Squamous cell carcinoma of the uterine cervix
(Redirected from Cervical SCC)
Jump to navigation
Jump to search
| Squamous cell carcinoma of the uterine cervix | |
|---|---|
| Diagnosis in short | |
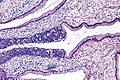
 Cervical squamous cell carcinoma in situ. H&E stain. | |
| LM DDx | squamous metaplasia of the uterine cervix, high-grade squamous intraepithelial lesion |
| IHC | p16 +ve |
| Gross | white lesion ~ usu. close to transformation zone |
| Site | uterine cervix |
|
| |
| Prevalence | most common cervical malignancy |
| Prognosis | usu. good, dependent on stage |
| Treatment | cervical cone, radical hysterectomy |
Squamous cell carcinoma of the uterine cervix, also cervical squamous cell carcinoma, is the most common primary malignancy of the uterine cervix.
General
- Most common type of cervical cancer.
Risk factors:
- Low socioeconomic status.
- Smoking.
- Early first intercourse.
- High risk partners.
- Human papillomavirus (HPV) infection, esp. "high risk HPV".
- HPV 16 closely assoc. with SCC.[1]
Gross
- White lesion.
- Firm.
Images
Microscopic
Features:
- Squamous differentiation.
- +/-Intracellular bridges.
- Scant-to-moderate cytoplasm.
- Penetration of basement membrane.
- May be challenging to determine.
- Nuclear atypia.
SCC of the cervix versus high-grade squamous intraepithelial lesion (carcinoma in situ): Invasive cancer look for:
- Eosinophilia.
- Extra large nuclei, i.e. nuclei 5x normal size.
- Stromal inflammation (lymphocytes, plasma cells).
- Long rete ridges.
- Numerous beeds/blobs of epithelial cells that seem unlikely to be rete ridges.
- Desmoplastic stroma - increased cellularity, spindle cell morphology.
DDx:
- Squamous metaplasia of the uterine cervix - if you can trace the squamous cells from a gland to the surface it is less likely to be invasive cancer.[2]
- High-grade squamous intraepithelial lesion +/- endocervical gland involvement.
Images
www:
- Microinvasive cervical SCC - low mag. (sunnybrook.ca).[3]
- Microinvasive cervical SCC - high mag. (sunnybrook.ca).[3]
- Cervical SCC - low mag. (ucsf.edu).[4]
- Cervical SCC - high mag. (uscf.edu).
Grading
Divided into:[5]
- Well-differentiated (keratinizing).
- Moderately differentiated (nonkeratinizing).
- Poorly differentiated.
Depth measurement
- Basement membrane (where it invades) to deepest point.
Note:
- Stage Ib - clinical diagnosis.
- Definition of stage Ib: clinically visible.
FIGO
Microinvasive SCC as per FIGO:
- Depth < 5 mm.
- Width < 7 mm.
- +/-Vascular invasion.
SGO
Microinvasive SCC as per The Society of Gynecologic Oncologists (SGO):
- <= 3 mm.
- Negative for vascular invasion.
Note:
- The SGO criteria the prefered by North American gynecologists.
IHC
- CK7, p63, p16 +ve (except verrucous variant)
- Factor VIII - to look for LVI.
Sign out
Biopsy
Early invasive SCC - things to report:
- Depth of invasion.
- Length of tumour.
- Number of blocks with tumour.
- Lymphovascular invasion (LVI).
- Margins.
UTERINE CERVIX, BIOPSY: - FRAGMENTS OF INVASIVE SQUAMOUS CELL CARCINOMA. -- DEPTH OF INVASION AND LENTH OF TUMOUR CANNOT BE ASSESSED. -- LYMPHOVASCULAR INVASION NOT APPARENT.
LESION, UTERINE CERVIX, BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA, MODERATELY DIFFERENTIATED, FRAGMENTED. - PLEASE SEE TUMOUR SUMMARY. TUMOUR SUMMARY - UTERINE CERVIX Specimen: Cervix. Procedure: Biopsy. Tumour Site: Cannot be determined. Tumour Size: Cannot be determined - see comment. Histologic Type: Squamous cell carcinoma, keratinizing. Histologic Grade: G2: Moderately differentiated. Stromal Invasion: Extent cannot be assessed - see comment. Lymph-Vascular Invasion: Not identified. Comment: The tissue submitted is essentially all tumour. The largest fragment measures 1.2 x 1.4 cm in the plane of section. Fragmentation and lack of normal histology preclude orientation. As both the in plane dimensions exceed 0.7 cm, this is at least a pT1b.
TAH-BSO
UTERUS, CERVIX, RIGHT AND LEFT OVARIES AND BILATERAL UTERINE TUBES, TOTAL HYSTERECTOMY AND BILATERAL SALPINGO-OOPHORECTOMY: - INVASIVE SQUAMOUS CELL CARCINOMA, pT1a1, pNx. -- MARGINS NEGATIVE FOR MALIGNANCY. -- PLEASE SEE TUMOUR SUMMARY. - PROLIFERATIVE ENDOMETRIUM. - UTERINE LEIOMYOMAS. - UTERINE TUBES WITH CHANGES COMPATIBLE WITH LIGATION, NO SIGNIFICANT PATHOLOGY. - OVARIES WITHOUT SIGNIFICANT PATHOLOGY.
See also
References
- ↑ De Boer, MA.; Peters, LA.; Aziz, MF.; Siregar, B.; Cornain, S.; Vrede, MA.; Jordanova, ES.; Fleuren, GJ. (Apr 2005). "Human papillomavirus type 18 variants: histopathology and E6/E7 polymorphisms in three countries.". Int J Cancer 114 (3): 422-5. doi:10.1002/ijc.20727. PMID 15551313.
- ↑ http://www.nature.com/modpathol/journal/v15/n3/pdf/3880520a.pdf
- ↑ 3.0 3.1 URL: http://sunnybrook.ca/content/?page=dept-labs-apath-gynpath-imgat-cvx-mal-microiscc. Accessed on: 2 May 2013.
- ↑ URL: http://missinglink.ucsf.edu/lm/IDS_107_Cervix_Ovary_Uterus/homepage.htm. Accessed on: 2 May 2013.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1077. ISBN 0-7216-0187-1.