Difference between revisions of "Gestational trophoblastic disease"
Jump to navigation
Jump to search
| Line 113: | Line 113: | ||
|} | |} | ||
Note: | Note: | ||
* ‡ The amount of Ki-67 staining varies considerably based on what one reads. Chen ''at al.''<ref>{{Cite journal | last1 = Chen | first1 = Y. | last2 = Shen | first2 = D. | last3 = Gu | first3 = Y. | last4 = Zhong | first4 = P. | last5 = Xie | first5 = J. | last6 = Song | first6 = Q. | title = The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion. | journal = Wien Klin Wochenschr | volume = 124 | issue = 5-6 | pages = 184-7 | month = Mar | year = 2012 | doi = 10.1007/s00508-011-0119-4 | PMID = 22218717 }}</ref> suggest 25% versus 5% for partial mole versus hydropic abortus. | * ‡ The amount of [[Ki-67]] staining varies considerably based on what one reads. Chen ''at al.''<ref>{{Cite journal | last1 = Chen | first1 = Y. | last2 = Shen | first2 = D. | last3 = Gu | first3 = Y. | last4 = Zhong | first4 = P. | last5 = Xie | first5 = J. | last6 = Song | first6 = Q. | title = The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion. | journal = Wien Klin Wochenschr | volume = 124 | issue = 5-6 | pages = 184-7 | month = Mar | year = 2012 | doi = 10.1007/s00508-011-0119-4 | PMID = 22218717 }}</ref> suggest 25% versus 5% for partial mole versus hydropic abortus. | ||
====Mole versus normal==== | ====Mole versus normal==== | ||
Revision as of 13:10, 30 June 2017
Gestational trophoblastic disease (abbreviated GTD), also gestational trophoblastic neoplasia (abbreviated GTN), includes choriocarcinoma and hydatidiform moles.
Overview
Most common
Overview of gestational trophoblastic disease:
| Type of mole | Gross | Nuclear atypia | Chorionic villi | IHC | DNA content | Micrographs |
|---|---|---|---|---|---|---|
| Complete mole | "snowstorm" | +/- ? | yes, all abnormal | p57(KIP2) -ve | Paternal, diploid | complete mole + intermed. trophoblast (WC), complete mole (WC) |
| Partial mole | grape-like clusters |
+/- | large villi, villi with cisterns, villi with cytotrophoblastic inclusions |
p57(KIP2) +ve | Maternal & paternal, tripoid | partial mole (utah.edu) |
| Choriocarcinoma | haemorrahagic, necrotic | marked | none | beta-hCG +ve | ? |
More comprehensive overview
Benign abnormal looking placenta:
- Placental site nodule (PSN).
- Exaggerated placental site (EPS).
Abnormal fertilization:
Tumours:
- Invasive mole.
- Choriocarcinoma.
- Placental site trophoblastic tumour (PSTT).
- Epithelioid trophoblastic tumour (ETT).
Entities
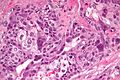
Choriocarcinoma
Main article: Choriocarcinoma
Hydatidiform moles
General
- Significance: increased risk for choriocarcinoma (in complete moles).
- Non-neoplastic proliferation.
Etymology:
- Hydatid is literally watery vesicle.[1]
Types
- Partial mole - see partial mole.
- Complete mole - see complete mole.
Extent:
- Invasive mole - not a subtype.
- Within uterine muscle +/- vessels.
Microscopic
Hydropic changes:
| Entity | Chorionic villi (outline) | Cisterns | Blood vessels | Nucleated RBCs | p57 / Ki-67[2] staining ‡ | Ploidy | Micrograph |
|---|---|---|---|---|---|---|---|
| Complete mole | bizarre; often not ovoid; fissures/slit-like gaps | well-developed | canalicular (thin walled) / few (???) | rare | -ve / ~70% | diploid / tetraploid | [1], [2], [3], [4] |
| Partial mole | jagged, still quasi ovoid | poorly developed / small | present | common | +ve / ~70% | triploid | [5], [6] |
| Hydropic abortus | smooth | poorly developed / small | common | common | +ve / ~20% | diploid | [7] |
Note:
- ‡ The amount of Ki-67 staining varies considerably based on what one reads. Chen at al.[3] suggest 25% versus 5% for partial mole versus hydropic abortus.
Mole versus normal
- Moles have large chorionic villi with edema and abnormal blood vessels.[4]
Non-molar versus partial versus complete - short version
Features:[5]
- Non-molar pregnancy: polar proliferation of trophoblastic tissue.
- Partial mole: Norwegian fjord periphery, circumferential or multifocal trophoblastic proliferation, fetal parts.
- Complete mole: grapes grossly, large villi with round borders.
IHC
- p57(KIP2) - the gene is strongly paternally imprinted and the paternal copy is inactived; its expression is from the maternal gene.
Molecular
- The type of mole can be determined by cytogenetics.[8]
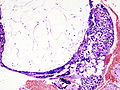
Partial hydatidiform mole
- AKA partial mole.
General
Genetics:
- Usually triploid (e.g. 69XXY).
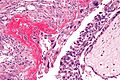
Microscopic
Features:
- Abnormal chorionic villi.
- Villi too large (>0.1 mm ?).
- Villi with cisterns.
- Contain fluid in the centre, i.e. are "hydropic".
- Villi with cytotrophoblastic inclusions.
- Cytotrophoblast in the core of a villus (normally it is only at the surface of the villus).
- May have fetal parts, such as nucleated RBCs.
- Trophoblastic proliferation.
- Without atypia.[9]
- "Norwegian fjord periphery"[5] - jagged border / irregular sawtooth-like periphery.
- Complete moles tend to have a smooth border
DDx:
- Complete hydatidiform mole.
- Placental mesenchymal dysplasia.
- Hydropic abortus - see products of conception and chorionic villi.
Images:
IHC
Features:[10]
- Ki-67 ~ 25+/-5% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-1%.
- p53 ~ 22+/-12% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-3%.
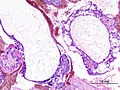
Complete hydatidiform mole
General
Epidemiology:
- May precede choriocarcinoma[11] ~ 1-2% risk.
Genetics:
- Diploid - most are 46XX.
- Male derived, i.e. arise from DNA in sperm; empty egg fertilized.
Gross/Radiology
Image:
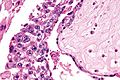
Microscopic
Features:
- No normal villi.
- No fetal parts seen.
- Very rarely nucleated RBCs.
Images
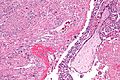
Invasive hydatidiform mole
General
- This is not a distinct subtype - see hydatidiform mole.
Microscopic
Features:
- Chorionic villi - abnormal +/- normal.
- Trophoblastic cells within uterine muscle +/- vessels - key feature.
DDx:
- Choriocarcinoma - lack chorionic villi, usu. hemorrhagic.
Images
Entities - intermediate trophoblast
| Entity | Key feature | Other histologic features | IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|
| Placental site nodule (PSN) | paucicellular, hyaline material | no mitotic activity | p16 -ve, MIB1 low | EPS, squamous carcinoma | post-partum | (ijpmonline.org) |
| Exaggerated placental site (EPS) | abundant intermediate trophoblasts - between muscle | no mitotic activity | MIB1 ~0% | PSTT, PSN | post-partum | Image? |
| Placental site trophoblastic tumour (PSTT) | abundant cytoplasm - not clear, dyscohesive | +/-multinucleation | MIB1 high, p63 -ve, CD146 +ve | EPS, choriocarcinoma | Other? | (webpathology.com) |
| Epithelioid trophoblastic tumour (ETT) | nests of cells in hyaline stroma | eosinophilic cytoplasm, central nucleus | MIB1 low, p63 +ve, CD146 -ve | squamous carcinoma | Other? | (webpathology.com) |
| Choriocarcinoma | polygonal cells with clear cytoplasm (cytotrophoblasts) | multinucleated cells with smudged nuclei (syncytiotrophoblasts), no chorionic villi | beta-hCG +ve, p63 +ve | invasive hydatidiform mole, PSTT | elevated beta-hCG (serum); not intermediate trophoblast derived. | (webpathology.com) |
Placental site nodule
- Abbreviated PSN.
Main article: Placental site nodule
Exaggerated placental site
- Abbreviated EPS.
- Previously known as syncytial endometritis.[15]
Main article: Exaggerated placental site
Placental site trophoblastic tumour
- Abbreviated PSTT.
- Malignant counterpart of exaggerated placental site (abbreviated EPS).
General
- Derived from intermediate trophoblast.
- Follows pregnancy.
- May be associated with nephrotic syndrome[16] with granular IgM staining.[17]
Clinical:
- Raised (serum) beta-hCG - but usually not has high as in choriocarcinoma.
- Prognosis dependent on time of diagnosis from last pregnancy.
- <48 months = good prognosis.[18]
Microscopic
Features:
- Large cells:
- Nuclear pleomorphism.
- Cytoplasm:
- Abundant.
- Solid, i.e. not vesicular.
- Light basophilic, not clear - key feature.
- NC ratio ~ normal.
- +/-Multinucleated cells.
- Ectatic blood vessels.
Note:
- No chorionic villi.
- If villi are present... it is probably a hydatidiform mole.
DDx:
- Exaggerated placental site - EPS has near zero Ki-67.
- Choriocarcinoma - choriocarcinoma biphasic.[20]
Images:
IHC
Features:[21]
- CD146 +ve.
- p63 -ve.
- Ki-67 ~14+/-7%.
- Choriocarcinoma ~69+/-20%.
Epithelioid trophoblastic tumour
- Abbreviated ETT.
General
- Often in endocervix.
- Malignant counterpart of placental site nodule or PSN.
Clinical:
- Vaginal bleeding.
- Elevated beta-hCG.
Gross
Features:[22]
- Solid mass.
- Flesh-like appearance.
Image:
Microscopic
Features:[23]
- Architecture: nests in hyaline matrix.
- Cytoplasm: abundant, eosinophilic.
DDx:
- Invasive squamous cell carcinoma.
Images:
IHC
Features:[24]
- Cyclin E +ve (nuclear).
- p16 -ve.
- +ve (nuclear) in squamous cell carcinoma of the cervix.
Others:
- HMCK -ve.
- SCC +ve.
Note:
- p63 not useful... +ve in both SCC and ETT.
See also
- Hydatid disease - due to Echinoccus spp. such as E. granulosus.
- Chorionic villi.
- Ectopic pregnancy.
- Placenta.
- Arias-Stella reaction - benign atypical changes of the endometrium associated with trophoblastic tissue.
References
- ↑ URL: http://dictionary.reference.com/browse/hydatid.
- ↑ URL: http://www.ihcworld.com/_newsletter/2003/focus_mar_2003.pdf. Accessed on: 28 May 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ URL: http://pathologyoutlines.com/placenta.html#hydatgeneral.
- ↑ 5.0 5.1 Howat, AJ.; Beck, S.; Fox, H.; Harris, SC.; Hill, AS.; Nicholson, CM.; Williams, RA. (Jul 1993). "Can histopathologists reliably diagnose molar pregnancy?". J Clin Pathol 46 (7): 599-602. PMID 8157742. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC501384/?page=3.
- ↑ Merchant SH, Amin MB, Viswanatha DS, Malhotra RK, Moehlenkamp C, Joste NE (February 2005). "p57KIP2 immunohistochemistry in early molar pregnancies: emphasis on its complementary role in the differential diagnosis of hydropic abortuses". Hum. Pathol. 36 (2): 180–6. doi:10.1016/j.humpath.2004.12.007. PMID 15754295.
- ↑ 7.0 7.1 Fukunaga, M. (Dec 2002). "Immunohistochemical characterization of p57(KIP2) expression in early hydatidiform moles.". Hum Pathol 33 (12): 1188-92. doi:10.1053/hupa.2002.129421. PMID 12514787.
- ↑ http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf
- ↑ URL: http://pathologyoutlines.com/placenta.html#incompletemole. Accessed on: 9 August 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1111. ISBN 0-7216-0187-1.
- ↑ URL:http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589. Accessed on: 27 July 2010.
- ↑ Abike, F.; Temizkan, O.; Payasli, A.; Avsar, F.; Karahan, N.; Baspinar, S. (Jan 2008). "Postmenopausal complete hydatidiform mole: a case report.". Maturitas 59 (1): 95-8. doi:10.1016/j.maturitas.2007.10.005. PMID 18162339.
- ↑ McDonald, TW.; Ruffolo, EH. (Feb 1983). "Modern management of gestational trophoblastic disease.". Obstet Gynecol Surv 38 (2): 67-83. PMID 6300738.
- ↑ URL: http://www.webpathology.com/image.asp?case=565&n=7. Accessed on: 22 May 2014.
- ↑ Bonazzi, C.; Urso, M.; Dell'Anna, T.; Sacco, S.; Buda, A.; Cantú, MG. (Aug 2004). "Placental site trophoblastic tumor: an overview.". J Reprod Med 49 (8): 585-8. PMID 15457847.
- ↑ Komatsuda, A.; Nakamoto, Y.; Asakura, K.; Yasuda, T.; Imai, H.; Miura, AB. (May 1992). "Case report: nephrotic syndrome associated with a total hydatidiform mole.". Am J Med Sci 303 (5): 309-12. PMID 1580319.
- ↑ 18.0 18.1 Schmid, P.; Nagai, Y.; Agarwal, R.; Hancock, B.; Savage, PM.; Sebire, NJ.; Lindsay, I.; Wells, M. et al. (Jul 2009). "Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study.". Lancet 374 (9683): 48-55. doi:10.1016/S0140-6736(09)60618-8. PMID 19552948.
- ↑ Baergen, RN.; Rutgers, JL.; Young, RH.; Osann, K.; Scully, RE. (Mar 2006). "Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance.". Gynecol Oncol 100 (3): 511-20. doi:10.1016/j.ygyno.2005.08.058. PMID 16246400.
- ↑ URL: http://www.webpathology.com/image.asp?n=3&Case=588. Accessed on: 1 January 2012.
- ↑ Shih, IM.; Kurman, RJ. (Jan 1998). "Ki-67 labeling index in the differential diagnosis of exaggerated placental site, placental site trophoblastic tumor, and choriocarcinoma: a double immunohistochemical staining technique using Ki-67 and Mel-CAM antibodies.". Hum Pathol 29 (1): 27-33. PMID 9445130.
- ↑ 22.0 22.1 Fadare, O.; Parkash, V.; Carcangiu, ML.; Hui, P. (Jan 2006). "Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement.". Mod Pathol 19 (1): 75-82. doi:10.1038/modpathol.3800485. PMID 16258513.
- ↑ 23.0 23.1 URL: http://www.webpathology.com/image.asp?case=589&n=2. Accessed on: 15 August 2011.
- ↑ Mao, TL.; Seidman, JD.; Kurman, RJ.; Shih, IeM. (Sep 2006). "Cyclin E and p16 immunoreactivity in epithelioid trophoblastic tumor--an aid in differential diagnosis.". Am J Surg Pathol 30 (9): 1105-10. doi:10.1097/01.pas.0000209854.28282.87. PMID 16931955.