Difference between revisions of "Orchiectomy grossing"
Jump to navigation
Jump to search
| (18 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
[[Image:Seminoma_of_the_Testis.jpg|thumb|150px|Orchiectomy specimen showing testis replaced by tumour (proven to be [[seminoma]]).]] | [[Image:Seminoma_of_the_Testis.jpg|thumb|150px|Orchiectomy specimen showing testis replaced by tumour (proven to be [[seminoma]]). (WC/Ed Uthman)]] | ||
This article deals with '''orchiectomy grossing'''. | This article deals with '''orchiectomy grossing'''. | ||
| Line 5: | Line 5: | ||
Orchiectomies are typically done for [[testicular tumours]]. | Orchiectomies are typically done for [[testicular tumours]]. | ||
They may be done for chronic pain or to control [[prostate cancer]]. | They may be done for chronic pain<ref name=pmid23929499>{{Cite journal | last1 = Rönkä | first1 = K. | last2 = Vironen | first2 = J. | last3 = Kokki | first3 = H. | last4 = Liukkonen | first4 = T. | last5 = Paajanen | first5 = H. | title = Role of orchiectomy in severe testicular pain after inguinal hernia surgery: audit of the Finnish Patient Insurance Centre. | journal = Hernia | volume = 19 | issue = 1 | pages = 53-9 | month = Feb | year = 2015 | doi = 10.1007/s10029-013-1150-3 | PMID = 23929499 }}</ref> or to control [[prostate cancer]]. Occasionally done in the context of a [[hernia repair]].<ref name=pmid3425809>{{cite journal |authors=Curtsinger LJ, Page CP, Aust JB |title=Orchiectomy during herniorrhaphy: what should we tell the patient? |journal=Am J Surg |volume=154 |issue=6 |pages=636–9 |date=December 1987 |pmid=3425809 |doi=10.1016/0002-9610(87)90232-7 |url=}}</ref> | ||
==Specimen opening== | |||
*Orient the specimen. | |||
**Follow cord to hilum of testis and [[epididymis]]. | |||
*Bisect the testis with one cut toward the hilum. | |||
**Do not cut through. | |||
**If tumour is a large do additional cuts parallel to the first cut to ensure proper [[fixation]]. | |||
*Place specimen(s) in [[formalin]]. | |||
Note: | |||
*Cutting easier if blade wet before cutting. | |||
*[[Marking ink|Inking]] the cord at the margin and mid section of the cord in different colours allows one to reconstruct the location if one has to go back to the gross. | |||
==Protocol== | ==Protocol== | ||
| Line 46: | Line 58: | ||
====Staging==== | ====Staging==== | ||
{{Main|Testicular cancer staging}} | |||
Based on AJCC 7th Edition:<ref>URL: [https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging]. Accessed on: 15 December 2014.</ref><ref name=cancer_org>URL: [http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging]. Accessed on: 15 December 2014.</ref> | Based on AJCC 7th Edition:<ref>URL: [https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging]. Accessed on: 15 December 2014.</ref><ref name=cancer_org>URL: [http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging]. Accessed on: 15 December 2014.</ref> | ||
*pT1 - confined to the testis or epididymis, no [[lymphovascular invasion]]. | *pT1 - confined to the testis or epididymis, no [[lymphovascular invasion]]. | ||
*pT2 - into tunica vaginalis or lymphovascular invasion. | *pT2 - into tunica vaginalis or lymphovascular invasion. | ||
*pT3 - into spermatic cord. | *pT3 - into [[spermatic cord]]. | ||
*pT4 - into the [[scrotum]]. | *pT4 - into the [[scrotum]]. | ||
===Alternate approaches=== | ===Alternate approaches=== | ||
==See also== | ==See also== | ||
*[[Testicular cancer staging]]. | |||
===Related protocols=== | ===Related protocols=== | ||
==References== | ==References== | ||
{{Reflist|1}} | {{Reflist|1}} | ||
Latest revision as of 18:04, 27 September 2024
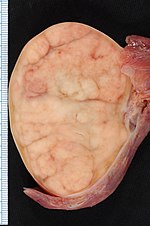
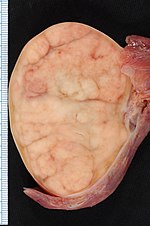
Orchiectomy specimen showing testis replaced by tumour (proven to be seminoma). (WC/Ed Uthman)
This article deals with orchiectomy grossing.
Introduction
Orchiectomies are typically done for testicular tumours.
They may be done for chronic pain[1] or to control prostate cancer. Occasionally done in the context of a hernia repair.[2]
Specimen opening
- Orient the specimen.
- Follow cord to hilum of testis and epididymis.
- Bisect the testis with one cut toward the hilum.
- Do not cut through.
- If tumour is a large do additional cuts parallel to the first cut to ensure proper fixation.
- Place specimen(s) in formalin.
Note:
- Cutting easier if blade wet before cutting.
- Inking the cord at the margin and mid section of the cord in different colours allows one to reconstruct the location if one has to go back to the gross.
Protocol
Dimensions and weight:
- Laterality: [ left / right ].
- Weight: ___ grams.
- Testis: ___ x ___ x ___ cm.
- Epididymis: ___ x ___ x ___ cm.
- Spermatic cord - length: __ cm, diameter: ___ cm.
- Inking: [colour].
Tumour:
- Size: ___ x ___ x ___ cm.
- Colour: [ tan / white / variable ].
- Firmness: [ firm / soft ].
- Morphology: [solid / cystic / solid and cystic - with ___ % cystic].
- Circumscription: [circumscribed / infiltrative border ].
- Hemorrhage: [ absent / present ].
- Necrosis: [ absent / present ].
- Extension into tunica albuginea: [ not identified / indeterminate / present ].
- Extension into the epididymis: [ not identified / indeterminate / present ].
Other - after sectioning:
- Testicular parenchyma: [ brown-tan, unremarkable / ___ ].
- Spermatic cord: [ unremarkable / ___ ].
Representative sections are submitted as follow:
- Spermatic cord resection margin, en face.
- Spermatic cord mid-section, cross section.
- Spermatic cord close to testis.
- Tumour in relation to epididymis.
- Tumour and rete testis.
- Tumour with testicular coverings.
- Additional tumour sections.
- Testis distant from the tumour.
Protocol notes
- The tumour should be submitted in total if this can be done in less than 10 cassettes.
- Lester's book (2nd Ed.) recommends 1 cassette per cm of maximal tumour dimension.[3]
Staging
Main article: Testicular cancer staging
Based on AJCC 7th Edition:[4][5]
- pT1 - confined to the testis or epididymis, no lymphovascular invasion.
- pT2 - into tunica vaginalis or lymphovascular invasion.
- pT3 - into spermatic cord.
- pT4 - into the scrotum.
Alternate approaches
See also
Related protocols
References
- ↑ Rönkä, K.; Vironen, J.; Kokki, H.; Liukkonen, T.; Paajanen, H. (Feb 2015). "Role of orchiectomy in severe testicular pain after inguinal hernia surgery: audit of the Finnish Patient Insurance Centre.". Hernia 19 (1): 53-9. doi:10.1007/s10029-013-1150-3. PMID 23929499.
- ↑ Curtsinger LJ, Page CP, Aust JB (December 1987). "Orchiectomy during herniorrhaphy: what should we tell the patient?". Am J Surg 154 (6): 636–9. doi:10.1016/0002-9610(87)90232-7. PMID 3425809.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 409. ISBN 978-0443066450.
- ↑ URL: https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging. Accessed on: 15 December 2014.
- ↑ URL: http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging. Accessed on: 15 December 2014.