Difference between revisions of "Chromophobe renal cell carcinoma"
(→IHC) |
|||
| (7 intermediate revisions by the same user not shown) | |||
| Line 6: | Line 6: | ||
| Micro = pale/clear (or eosinophilic) cytoplasm with wisps of eosinophilic material, perinuclear clearing (a pale halo surrounds the nucleus), periphery of cell distinct (cell membrane is easy to discern -- plant cell-like) | | Micro = pale/clear (or eosinophilic) cytoplasm with wisps of eosinophilic material, perinuclear clearing (a pale halo surrounds the nucleus), periphery of cell distinct (cell membrane is easy to discern -- plant cell-like) | ||
| Subtypes = classic, eosinophilic variant | | Subtypes = classic, eosinophilic variant | ||
| LMDDx = [[clear cell renal cell carcinoma]] (classic), [[renal oncocytoma]], [[clear cell renal cell carcinoma]] eosinophilic variant | | LMDDx = [[clear cell renal cell carcinoma]] (classic), [[renal oncocytoma]], [[clear cell renal cell carcinoma]] eosinophilic variant, [[renal hybrid oncocytic/chromophobe tumour]], other [[renal tumours with eosinophilic cytoplasm]] | ||
| Stains = [[Hale's colloidal iron]] ([[Mueller-Mowry stain]]) +ve | | Stains = [[Hale's colloidal iron]] ([[Mueller-Mowry stain]]) +ve | ||
| IHC = CK7 +ve cell membrane, CD117 +ve, vimentin -ve | | IHC = CK7 +ve cell membrane, CD117 +ve, vimentin -ve | ||
| Line 70: | Line 70: | ||
**Perinuclear clearing is ''not'' seen in clear cell RCC. | **Perinuclear clearing is ''not'' seen in clear cell RCC. | ||
**ChRCC has wisps in the cytoplasm. | **ChRCC has wisps in the cytoplasm. | ||
*Other [[clear cell tumours]]. | |||
*[[Benign clear cell clusters of the kidney]] - somewhat controversial. | |||
====Images==== | ====Images==== | ||
| Line 99: | Line 101: | ||
#*Perinuclear clearing is ''not'' seen in clear cell RCC. | #*Perinuclear clearing is ''not'' seen in clear cell RCC. | ||
#*ChRCC has wisps in the cytoplasm. | #*ChRCC has wisps in the cytoplasm. | ||
#[[Renal hybrid oncocytic/chromophobe tumour]]. | |||
#Other [[renal tumours with eosinophilic cytoplasm]]. | #Other [[renal tumours with eosinophilic cytoplasm]]. | ||
====Images==== | ====Images==== | ||
| Line 157: | Line 160: | ||
*[[DOG1]] +ve (Swalchick ''et al.''<ref name=pmid26678977>{{Cite journal | last1 = Swalchick | first1 = W. | last2 = Shamekh | first2 = R. | last3 = Bui | first3 = MM. | title = Is DOG1 Immunoreactivity Specific to Gastrointestinal Stromal Tumor? | journal = Cancer Control | volume = 22 | issue = 4 | pages = 498-504 | month = Oct | year = 2015 | doi = | PMID = 26678977 }}</ref> 32 +ve of 37 cases; Zhao ''et al.''<ref name=pmid25596994>{{Cite journal | last1 = Zhao | first1 = W. | last2 = Tian | first2 = B. | last3 = Wu | first3 = C. | last4 = Peng | first4 = Y. | last5 = Wang | first5 = H. | last6 = Gu | first6 = WL. | last7 = Gao | first7 = FH. | title = DOG1, cyclin D1, CK7, CD117 and vimentin are useful immunohistochemical markers in distinguishing chromophobe renal cell carcinoma from clear cell renal cell carcinoma and renal oncocytoma. | journal = Pathol Res Pract | volume = 211 | issue = 4 | pages = 303-7 | month = Apr | year = 2015 | doi = 10.1016/j.prp.2014.12.014 | PMID = 25596994 }}</ref> 32 +ve of 32 cases). | *[[DOG1]] +ve (Swalchick ''et al.''<ref name=pmid26678977>{{Cite journal | last1 = Swalchick | first1 = W. | last2 = Shamekh | first2 = R. | last3 = Bui | first3 = MM. | title = Is DOG1 Immunoreactivity Specific to Gastrointestinal Stromal Tumor? | journal = Cancer Control | volume = 22 | issue = 4 | pages = 498-504 | month = Oct | year = 2015 | doi = | PMID = 26678977 }}</ref> 32 +ve of 37 cases; Zhao ''et al.''<ref name=pmid25596994>{{Cite journal | last1 = Zhao | first1 = W. | last2 = Tian | first2 = B. | last3 = Wu | first3 = C. | last4 = Peng | first4 = Y. | last5 = Wang | first5 = H. | last6 = Gu | first6 = WL. | last7 = Gao | first7 = FH. | title = DOG1, cyclin D1, CK7, CD117 and vimentin are useful immunohistochemical markers in distinguishing chromophobe renal cell carcinoma from clear cell renal cell carcinoma and renal oncocytoma. | journal = Pathol Res Pract | volume = 211 | issue = 4 | pages = 303-7 | month = Apr | year = 2015 | doi = 10.1016/j.prp.2014.12.014 | PMID = 25596994 }}</ref> 32 +ve of 32 cases). | ||
**Useful in ChRCC versus clear cell RCC. | **Useful in ChRCC versus clear cell RCC. | ||
A panel: | |||
*CK7, [[PAX8]], CD117, CD10, [[Mueller-Mowry stain]]. | |||
===Comparison between some renal tumours with eosinophilic cytoplasm=== | |||
{| class="wikitable sortable" | |||
!Tumour | |||
![[CK7]] | |||
![[CD117]] | |||
![[GATA3]] | |||
|- | |||
| [[Renal oncocytoma]] | |||
| -ve † | |||
| +ve | |||
| -ve/+ve | |||
|- | |||
| Chromophobe renal cell carcinoma | |||
| +ve ‡ | |||
| +ve | |||
| -ve | |||
|- | |||
| [[Low-grade oncocytic tumour]] | |||
| +ve | |||
| -ve | |||
| +ve | |||
|- | |||
|} | |||
† may have scattered positive cells<br> | |||
‡ diffuse and strong | |||
==Molecular== | ==Molecular== | ||
| Line 184: | Line 216: | ||
Negative: AMACR, CD10, CD68, RCC, vimentin. | Negative: AMACR, CD10, CD68, RCC, vimentin. | ||
</pre> | </pre> | ||
===Micro=== | |||
The sections show a sheeting tumour with abundant and eosinophilic cytoplasm. The tumour cell cell membranes are prominent and plant-like. Perinuclear clearing is present. Binucleation is frequent and the nuclear membranes moderately irregular. No definite papillae or macrophages are present. Nucleoli are not prominent. Small blood vessels are not prominent. | |||
====Alternate==== | |||
The sections show a tumour composed of compact nests. The cytoplasm is abundant and eosinophilic. Perinuclear clearing is prominent. Binucleation is frequent and the nuclear membranes moderately irregular to round. No definite papillae or macrophages are present. Nucleoli are not prominent. | |||
==See also== | ==See also== | ||
Latest revision as of 15:04, 18 April 2024
| Chromophobe renal cell carcinoma | |
|---|---|
| Diagnosis in short | |
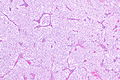
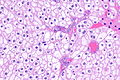
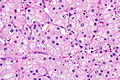
 Chromophobe renal cell carcinoma showing the characteristic perinuclear clearing and distinctive (plant-like) cellular borders. H&E stain. | |
|
| |
| LM | pale/clear (or eosinophilic) cytoplasm with wisps of eosinophilic material, perinuclear clearing (a pale halo surrounds the nucleus), periphery of cell distinct (cell membrane is easy to discern -- plant cell-like) |
| Subtypes | classic, eosinophilic variant |
| LM DDx | clear cell renal cell carcinoma (classic), renal oncocytoma, clear cell renal cell carcinoma eosinophilic variant, renal hybrid oncocytic/chromophobe tumour, other renal tumours with eosinophilic cytoplasm |
| Stains | Hale's colloidal iron (Mueller-Mowry stain) +ve |
| IHC | CK7 +ve cell membrane, CD117 +ve, vimentin -ve |
| Gross | grey-beige, lacks central scar |
| Grossing notes | total nephrectomy for tumour grossing, partial nephrectomy grossing |
| Staging | kidney cancer staging |
| Site | kidney - see renal tumours |
|
| |
| Syndromes | Birt–Hogg–Dubé syndrome |
|
| |
| Prevalence | relatively common |
| Clin. DDx | other renal tumours |
| Treatment | surgical resection |
Chromophobe renal cell carcinoma, abbreviated ChRCC, is a relatively common form of renal cell carcinoma.
General
- Least common of the common types of RCC (clear cell RCC, papillary RCC, chromophobe RCC).
- ISUP nucleolar grading (replaces Fuhrman grading) not done for this entity, as it does not appear to have any predictive value.[1]
- May be associated with Birt–Hogg–Dubé syndrome.[2]
- Can be seen in the context of renal oncocytosis.[3]
Subtypes
There are two subtypes:[4]
- Classic.
- Eosinophilic variant.
Gross
- Grey-beige colour.[5]
- Solitary, usually.‡
- Well-circumscribed.
Note:
- ‡ Approximately 3% are multifocal.[6]
Image
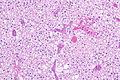
Microscopic
Classic
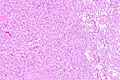
Features - classic type (3 P's memory device):[7][4]
- Pale cytoplasm, with wisps of eosinophilic material; the cells are not completely clear, they have "cobwebs".
- Perinuclear clearing, i.e. a pale halo surrounds the nucleus - key feature.
- Periphery of cell distinct, i.e. cell membrane is easy to discern.
Notes:
- May have psammoma bodies.
- May be described as "plant-like"; plant cells have (thick) cell walls.
- The perinuclear clearing is often somewhat patchy, i.e. it is usually not present in very tumour cell.
DDx:
- Clear cell RCC (classic).
- Perinuclear clearing is not seen in clear cell RCC.
- ChRCC has wisps in the cytoplasm.
- Other clear cell tumours.
- Benign clear cell clusters of the kidney - somewhat controversial.
Images
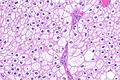
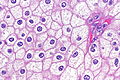
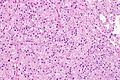
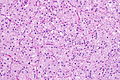
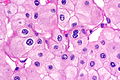
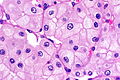
Eosinophilic variant
Features - eosinophilic variant:[4]
- Eosinophilic (finely granular) cytoplasm.
- Perinuclear clearing - key feature.
- Periphery of cell distinct.
- Smaller cells than classic subtype.
Notes:
- May have psammoma bodies.
DDx:
- Oncocytoma - particularly the eosinophilic variant.
- IHC may be useful to differentiate (CK7: oncocytoma = cytoplasm +ve, chromophobe = cell membrane +ve).
- A comparison based on histomorphology: Tabular comparison between ChRCC & oncocytoma.
- Oncocytoma typically has: no perinuclear clearing, no raisinoid nuclei, no binucleation.
- Clear cell RCC, eosinophilic variant.
- Perinuclear clearing is not seen in clear cell RCC.
- ChRCC has wisps in the cytoplasm.
- Renal hybrid oncocytic/chromophobe tumour.
- Other renal tumours with eosinophilic cytoplasm.
Images
Case 1
Case 2
www
Stains
- Hale's colloidal iron +ve (blue granular cytoplasmic).
- Oncocytoma -ve.
Note:
- This seems to be a difficult stain to get working.
Images
- ChRCC Hale's colloidal iron - several images (nature.com).
- ChRCC Hale's colloidal iron (ultrapath.org).[8]
- ChRCC Hale's colloidal iron (diagnosticpathology.org).
IHC
- CK7 +ve cell membrane.[4]
- Useful for differentiating from oncocytoma.
- CD117 +ve.
- Vimentin -ve.[9][10]
Others:[11]
- CD10 -ve.
- RCC -ve.
Uncommon stains for ChRCC versus oncocytoma:
ChRCC versus clear cell RCC
- CD117 +ve.
- -ve in CCRCC.
- CA9 (carbonic anhydrase 9) -ve.
- +ve (strong membranous) in CCRCC.[15]
- CK7 +ve.
- -ve in CCRCC.
Others:
- DOG1 +ve (Swalchick et al.[16] 32 +ve of 37 cases; Zhao et al.[17] 32 +ve of 32 cases).
- Useful in ChRCC versus clear cell RCC.
A panel:
- CK7, PAX8, CD117, CD10, Mueller-Mowry stain.
Comparison between some renal tumours with eosinophilic cytoplasm
| Tumour | CK7 | CD117 | GATA3 |
|---|---|---|---|
| Renal oncocytoma | -ve † | +ve | -ve/+ve |
| Chromophobe renal cell carcinoma | +ve ‡ | +ve | -ve |
| Low-grade oncocytic tumour | +ve | -ve | +ve |
† may have scattered positive cells
‡ diffuse and strong
Molecular
- Extensive aneusomy (monosomy?):[18]
- Loss of chromosomes: 1, 2, 6, 10, 13, 17, 21.
EM
Ultrastructural features:[19]
- Microvesicles.
- Complex plicated cell membrane.
Images
Sign out
KIDNEY, RIGHT UPPER POLE, PARTIAL NEPHRECTOMY: - CHROMOPHOBE RENAL CELL CARCINOMA. COMMENT: The sections show a mix of clear cells with wispy cytoplasm, and cells with eosinophilic cytoplasm and perinuclear halos. There are no true papillae. Stains and immunostains: Positive: CK7, CAM5.2, EMA, pankeratin, CD117, colloidal iron. Negative: AMACR, CD10, CD68, RCC, vimentin.
Micro
The sections show a sheeting tumour with abundant and eosinophilic cytoplasm. The tumour cell cell membranes are prominent and plant-like. Perinuclear clearing is present. Binucleation is frequent and the nuclear membranes moderately irregular. No definite papillae or macrophages are present. Nucleoli are not prominent. Small blood vessels are not prominent.
Alternate
The sections show a tumour composed of compact nests. The cytoplasm is abundant and eosinophilic. Perinuclear clearing is prominent. Binucleation is frequent and the nuclear membranes moderately irregular to round. No definite papillae or macrophages are present. Nucleoli are not prominent.
See also
References
- ↑ Delahunt, B.; Sika-Paotonu, D.; Bethwaite, PB.; McCredie, MR.; Martignoni, G.; Eble, JN.; Jordan, TW. (Jun 2007). "Fuhrman grading is not appropriate for chromophobe renal cell carcinoma.". Am J Surg Pathol 31 (6): 957-60. doi:10.1097/01.pas.0000249446.28713.53. PMID 17527087.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 290. ISBN 978-0781765275.
- ↑ Kuroda, N.; Tanaka, A.; Ohe, C.; Mikami, S.; Nagashima, Y.; Sasaki, T.; Inoue, K.; Hes, O. et al. (Nov 2012). "Review of renal oncocytosis (multiple oncocytic lesions) with focus on clinical and pathobiological aspects.". Histol Histopathol 27 (11): 1407-12. PMID 23018240.
- ↑ 4.0 4.1 4.2 4.3 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 293. ISBN 978-0443066771.
- ↑ Kuroda, N.; Toi, M.; Hiroi, M.; Enzan, H. (Jan 2003). "Review of chromophobe renal cell carcinoma with focus on clinical and pathobiological aspects.". Histol Histopathol 18 (1): 165-71. PMID 12507296.
- ↑ Siracusano, S.; Novara, G.; Antonelli, A.; Artibani, W.; Bertini, R.; Carini, M.; Carmignani, G.; Ciciliato, S. et al. (Dec 2012). "Prognostic role of tumour multifocality in renal cell carcinoma.". BJU Int 110 (11 Pt B): E443-8. doi:10.1111/j.1464-410X.2012.11121.x. PMID 22502873.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1016-7. ISBN 0-7216-0187-1.
- ↑ URL: http://www.ultrapath.org/oldsite/cases99/sep99/cotm9-2.html. Accessed on: 9 October 2011.
- ↑ Zhang, W.; Yu, WJ.; Jiang, YX.; Li, YJ.; Han, F.; Liu, Y.; Han, ZL. (Feb 2012). "[Chromophobe renal cell carcinoma: a clinicopathologic study and immunophenotypes of 42 cases].". Zhonghua Bing Li Xue Za Zhi 41 (2): 76-80. PMID 22455881.
- ↑ Din, NU.; Fatima, S.; Ahmad, Z. (Dec 2013). "Chromophobe renal cell carcinoma: a morphologic and immunohistochemical study of 45 cases.". Ann Diagn Pathol 17 (6): 508-13. doi:10.1016/j.anndiagpath.2013.06.005. PMID 24095630.
- ↑ Geramizadeh, B.; Ravanshad, M.; Rahsaz, M.. "Useful markers for differential diagnosis of oncocytoma, chromophobe renal cell carcinoma and conventional renal cell carcinoma.". Indian J Pathol Microbiol 51 (2): 167-71. PMID 18603673.
- ↑ Memeo L, Jhang J, Assaad AM, et al. (February 2007). "Immunohistochemical analysis for cytokeratin 7, KIT, and PAX2: value in the differential diagnosis of chromophobe cell carcinoma". Am. J. Clin. Pathol. 127 (2): 225–9. doi:10.1309/9KWEA4W9Y94D1AEE. PMID 17210525. http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17210525.
- ↑ Jain, S.; Roy, S.; Amin, M.; Acquafondata, M.; Yin, M.; Laframboise, W.; Bastacky, S.; Pantanowitz, L. et al. (Dec 2013). "Amylase α-1A (AMY1A): A Novel Immunohistochemical Marker to Differentiate Chromophobe Renal Cell Carcinoma From Benign Oncocytoma.". Am J Surg Pathol 37 (12): 1824-30. doi:10.1097/PAS.0000000000000108. PMID 24225843.
- ↑ Amin MB, Epstein JI, Ulbright TM, et al. (August 2014). "Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): 1017–22. doi:10.1097/PAS.0000000000000254. PMID 25025364.
- ↑ Al-Ahmadie HA, Alden D, Fine SW, et al. (July 2011). "Role of immunohistochemistry in the evaluation of needle core biopsies in adult renal cortical tumors: an ex vivo study". Am. J. Surg. Pathol. 35 (7): 949–61. doi:10.1097/PAS.0b013e31821e25cd. PMID 21677535.
- ↑ Swalchick, W.; Shamekh, R.; Bui, MM. (Oct 2015). "Is DOG1 Immunoreactivity Specific to Gastrointestinal Stromal Tumor?". Cancer Control 22 (4): 498-504. PMID 26678977.
- ↑ Zhao, W.; Tian, B.; Wu, C.; Peng, Y.; Wang, H.; Gu, WL.; Gao, FH. (Apr 2015). "DOG1, cyclin D1, CK7, CD117 and vimentin are useful immunohistochemical markers in distinguishing chromophobe renal cell carcinoma from clear cell renal cell carcinoma and renal oncocytoma.". Pathol Res Pract 211 (4): 303-7. doi:10.1016/j.prp.2014.12.014. PMID 25596994.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 292. ISBN 978-0781765275.
- ↑ 19.0 19.1 Lee, W. (Apr 2011). "Imprint cytology of the chromophobe renal cell carcinoma: Correlation with the histological and ultrastructural features.". J Cytol 28 (2): 77-80. doi:10.4103/0970-9371.80749. PMID 21713152.