated head and neck SCC]]. | ||
*High grade [[urothelial carcinoma]] ~86% of cases by PCR.<ref name=pmid25069600>{{Cite journal | last1 = Piaton | first1 = E. | last2 = Casalegno | first2 = JS. | last3 = Advenier | first3 = AS. | last4 = Decaussin-Petrucci | first4 = M. | last5 = Mege-Lechevallier | first5 = F. | last6 = Ruffion | first6 = A. | last7 = Mekki | first7 = Y. | title = p16(INK4a) overexpression is not linked to oncogenic human papillomaviruses in patients with high-grade urothelial cancer cells. | journal = Cancer Cytopathol | volume = 122 | issue = 10 | pages = 760-9 | month = Oct | year = 2014 | doi = 10.1002/cncy.21462 | PMID = 25069600 }}</ref> | *High grade [[urothelial carcinoma]] ~86% of cases by PCR.<ref name=pmid25069600>{{Cite journal | last1 = Piaton | first1 = E. | last2 = Casalegno | first2 = JS. | last3 = Advenier | first3 = AS. | last4 = Decaussin-Petrucci | first4 = M. | last5 = Mege-Lechevallier | first5 = F. | last6 = Ruffion | first6 = A. | last7 = Mekki | first7 = Y. | title = p16(INK4a) overexpression is not linked to oncogenic human papillomaviruses in patients with high-grade urothelial cancer cells. | journal = Cancer Cytopathol | volume = 122 | issue = 10 | pages = 760-9 | month = Oct | year = 2014 | doi = 10.1002/cncy.21462 | PMID = 25069600 }}</ref> | ||
*[[Serous carcinoma of the endometrium]] - should be strong.<ref name=pmid17581420>{{Cite journal | last1 = Chiesa-Vottero | first1 = AG. | last2 = Malpica | first2 = A. | last3 = Deavers | first3 = MT. | last4 = Broaddus | first4 = R. | last5 = Nuovo | first5 = GJ. | last6 = Silva | first6 = EG. | title = Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma. | journal = Int J Gynecol Pathol | volume = 26 | issue = 3 | pages = 328-33 | month = Jul | year = 2007 | doi = 10.1097/01.pgp.0000235065.31301.3e | PMID = 17581420 }}</ref> | *[[Serous carcinoma of the endometrium]] - should be strong.<ref name=pmid17581420>{{Cite journal | last1 = Chiesa-Vottero | first1 = AG. | last2 = Malpica | first2 = A. | last3 = Deavers | first3 = MT. | last4 = Broaddus | first4 = R. | last5 = Nuovo | first5 = GJ. | last6 = Silva | first6 = EG. | title = Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma. | journal = Int J Gynecol Pathol | volume = 26 | issue = 3 | pages = 328-33 | month = Jul | year = 2007 | doi = 10.1097/01.pgp.0000235065.31301.3e | PMID = 17581420 }}</ref> | ||
Revision as of 13:45, 28 September 2018
| P16 | |
|---|---|
| Immunostain in short | |
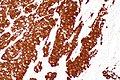
 HSIL showing the characteristic p16 staining. (WC/Nephron) | |
| Similar stains | HPV |
| Use | HSIL versus LSIL, HPV associated SCC versus non-HPV associated SCC |
| Subspeciality | gynecologic pathology, head and neck pathology |
| Normal staining pattern | nuclear and cytoplasmic |
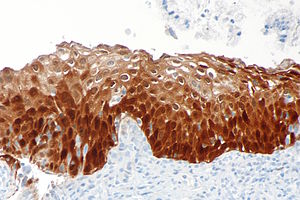
| Positive | endometrial tubal metaplasia, cervical SCC, HPV-associated head and neck SCC, serous carcinoma of the endometrium |

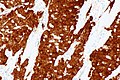
Endocervical AIS showing the characteristic p16 staining.
p16 is a commonly used immunostain. It can be considered a surrogate marker for HPV infection. p16, like most other "p" stains, is a nuclear stain.
Pattern
- Nuclear stain +/- cytoplasmic staining.
Use
- Squamous lesions of the uterine cervix - see HSIL.
- Head and neck squamous cell carcinoma, specifically human papillomavirus-associated head and neck squamous cell carcinoma.
Head and neck squamous cell carcinoma
p16 testing is useful in:
- Lymph node metastases with an unknown primary - positivity suggests an oropharyngeal primary.
- Oropharyngeal carcinomas.
Note:
- Like elsewhere, i.e. other anatomical sites, p16 is an imperfect surrogate marker for the presence of HPV.[1]
- Non-oropharyngeal sites (oral cavity, larynx, and hypopharynx) are not well-studied; however, it is known that p16 positivity is much less common in there.[1]
Images
Positive
- Squamous cell carcinoma - esp. cervical SCC, anal SCC, penile SCC, HPV-associated head and neck SCC.
- High grade urothelial carcinoma ~86% of cases by PCR.[2]
- Serous carcinoma of the endometrium - should be strong.[3]
- High-grade squamous intraepithelial lesion - full thickness, strong.
- A subset of LSIL stains with p16; however, it is not full thickness - see HSIL article.
Benign
- p16 endometrial tubal metaplasia.[4]
Focal staining
- Endometriosis - focal/weak staining may be seen.[5][6]
Negative
References
- ↑ 1.0 1.1 Stephen, JK.; Divine, G.; Chen, KM.; Chitale, D.; Havard, S.; Worsham, MJ. (2013). "Significance of p16 in Site-specific HPV Positive and HPV Negative Head and Neck Squamous Cell Carcinoma.". Cancer Clin Oncol 2 (1): 51-61. doi:10.5539/cco.v2n1p51. PMID 23935769.
- ↑ Piaton, E.; Casalegno, JS.; Advenier, AS.; Decaussin-Petrucci, M.; Mege-Lechevallier, F.; Ruffion, A.; Mekki, Y. (Oct 2014). "p16(INK4a) overexpression is not linked to oncogenic human papillomaviruses in patients with high-grade urothelial cancer cells.". Cancer Cytopathol 122 (10): 760-9. doi:10.1002/cncy.21462. PMID 25069600.
- ↑ Chiesa-Vottero, AG.; Malpica, A.; Deavers, MT.; Broaddus, R.; Nuovo, GJ.; Silva, EG. (Jul 2007). "Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma.". Int J Gynecol Pathol 26 (3): 328-33. doi:10.1097/01.pgp.0000235065.31301.3e. PMID 17581420.
- ↑ Horree, N.; Heintz, AP.; Sie-Go, DM.; van Diest, PJ. (2007). "p16 is consistently expressed in endometrial tubal metaplasia.". Cell Oncol 29 (1): 37-45. PMID 17429140.
- ↑ Stewart, CJ.; Bharat, C. (Feb 2016). "Clinicopathological and immunohistological features of polypoid endometriosis.". Histopathology 68 (3): 398-404. doi:10.1111/his.12755. PMID 26095917.
- ↑ O'Neill, CJ.; McCluggage, WG. (Jan 2006). "p16 expression in the female genital tract and its value in diagnosis.". Adv Anat Pathol 13 (1): 8-15. doi:10.1097/01.pap.0000201828.92719.f3. PMID 16462152.
- ↑ Pereira, TC.; Share, SM.; Magalhães, AV.; Silverman, JF. (Jan 2011). "Can we tell the site of origin of metastatic squamous cell carcinoma? An immunohistochemical tissue microarray study of 194 cases.". Appl Immunohistochem Mol Morphol 19 (1): 10-4. doi:10.1097/PAI.0b013e3181ecaf1c. PMID 20823766.