Difference between revisions of "Collagenous colitis"
Jump to navigation
Jump to search
(redirect w/ cat.) |
|||
| (15 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Collagenous_colitis_-_high_mag.jpg | |||
| Width = | |||
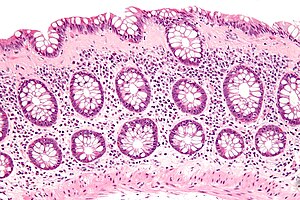
| Caption = Collagenous colitis. [[H&E stain]]. | |||
| Micro = intraepithelial lymphocytes (>20/100 enterocytes), subepithelial collagen band (>= 10 micrometres thick) | |||
| Subtypes = | |||
| LMDDx = [[lymphocytic colitis]], [[Crohn's disease]] (very rare) | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[colon]] - typically more prominent proximally | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = predominantly women (women:men=20:1) | |||
| Signs = | |||
| Symptoms = diarrhea, non-bloody | |||
| Prevalence = | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = normal | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = [[irritable bowel syndrome]], [[lymphocytic colitis]] | |||
}} | |||
'''Collagenous colitis''' is a type of [[microscopic colitis]]. It has a characteristic clinical presentation and no apparent endoscopic changes. | |||
==General== | |||
*Collagenous colitis may be related to [[lymphocytic colitis]]. | |||
**It is hypothesized that these conditions may be the same pathology at different time points.<ref name=medscape180664/> | |||
*May be associated with to [[collagenous gastritis]] in adults.<ref name=pmid19730387>{{Cite journal | last1 = Brain | first1 = O. | last2 = Rajaguru | first2 = C. | last3 = Warren | first3 = B. | last4 = Booth | first4 = J. | last5 = Travis | first5 = S. | title = Collagenous gastritis: reports and systematic review. | journal = Eur J Gastroenterol Hepatol | volume = 21 | issue = 12 | pages = 1419-24 | month = Dec | year = 2009 | doi = 10.1097/MEG.0b013e32832770fa | PMID = 19730387 }}</ref> | |||
Presentation: | |||
*Chronic diarrhea, non-bloody.<ref name=medscape180664>URL: [http://emedicine.medscape.com/article/180664-overview http://emedicine.medscape.com/article/180664-overview]. Accessed on: 31 May 2010.</ref> | |||
Notes: | |||
*Clinical DDx includes [[irritable bowel syndrome]] - which has no or subtle histopathologic changes. | |||
*This pathology also afflicits rectum; however, it is less commonly found there. | |||
**The rectum is afflicted in approximately in 65% of cases.<ref name=pmid12018911>{{cite journal |author=Agnarsdottir M, Gunnlaugsson O, Orvar KB, ''et al.'' |title=Collagenous and lymphocytic colitis in Iceland |journal=Dig. Dis. Sci. |volume=47 |issue=5 |pages=1122–8 |year=2002 |month=May |pmid=12018911 |doi= |url=}}</ref> | |||
===Epidemiology=== | |||
*Age: a disease of adults - usually 50s. | |||
*Sex: | |||
**LC males ~= females,<ref name=medscape180664/> | |||
**CC females:males = 20:1.<ref name=medscape180664/> | |||
*Drugs are associated with LC and CC. | |||
**[[NSAID]]s - posulated association/weak association, | |||
**SSRIs (used primarily for depression) - moderate association, dependent on specific drug. | |||
*Associated with autoimmune disorders - [[celiac disease]], [[diabetes mellitus]], [[thyroid]] disorders and [[arthritis]].<ref name=pmid19109861>{{cite journal |author=Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S |title=Diagnosis and management of microscopic colitis |journal=World J. Gastroenterol. |volume=14 |issue=48 |pages=7280-8 |year=2008 |month=December |pmid=19109861 |doi= |url=http://www.wjgnet.com/1007-9327/14/7280.asp}}</ref> | |||
*No increased risk of colorectal carcinoma.<ref name=pmid19109861/> | |||
===Treatment=== | |||
*Sometimes just follow-up. | |||
*Steroids - budesonide -- short-term treatment.<ref name=pmid19109861/> | |||
==Gross== | |||
*Endoscopic examination is normal. | |||
**This is why it is called a ''[[microscopic colitis]]''. | |||
==Microscopic== | |||
Features: | |||
*[[Intraepithelial lymphocytes]] - '''important'''. | |||
*Collagenous material in the lamina propria (pink on H&E) -- '''key feature'''. | |||
**Can be demonstrated with a trichrome stain -- collagen = green on trichrome. | |||
**Subepithelial collagen needs to be >= 10 micrometres thick for diagnosis.<ref name=pmid19109861/> | |||
***8 micrometres is the diameter of a [[RBC]]. | |||
***The normal thickness of the subepithelial collagen is 3 micrometres.<ref name=pmid19109861/> | |||
***Transverse colon usually thickest - in one series ~ 47 micrometres on average.<ref name=pmid10208468>{{Cite journal | last1 = Offner | first1 = FA. | last2 = Jao | first2 = RV. | last3 = Lewin | first3 = KJ. | last4 = Havelec | first4 = L. | last5 = Weinstein | first5 = WM. | title = Collagenous colitis: a study of the distribution of morphological abnormalities and their histological detection. | journal = Hum Pathol | volume = 30 | issue = 4 | pages = 451-7 | month = Apr | year = 1999 | doi = | PMID = 10208468 }}</ref> | |||
**Thickening is usually patchy.<ref name=pmid1740280/> | |||
**Thickening "follows the crypts from the surface" - useful for differentiating from tangential sections of the basement membrane.<ref name=bell>Bell, D. 4 Mar 2009.</ref> | |||
**Collagen may envelope capillaries - useful to discern from basement membrane.<ref name=bell>Bell, D. 4 Mar 2009.</ref> | |||
Notes: | |||
*CC is typically more prominent in the proximal colon - may reflect concentration gradient of offending causitive agents.<ref name=pmid19109861/> | |||
*Significant negative findings:<ref name=hopkins_cc_lc>[http://hopkins-gi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&disease=29&organ=6&lang_id=1 http://hopkins-gi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&disease=29&organ=6&lang_id=1]</ref> | |||
**No [[PMN]]s. | |||
**No crypt distortion. | |||
*Thickened collagen band uncommon in rectum.<ref name=pmid1740280>{{Cite journal | last1 = Tanaka | first1 = M. | last2 = Mazzoleni | first2 = G. | last3 = Riddell | first3 = RH. | title = Distribution of collagenous colitis: utility of flexible sigmoidoscopy. | journal = Gut | volume = 33 | issue = 1 | pages = 65-70 | month = Jan | year = 1992 | doi = | PMID = 1740280 }}</ref> | |||
*Described in association of [[pseudomembranous colitis|pseudomembranes]].<ref name=pmid14508399>{{Cite journal | last1 = Yuan | first1 = S. | last2 = Reyes | first2 = V. | last3 = Bronner | first3 = MP. | title = Pseudomembranous collagenous colitis. | journal = Am J Surg Pathol | volume = 27 | issue = 10 | pages = 1375-9 | month = Oct | year = 2003 | doi = | PMID = 14508399 }}</ref> | |||
DDx: | |||
*[[Lymphocytic colitis]]. | |||
*[[Crohn's disease]] - very rare, may be a perfect mimic.<ref name=pmid10478667>{{Cite journal | last1 = Goldstein | first1 = NS. | last2 = Gyorfi | first2 = T. | title = Focal lymphocytic colitis and collagenous colitis: patterns of Crohn's colitis? | journal = Am J Surg Pathol | volume = 23 | issue = 9 | pages = 1075-81 | month = Sep | year = 1999 | doi = | PMID = 10478667 }}</ref> | |||
===Images=== | |||
<gallery> | |||
Image:Collagenous_colitis_-_intermed_mag.jpg | CC - intermed mag. (WC/Nephron) | |||
Image:Collagenous_colitis_-_high_mag.jpg | CC - high mag. (WC/Nephron) | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
TRANSVERSE COLON, BIOPSY: | |||
- COLLAGENOUS COLITIS. | |||
</pre> | |||
===Micro=== | |||
The sections show colonic mucosa with abundant intraepithelial lymphocytes (>20 lymphocytes/100 surface epithelial cells). A prominent collagen band is apparent below the epithelium (>10 micrometres thick). The glandular architecture is within normal limits. | |||
There are no granulomas. No neutrophilic cryptitis is apparent. The epithelium matures | |||
appropriately to the surface. | |||
==See also== | |||
*[[Colon]]. | |||
*[[Lymphocytic colitis]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Colon]] | |||
[[Category:Gastrointestinal pathology]] | |||
Latest revision as of 14:30, 25 May 2016
| Collagenous colitis | |
|---|---|
| Diagnosis in short | |
 Collagenous colitis. H&E stain. | |
|
| |
| LM | intraepithelial lymphocytes (>20/100 enterocytes), subepithelial collagen band (>= 10 micrometres thick) |
| LM DDx | lymphocytic colitis, Crohn's disease (very rare) |
| Site | colon - typically more prominent proximally |
|
| |
| Clinical history | predominantly women (women:men=20:1) |
| Symptoms | diarrhea, non-bloody |
| Endoscopy | normal |
| Clin. DDx | irritable bowel syndrome, lymphocytic colitis |
Collagenous colitis is a type of microscopic colitis. It has a characteristic clinical presentation and no apparent endoscopic changes.
General
- Collagenous colitis may be related to lymphocytic colitis.
- It is hypothesized that these conditions may be the same pathology at different time points.[1]
- May be associated with to collagenous gastritis in adults.[2]
Presentation:
- Chronic diarrhea, non-bloody.[1]
Notes:
- Clinical DDx includes irritable bowel syndrome - which has no or subtle histopathologic changes.
- This pathology also afflicits rectum; however, it is less commonly found there.
- The rectum is afflicted in approximately in 65% of cases.[3]
Epidemiology
- Age: a disease of adults - usually 50s.
- Sex:
- Drugs are associated with LC and CC.
- NSAIDs - posulated association/weak association,
- SSRIs (used primarily for depression) - moderate association, dependent on specific drug.
- Associated with autoimmune disorders - celiac disease, diabetes mellitus, thyroid disorders and arthritis.[4]
- No increased risk of colorectal carcinoma.[4]
Treatment
- Sometimes just follow-up.
- Steroids - budesonide -- short-term treatment.[4]
Gross
- Endoscopic examination is normal.
- This is why it is called a microscopic colitis.
Microscopic
Features:
- Intraepithelial lymphocytes - important.
- Collagenous material in the lamina propria (pink on H&E) -- key feature.
- Can be demonstrated with a trichrome stain -- collagen = green on trichrome.
- Subepithelial collagen needs to be >= 10 micrometres thick for diagnosis.[4]
- Thickening is usually patchy.[6]
- Thickening "follows the crypts from the surface" - useful for differentiating from tangential sections of the basement membrane.[7]
- Collagen may envelope capillaries - useful to discern from basement membrane.[7]
Notes:
- CC is typically more prominent in the proximal colon - may reflect concentration gradient of offending causitive agents.[4]
- Significant negative findings:[8]
- No PMNs.
- No crypt distortion.
- Thickened collagen band uncommon in rectum.[6]
- Described in association of pseudomembranes.[9]
DDx:
- Lymphocytic colitis.
- Crohn's disease - very rare, may be a perfect mimic.[10]
Images
Sign out
TRANSVERSE COLON, BIOPSY: - COLLAGENOUS COLITIS.
Micro
The sections show colonic mucosa with abundant intraepithelial lymphocytes (>20 lymphocytes/100 surface epithelial cells). A prominent collagen band is apparent below the epithelium (>10 micrometres thick). The glandular architecture is within normal limits.
There are no granulomas. No neutrophilic cryptitis is apparent. The epithelium matures appropriately to the surface.
See also
References
- ↑ 1.0 1.1 1.2 1.3 URL: http://emedicine.medscape.com/article/180664-overview. Accessed on: 31 May 2010.
- ↑ Brain, O.; Rajaguru, C.; Warren, B.; Booth, J.; Travis, S. (Dec 2009). "Collagenous gastritis: reports and systematic review.". Eur J Gastroenterol Hepatol 21 (12): 1419-24. doi:10.1097/MEG.0b013e32832770fa. PMID 19730387.
- ↑ Agnarsdottir M, Gunnlaugsson O, Orvar KB, et al. (May 2002). "Collagenous and lymphocytic colitis in Iceland". Dig. Dis. Sci. 47 (5): 1122–8. PMID 12018911.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S (December 2008). "Diagnosis and management of microscopic colitis". World J. Gastroenterol. 14 (48): 7280-8. PMID 19109861. http://www.wjgnet.com/1007-9327/14/7280.asp.
- ↑ Offner, FA.; Jao, RV.; Lewin, KJ.; Havelec, L.; Weinstein, WM. (Apr 1999). "Collagenous colitis: a study of the distribution of morphological abnormalities and their histological detection.". Hum Pathol 30 (4): 451-7. PMID 10208468.
- ↑ 6.0 6.1 Tanaka, M.; Mazzoleni, G.; Riddell, RH. (Jan 1992). "Distribution of collagenous colitis: utility of flexible sigmoidoscopy.". Gut 33 (1): 65-70. PMID 1740280.
- ↑ 7.0 7.1 Bell, D. 4 Mar 2009.
- ↑ http://hopkins-gi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&disease=29&organ=6&lang_id=1
- ↑ Yuan, S.; Reyes, V.; Bronner, MP. (Oct 2003). "Pseudomembranous collagenous colitis.". Am J Surg Pathol 27 (10): 1375-9. PMID 14508399.
- ↑ Goldstein, NS.; Gyorfi, T. (Sep 1999). "Focal lymphocytic colitis and collagenous colitis: patterns of Crohn's colitis?". Am J Surg Pathol 23 (9): 1075-81. PMID 10478667.

