Difference between revisions of "Papillary renal cell carcinoma"
(→Images) |
|||
| (42 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
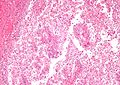
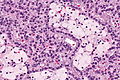
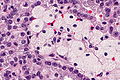
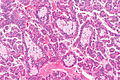
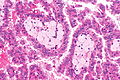
| Caption = Papillary renal cell carcinoma. [[H&E stain]]. | | Caption = Papillary renal cell carcinoma. [[H&E stain]]. | ||
| Micro = cuboidal or low columnar cells (simple or pseudostratified) on papillae, interstitial foam cells in the vascular cores | | Micro = cuboidal or low columnar cells (simple or pseudostratified) on papillae, interstitial foam cells in the vascular cores | ||
| Subtypes = type 1 | | Subtypes = no ''World Health Organization'' recognized subtypes; defunct subtypes: "type 1" and "type 2", oncocytic variant | ||
| LMDDx = [[clear cell renal cell carcinoma]], [[clear cell papillary renal cell carcinoma]], [[metanephric adenoma]] (esp. solid | | LMDDx = [[clear cell renal cell carcinoma]], [[clear cell papillary renal cell carcinoma]], [[metanephric adenoma]] (esp. solid PaRCC type 1), [[collecting duct carcinoma]] (esp. PaRCC type 2), [[renal papillary adenoma]], [[acquired cystic disease-associated renal cell carcinoma]], [[urothelial carcinoma]], [[renal mucinous tubular and spindle cell carcinoma]], [[ALK translocation renal cell carcinoma]], [[Xp11 translocation renal cell carcinoma]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = MET mutation (hereditary papillary renal cell carcinoma), FH mutation (hereditary leiomyomatosis and renal cell cancer) | ||
| IF = | | IF = | ||
| Gross = may be multifocal, must be > | | Gross = may be multifocal, must be >1.5 cm (if low ISUP grade), often necrotic-appearing (brown, soft, friable) | ||
| | | Grossing = [[total nephrectomy for tumour grossing]], [[partial nephrectomy grossing]] | ||
| Staging = [[kidney cancer staging]] | |||
| Site = [[kidney]] - see [[kidney tumours]] | | Site = [[kidney]] - see [[kidney tumours]] | ||
| Assdx = [[acquired renal cystic disease]] ([[end-stage renal disease]]) | | Assdx = [[acquired renal cystic disease]] ([[end-stage renal disease]]) | ||
| Syndromes = hereditary papillary renal cell carcinoma | | Syndromes = hereditary papillary renal cell carcinoma, [[hereditary leiomyomatosis and renal cell cancer]] | ||
| Clinicalhx = | | Clinicalhx = | ||
| Signs = | | Signs = | ||
| Line 32: | Line 33: | ||
==General== | ==General== | ||
* | *Historically, PaRCC was subclassified<ref name=Ref_GUP289>{{Ref GUP|289}}</ref> into ''type 1'' and ''type 2''. | ||
**Type 1 and Type 2 are different on a cytogenetic and molecular basis.<ref>{{Cite journal | last1 = Klatte | first1 = T. | last2 = Pantuck | first2 = AJ. | last3 = Said | first3 = JW. | last4 = Seligson | first4 = DB. | last5 = Rao | first5 = NP. | last6 = LaRochelle | first6 = JC. | last7 = Shuch | first7 = B. | last8 = Zisman | first8 = A. | last9 = Kabbinavar | first9 = FF. | title = Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma. | journal = Clin Cancer Res | volume = 15 | issue = 4 | pages = 1162-9 | month = Feb | year = 2009 | doi = 10.1158/1078-0432.CCR-08-1229 | PMID = 19228721 }}</ref> | **Type 1 and Type 2 are different on a cytogenetic and molecular basis.<ref>{{Cite journal | last1 = Klatte | first1 = T. | last2 = Pantuck | first2 = AJ. | last3 = Said | first3 = JW. | last4 = Seligson | first4 = DB. | last5 = Rao | first5 = NP. | last6 = LaRochelle | first6 = JC. | last7 = Shuch | first7 = B. | last8 = Zisman | first8 = A. | last9 = Kabbinavar | first9 = FF. | title = Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma. | journal = Clin Cancer Res | volume = 15 | issue = 4 | pages = 1162-9 | month = Feb | year = 2009 | doi = 10.1158/1078-0432.CCR-08-1229 | PMID = 19228721 }}</ref> | ||
| Line 38: | Line 39: | ||
*Associated with ''[[acquired renal cystic disease]]''.<ref name=Ref_DARP438>{{Ref DARP|438}}</ref> | *Associated with ''[[acquired renal cystic disease]]''.<ref name=Ref_DARP438>{{Ref DARP|438}}</ref> | ||
*May be familial - uncommon.<ref name=pmid12629341>{{Cite journal | last1 = Czene | first1 = K. | last2 = Hemminki | first2 = K. | title = Familial papillary renal cell tumors and subsequent cancers: a nationwide epidemiological study from Sweden. | journal = J Urol | volume = 169 | issue = 4 | pages = 1271-5 | month = Apr | year = 2003 | doi = 10.1097/01.ju.0000052373.36963.12 | PMID = 12629341 }}</ref> | *May be familial - uncommon.<ref name=pmid12629341>{{Cite journal | last1 = Czene | first1 = K. | last2 = Hemminki | first2 = K. | title = Familial papillary renal cell tumors and subsequent cancers: a nationwide epidemiological study from Sweden. | journal = J Urol | volume = 169 | issue = 4 | pages = 1271-5 | month = Apr | year = 2003 | doi = 10.1097/01.ju.0000052373.36963.12 | PMID = 12629341 }}</ref> | ||
**MET mutation<ref name=pmid22717761>{{Cite journal | last1 = Wadt | first1 = KA. | last2 = Gerdes | first2 = AM. | last3 = Hansen | first3 = TV. | last4 = Toft | first4 = BG. | last5 = Friis-Hansen | first5 = L. | last6 = Andersen | first6 = MK. | title = Novel germline c-MET mutation in a family with hereditary papillary renal carcinoma. | journal = Fam Cancer | volume = 11 | issue = 3 | pages = 535-7 | month = Sep | year = 2012 | doi = 10.1007/s10689-012-9542-6 | PMID = 22717761 }}</ref> - autosomal dominant transmission | **MET mutation<ref name=pmid22717761>{{Cite journal | last1 = Wadt | first1 = KA. | last2 = Gerdes | first2 = AM. | last3 = Hansen | first3 = TV. | last4 = Toft | first4 = BG. | last5 = Friis-Hansen | first5 = L. | last6 = Andersen | first6 = MK. | title = Novel germline c-MET mutation in a family with hereditary papillary renal carcinoma. | journal = Fam Cancer | volume = 11 | issue = 3 | pages = 535-7 | month = Sep | year = 2012 | doi = 10.1007/s10689-012-9542-6 | PMID = 22717761 }}</ref> - autosomal dominant transmission (previously ''PaRCC type 1''). | ||
==Gross== | ==Gross== | ||
*Renal cortical mass > | *Renal cortical mass usually >1.5 cm. | ||
*May be multifocal. | *May be multifocal. ‡ | ||
*Often necrotic appearing - light-to-dark brown, soft/mushy, friable. | |||
Note: | |||
*‡ Approximately 10% of PaRCCs are multifocal (based on a set of 5378 patients);<ref name=pmid22502873>{{Cite journal | last1 = Siracusano | first1 = S. | last2 = Novara | first2 = G. | last3 = Antonelli | first3 = A. | last4 = Artibani | first4 = W. | last5 = Bertini | first5 = R. | last6 = Carini | first6 = M. | last7 = Carmignani | first7 = G. | last8 = Ciciliato | first8 = S. | last9 = Cunico | first9 = SC. | title = Prognostic role of tumour multifocality in renal cell carcinoma. | journal = BJU Int | volume = 110 | issue = 11 Pt B | pages = E443-8 | month = Dec | year = 2012 | doi = 10.1111/j.1464-410X.2012.11121.x | PMID = 22502873 }}</ref> it is the renal tumour that is most commonly multifocal. | |||
==Microscopic== | ==Microscopic== | ||
| Line 48: | Line 53: | ||
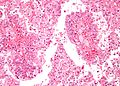
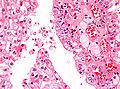
*Cuboidal or low columnar cell in papillae. | *Cuboidal or low columnar cell in papillae. | ||
*Interstitial foam cells in vascular cores - '''key feature'''. | *Interstitial foam cells in vascular cores - '''key feature'''. | ||
**Most sensitive and specific feature of | **Most sensitive and specific feature of PaRCC.<ref>{{cite journal |author=Granter SR, Perez-Atayde AR, Renshaw AA |title=Cytologic analysis of papillary renal cell carcinoma |journal=Cancer |volume=84 |issue=5 |pages=303?8 |year=1998 |month=October |pmid=9801205 |doi= |url=http://dx.doi.org/10.1002/(SICI)1097-0142(19981025)84:5<303::AID-CNCR6>3.0.CO;2-7}}</ref> | ||
*Highly vascular. | *Highly vascular. | ||
Size criterion: | Size criterion: | ||
*Papillary lesions '''''must''''' be > | *Papillary lesions with low [[ISUP nucleolar grade|ISUP grade]] '''''must''''' be >1.5 cm to be called ''carcinoma''; smaller lesions (<=1.5 cm) with low ISUP grade are called ''[[renal papillary adenoma|papillary adenoma]]s''.<ref name=pmid26935559>{{Cite journal | last1 = Moch | first1 = H. | last2 = Cubilla | first2 = AL. | last3 = Humphrey | first3 = PA. | last4 = Reuter | first4 = VE. | last5 = Ulbright | first5 = TM. | title = The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. | journal = Eur Urol | volume = | issue = | pages = | month = Feb | year = 2016 | doi = 10.1016/j.eururo.2016.02.029 | PMID = 26935559 }}</ref><ref name=Ref_GUP288>{{Ref GUP|288}}</ref> † | ||
Mnemonic ''HIP'': '''h'''ighly vascular, '''i'''nterstitial foam cells, '''p'''apillae. | Mnemonic ''HIP'': '''h'''ighly vascular, '''i'''nterstitial foam cells, '''p'''apillae. | ||
Note: | |||
*† The [[diagnostic size cut-off]] in the 2004 [[WHO]] GU (blue) book was 0.5 cm.<ref name=pmid26935559/><ref>{{Ref WHOGU|28}}</ref> | |||
DDx: | DDx: | ||
*[[Clear cell RCC]]. | *[[Clear cell RCC]]. | ||
**Papillary: | **Papillary: histiocytes, intracellular hemosiderin, [[CK7]] +ve. | ||
*[[Clear cell papillary renal cell carcinoma]]. | *[[Clear cell papillary renal cell carcinoma]] - apical nuclei, usu. no true papillae. | ||
*[[Metanephric adenoma]] | *[[Metanephric adenoma]] (esp. solid PaRCC type 1) - no histiocytes, WT-1 +ve. | ||
*[[Collecting duct carcinoma]] - esp. | *[[Collecting duct carcinoma]] - esp. PaRCC type 2. | ||
*[[Renal papillary adenoma]]. | *[[Urothelial carcinoma]]. | ||
*[[Renal papillary adenoma]] - doesn't fulfill size criterion for PaRCC. | |||
*[[Acquired cystic disease-associated renal cell carcinoma]]. | |||
*[[Renal mucinous tubular and spindle cell carcinoma]]. | |||
*[[Hereditary leiomyomatosis and renal cell carcinoma syndrome-associated renal cell carcinoma]] - for ''type 2 PaRCC''; CK7 -ve, prominent eosinophilic nucleoli. | |||
*[[ALK translocation renal cell carcinoma]]. | |||
*[[Mixed epithelial and stromal tumour]].<ref name=pmid31862520>{{cite journal |authors=Rogala J, Kojima F, Alaghehbandan R, Agaimy A, Martinek P, Ondic O, Ulamec M, Sperga M, Michalova K, Pivovarcikova K, Pitra T, Hora M, Ferak I, Marečková J, Michal M, Hes O |title=Papillary renal cell carcinoma with prominent spindle cell stroma - tumor mimicking mixed epithelial and stromal tumor of the kidney: Clinicopathologic, morphologic, immunohistochemical and molecular genetic analysis of 6 cases |journal=Ann Diagn Pathol |volume=44 |issue= |pages=151441 |date=February 2020 |pmid=31862520 |doi=10.1016/j.anndiagpath.2019.151441 |url=}}</ref> | |||
*[[Papillary renal neoplasm with reverse polarity]] (PRNRP) - nuclei at luminal aspect of cell (rather than closer to the basement membrane).<ref name=pmid31135486>{{cite journal |authors=Al-Obaidy KI, Eble JN, Cheng L, Williamson SR, Sakr WA, Gupta N, Idrees MT, Grignon DJ |title=Papillary Renal Neoplasm With Reverse Polarity: A Morphologic, Immunohistochemical, and Molecular Study |journal=Am J Surg Pathol |volume=43 |issue=8 |pages=1099–1111 |date=August 2019 |pmid=31135486 |doi=10.1097/PAS.0000000000001288 |url=}}</ref> | |||
**May be considered a subtype of papillary renal cell carcinoma (rather than a distinct entity). | |||
*[[Xp11 translocation renal cell carcinoma]]. | |||
===Images=== | ===Images=== | ||
| Line 81: | Line 98: | ||
===Histological subtyping=== | ===Histological subtyping=== | ||
Historically, PaRCC was subtyped:<ref name=Ref_GUP289>{{Ref GUP|289}}</ref><ref>{{Cite journal | last1 = Delahunt | first1 = B. | last2 = Eble | first2 = JN. | title = Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study of 105 tumors. | journal = Mod Pathol | volume = 10 | issue = 6 | pages = 537-44 | month = Jun | year = 1997 | doi = | PMID = 9195569 }}</ref> | |||
*''Type 1'' - single layer of cells on basement membrane - '''most important'''. | *''Type 1'' - single layer of cells on basement membrane - '''most important'''. | ||
** Usually low grade nuclear features, i.e. low | ** Usually low grade nuclear features, i.e. low [[ISUP nucleolar grade]]. | ||
** Other characteristics: | ** Other characteristics: | ||
*** Clear cytoplasm. | *** Clear cytoplasm. | ||
| Line 89: | Line 106: | ||
*** Cells smaller. | *** Cells smaller. | ||
*''Type 2'' - pseudostratification of cells - '''most important'''. | *''Type 2'' - pseudostratification of cells - '''most important'''. | ||
** Usually high grade nuclear features, i.e. high | ** Usually high grade nuclear features, i.e. high [[ISUP nucleolar grade]]. | ||
** Other characteristics: | ** Other characteristics: | ||
*** Eosinophilic cytoplasm. | *** Eosinophilic cytoplasm. | ||
*** Foamy macrophages - uncommon. | *** Foamy macrophages - uncommon. | ||
*** Cells larger. | *** Cells larger. | ||
The WHO GU Blue Book 5th Ed. recommends against subtyping. | |||
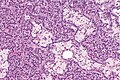
Another subtype: | Another subtype: | ||
*''Oncocytic'' - oncocytic cytoplasm. | *''Oncocytic'' - oncocytic cytoplasm. | ||
**Extremely rare ~ | **Extremely rare ~ a few dozen reported.<ref name=pmid19494850 >{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref><ref name=pmid16730306>{{Cite journal | last1 = Hes | first1 = O. | last2 = Brunelli | first2 = M. | last3 = Michal | first3 = M. | last4 = Cossu Rocca | first4 = P. | last5 = Hora | first5 = M. | last6 = Chilosi | first6 = M. | last7 = Mina | first7 = M. | last8 = Boudova | first8 = L. | last9 = Menestrina | first9 = F. | title = Oncocytic papillary renal cell carcinoma: a clinicopathologic, immunohistochemical, ultrastructural, and interphase cytogenetic study of 12 cases. | journal = Ann Diagn Pathol | volume = 10 | issue = 3 | pages = 133-9 | month = Jun | year = 2006 | doi = 10.1016/j.anndiagpath.2005.12.002 | PMID = 16730306 }}</ref> | ||
***One "large" series was 14 cases.<ref name=pmid27931799>{{Cite journal | last1 = Han | first1 = G. | last2 = Yu | first2 = W. | last3 = Chu | first3 = J. | last4 = Liu | first4 = Y. | last5 = Jiang | first5 = Y. | last6 = Li | first6 = Y. | last7 = Zhang | first7 = W. | title = Oncocytic papillary renal cell carcinoma: A clinicopathological and genetic analysis and indolent clinical course in 14 cases. | journal = Pathol Res Pract | volume = 213 | issue = 1 | pages = 1-6 | month = Jan | year = 2017 | doi = 10.1016/j.prp.2016.04.009 | PMID = 27931799 }}</ref> | |||
==IHC== | ==IHC== | ||
| Line 105: | Line 125: | ||
*Panker (AE1/AE3) +ve. | *Panker (AE1/AE3) +ve. | ||
*CK7 +ve ~90% of type 1, 20% of type 2. | *CK7 +ve ~90% of type 1, 20% of type 2. | ||
*CD10 +ve.<ref>[http://surgpathcriteria.stanford.edu/kidney/papillary-renal-cell-carcinoma/differential-diagnosis.html http://surgpathcriteria.stanford.edu/kidney/papillary-renal-cell-carcinoma/differential-diagnosis.html]. Accessed on: 6 May 2014.</ref> | |||
Others: | |||
* | *GATA3 +ve - oncocytic variant of PaRCC; negative in other PaRCC subtypes.<ref name=pmid28984673>{{cite journal |authors=Saleeb RM, Brimo F, Farag M, Rompré-Brodeur A, Rotondo F, Beharry V, Wala S, Plant P, Downes MR, Pace K, Evans A, Bjarnason G, Bartlett JMS, Yousef GM |title=Toward Biological Subtyping of Papillary Renal Cell Carcinoma With Clinical Implications Through Histologic, Immunohistochemical, and Molecular Analysis |journal=Am J Surg Pathol |volume=41 |issue=12 |pages=1618–1629 |date=December 2017 |pmid=28984673 |doi=10.1097/PAS.0000000000000962 |url=}}</ref> | ||
Type 1 versus Type 2:<ref name=pmid9234615>{{Cite journal | last1 = Ono | first1 = Y. | last2 = Ito | first2 = T. | last3 = Tsujino | first3 = S. | last4 = Aizawa | first4 = S. | last5 = Suzuki | first5 = M. | title = [A study of papillary renal cell carcinoma. Clinicopathological, immunohistochemical features and its typing]. | journal = Nihon Hinyokika Gakkai Zasshi | volume = 88 | issue = 6 | pages = 587-95 | month = Jun | year = 1997 | doi = | PMID = 9234615 }}</ref> | Type 1 versus Type 2:<ref name=pmid9234615>{{Cite journal | last1 = Ono | first1 = Y. | last2 = Ito | first2 = T. | last3 = Tsujino | first3 = S. | last4 = Aizawa | first4 = S. | last5 = Suzuki | first5 = M. | title = [A study of papillary renal cell carcinoma. Clinicopathological, immunohistochemical features and its typing]. | journal = Nihon Hinyokika Gakkai Zasshi | volume = 88 | issue = 6 | pages = 587-95 | month = Jun | year = 1997 | doi = | PMID = 9234615 }}</ref> | ||
| Line 132: | Line 153: | ||
==Sign out== | ==Sign out== | ||
<pre> | |||
Kidney Tumour, Left, Partial Nephrectomy: | |||
- PAPILLARY RENAL CELL CARCINOMA. | |||
-- Surgical margins NEGATIVE. | |||
-- ISUP nucleolar (Fuhrman) Grade 3. | |||
-- TNM stage: pT1a pNx. | |||
-- Please see tumour summary. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
KIDNEY, RIGHT, RADICAL NEPHRECTOMY: | KIDNEY, RIGHT, RADICAL NEPHRECTOMY: | ||
- PAPILLARY RENAL CELL CARCINOMA, | - PAPILLARY RENAL CELL CARCINOMA, WHO/ISUP NUCLEOLAR GRADE 3, pT2a(2), pNx. | ||
-- SURGICAL MARGINS NEGATIVE. | -- SURGICAL MARGINS NEGATIVE. | ||
-- PLEASE SEE TUMOUR SUMMARY. | -- PLEASE SEE TUMOUR SUMMARY. | ||
| Line 145: | Line 176: | ||
The papillae predominantly have a single layer of tumour cells and the cytoplasm of the tumour cells is predominantly clear. | The papillae predominantly have a single layer of tumour cells and the cytoplasm of the tumour cells is predominantly clear. | ||
Nucleoli are visible focally with the 10x objective ( | Nucleoli are visible focally with the 10x objective (ISUP nucleolar grade 3). | ||
A second tumour with the same morphology is present and measures 8 millimetres. | A second tumour with the same morphology is present and measures 8 millimetres. | ||
Multiple small lesions, like the largest tumour, less than | Multiple small lesions, like the largest tumour, less than 1.5 cm are present. | ||
===Oncocytic variant=== | ===Oncocytic variant=== | ||
| Line 155: | Line 186: | ||
KIDNEY, RIGHT, NEPHRECTOMY: | KIDNEY, RIGHT, NEPHRECTOMY: | ||
- PAPILLARY RENAL CELL CARCINOMA, ONCOCYTIC -- SEE COMMENT; | - PAPILLARY RENAL CELL CARCINOMA, ONCOCYTIC -- SEE COMMENT; | ||
- | - WHO/ISUP GRADE 2; | ||
- SURGICAL MARGINS NEGATIVE; | - SURGICAL MARGINS NEGATIVE; | ||
- PLEASE SEE TUMOUR SUMMARY. | - PLEASE SEE TUMOUR SUMMARY. | ||
| Line 177: | Line 208: | ||
[[Category:Kidney tumours]] | [[Category:Kidney tumours]] | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Papillary tumour]] | |||
Latest revision as of 00:02, 20 March 2024
| Papillary renal cell carcinoma | |
|---|---|
| Diagnosis in short | |
 Papillary renal cell carcinoma. H&E stain. | |
|
| |
| LM | cuboidal or low columnar cells (simple or pseudostratified) on papillae, interstitial foam cells in the vascular cores |
| Subtypes | no World Health Organization recognized subtypes; defunct subtypes: "type 1" and "type 2", oncocytic variant |
| LM DDx | clear cell renal cell carcinoma, clear cell papillary renal cell carcinoma, metanephric adenoma (esp. solid PaRCC type 1), collecting duct carcinoma (esp. PaRCC type 2), renal papillary adenoma, acquired cystic disease-associated renal cell carcinoma, urothelial carcinoma, renal mucinous tubular and spindle cell carcinoma, ALK translocation renal cell carcinoma, Xp11 translocation renal cell carcinoma |
| Molecular | MET mutation (hereditary papillary renal cell carcinoma), FH mutation (hereditary leiomyomatosis and renal cell cancer) |
| Gross | may be multifocal, must be >1.5 cm (if low ISUP grade), often necrotic-appearing (brown, soft, friable) |
| Grossing notes | total nephrectomy for tumour grossing, partial nephrectomy grossing |
| Staging | kidney cancer staging |
| Site | kidney - see kidney tumours |
|
| |
| Associated Dx | acquired renal cystic disease (end-stage renal disease) |
| Syndromes | hereditary papillary renal cell carcinoma, hereditary leiomyomatosis and renal cell cancer |
|
| |
| Prevalence | relatively common |
| Clin. DDx | other kidney tumours |
| Treatment | surgical excision, ablation |
Papillary renal cell carcinoma, abbreviated PRCC, PaRCC and papillary RCC, is the second most common type of renal cell carcinoma.
General
- Historically, PaRCC was subclassified[1] into type 1 and type 2.
- Type 1 and Type 2 are different on a cytogenetic and molecular basis.[2]
Epidemiology
- Associated with acquired renal cystic disease.[3]
- May be familial - uncommon.[4]
- MET mutation[5] - autosomal dominant transmission (previously PaRCC type 1).
Gross
- Renal cortical mass usually >1.5 cm.
- May be multifocal. ‡
- Often necrotic appearing - light-to-dark brown, soft/mushy, friable.
Note:
- ‡ Approximately 10% of PaRCCs are multifocal (based on a set of 5378 patients);[6] it is the renal tumour that is most commonly multifocal.
Microscopic
Features:[7]
- Cuboidal or low columnar cell in papillae.
- Interstitial foam cells in vascular cores - key feature.
- Most sensitive and specific feature of PaRCC.[8]
- Highly vascular.
Size criterion:
- Papillary lesions with low ISUP grade must be >1.5 cm to be called carcinoma; smaller lesions (<=1.5 cm) with low ISUP grade are called papillary adenomas.[9][10] †
Mnemonic HIP: highly vascular, interstitial foam cells, papillae.
Note:
- † The diagnostic size cut-off in the 2004 WHO GU (blue) book was 0.5 cm.[9][11]
DDx:
- Clear cell RCC.
- Papillary: histiocytes, intracellular hemosiderin, CK7 +ve.
- Clear cell papillary renal cell carcinoma - apical nuclei, usu. no true papillae.
- Metanephric adenoma (esp. solid PaRCC type 1) - no histiocytes, WT-1 +ve.
- Collecting duct carcinoma - esp. PaRCC type 2.
- Urothelial carcinoma.
- Renal papillary adenoma - doesn't fulfill size criterion for PaRCC.
- Acquired cystic disease-associated renal cell carcinoma.
- Renal mucinous tubular and spindle cell carcinoma.
- Hereditary leiomyomatosis and renal cell carcinoma syndrome-associated renal cell carcinoma - for type 2 PaRCC; CK7 -ve, prominent eosinophilic nucleoli.
- ALK translocation renal cell carcinoma.
- Mixed epithelial and stromal tumour.[12]
- Papillary renal neoplasm with reverse polarity (PRNRP) - nuclei at luminal aspect of cell (rather than closer to the basement membrane).[13]
- May be considered a subtype of papillary renal cell carcinoma (rather than a distinct entity).
- Xp11 translocation renal cell carcinoma.
Images
Histological subtyping
Historically, PaRCC was subtyped:[1][14]
- Type 1 - single layer of cells on basement membrane - most important.
- Usually low grade nuclear features, i.e. low ISUP nucleolar grade.
- Other characteristics:
- Clear cytoplasm.
- Foamy macrophages - common.
- Cells smaller.
- Type 2 - pseudostratification of cells - most important.
- Usually high grade nuclear features, i.e. high ISUP nucleolar grade.
- Other characteristics:
- Eosinophilic cytoplasm.
- Foamy macrophages - uncommon.
- Cells larger.
The WHO GU Blue Book 5th Ed. recommends against subtyping.
Another subtype:
- Oncocytic - oncocytic cytoplasm.
IHC
Features:[1]
- AMACR +ve.
- HMWCK (34betaE12) +ve.
- Panker (AE1/AE3) +ve.
- CK7 +ve ~90% of type 1, 20% of type 2.
- CD10 +ve.[18]
Others:
- GATA3 +ve - oncocytic variant of PaRCC; negative in other PaRCC subtypes.[19]
Type 1 versus Type 2:[20]
- CK7:
- Type 1 ~ 100%.
- Type 2 ~ 19%.
- CK19:
- Type 1 ~ 100%.
- Type 2 ~ 53%.
Metanephric adenoma vs. PaRCC type 1:[21]
- AMACR +ve.
- WT-1 -ve.
- CD57 -ve.
Molecular
Features:[22]
- Sporadic: trisomies 7, 16, 17.
- Familial: trisomy 7.
- Chromosome 7 = location of MET gene.
Note:
- Not used for diagnosis.[23]
Sign out
Kidney Tumour, Left, Partial Nephrectomy: - PAPILLARY RENAL CELL CARCINOMA. -- Surgical margins NEGATIVE. -- ISUP nucleolar (Fuhrman) Grade 3. -- TNM stage: pT1a pNx. -- Please see tumour summary.
Block letters
KIDNEY, RIGHT, RADICAL NEPHRECTOMY: - PAPILLARY RENAL CELL CARCINOMA, WHO/ISUP NUCLEOLAR GRADE 3, pT2a(2), pNx. -- SURGICAL MARGINS NEGATIVE. -- PLEASE SEE TUMOUR SUMMARY. - RENAL PAPILLARY ADENOMAS.
Micro
The sections show a tumour in the kidney with fibrovascular cores (papillae) that focally contain macrophages. Psammoma bodies are present. Siderophages are present.
The papillae predominantly have a single layer of tumour cells and the cytoplasm of the tumour cells is predominantly clear.
Nucleoli are visible focally with the 10x objective (ISUP nucleolar grade 3).
A second tumour with the same morphology is present and measures 8 millimetres.
Multiple small lesions, like the largest tumour, less than 1.5 cm are present.
Oncocytic variant
KIDNEY, RIGHT, NEPHRECTOMY: - PAPILLARY RENAL CELL CARCINOMA, ONCOCYTIC -- SEE COMMENT; - WHO/ISUP GRADE 2; - SURGICAL MARGINS NEGATIVE; - PLEASE SEE TUMOUR SUMMARY. COMMENT: The oncocytic variant of papillary renal cell carcinoma (RCC) is uncommon and not widely recognized as a subtype of papillary RCC. The prognostic significance of the oncocytic cytoplasm is uncertain.[1] The histomorphology in this case is compatible with a type 1 papillary RCC. 1. Ann Diagn Pathol. 2006 Jun;10(3):133-9.
See also
References
- ↑ 1.0 1.1 1.2 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 289. ISBN 978-0443066771.
- ↑ Klatte, T.; Pantuck, AJ.; Said, JW.; Seligson, DB.; Rao, NP.; LaRochelle, JC.; Shuch, B.; Zisman, A. et al. (Feb 2009). "Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma.". Clin Cancer Res 15 (4): 1162-9. doi:10.1158/1078-0432.CCR-08-1229. PMID 19228721.
- ↑ Fogo, Agnes B.; Kashgarian, Michael (2005). Diagnostic Atlas of Renal Pathology: A Companion to Brenner and Rector's The Kidney 7E (1st ed.). Saunders. pp. 438. ISBN 978-1416028710.
- ↑ Czene, K.; Hemminki, K. (Apr 2003). "Familial papillary renal cell tumors and subsequent cancers: a nationwide epidemiological study from Sweden.". J Urol 169 (4): 1271-5. doi:10.1097/01.ju.0000052373.36963.12. PMID 12629341.
- ↑ Wadt, KA.; Gerdes, AM.; Hansen, TV.; Toft, BG.; Friis-Hansen, L.; Andersen, MK. (Sep 2012). "Novel germline c-MET mutation in a family with hereditary papillary renal carcinoma.". Fam Cancer 11 (3): 535-7. doi:10.1007/s10689-012-9542-6. PMID 22717761.
- ↑ Siracusano, S.; Novara, G.; Antonelli, A.; Artibani, W.; Bertini, R.; Carini, M.; Carmignani, G.; Ciciliato, S. et al. (Dec 2012). "Prognostic role of tumour multifocality in renal cell carcinoma.". BJU Int 110 (11 Pt B): E443-8. doi:10.1111/j.1464-410X.2012.11121.x. PMID 22502873.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1017-8. ISBN 0-7216-0187-1.
- ↑ Granter SR, Perez-Atayde AR, Renshaw AA (October 1998). <303::AID-CNCR6>3.0.CO;2-7 "Cytologic analysis of papillary renal cell carcinoma". Cancer 84 (5): 303?8. PMID 9801205. http://dx.doi.org/10.1002/(SICI)1097-0142(19981025)84:5<303::AID-CNCR6>3.0.CO;2-7.
- ↑ 9.0 9.1 Moch, H.; Cubilla, AL.; Humphrey, PA.; Reuter, VE.; Ulbright, TM. (Feb 2016). "The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours.". Eur Urol. doi:10.1016/j.eururo.2016.02.029. PMID 26935559.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 288. ISBN 978-0443066771.
- ↑ The International Agency for Research on Cancer (Author), J. Eble (Editor), J. Epstein (Editor), I. Sesterhenn (Editor), G. Sauter (Editor) (2004). Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs (IARC WHO Classification of Tumours) (1st ed.). Lyon: World Health Organization. pp. 28. ISBN 978-9283224150.
- ↑ Rogala J, Kojima F, Alaghehbandan R, Agaimy A, Martinek P, Ondic O, Ulamec M, Sperga M, Michalova K, Pivovarcikova K, Pitra T, Hora M, Ferak I, Marečková J, Michal M, Hes O (February 2020). "Papillary renal cell carcinoma with prominent spindle cell stroma - tumor mimicking mixed epithelial and stromal tumor of the kidney: Clinicopathologic, morphologic, immunohistochemical and molecular genetic analysis of 6 cases". Ann Diagn Pathol 44: 151441. doi:10.1016/j.anndiagpath.2019.151441. PMID 31862520.
- ↑ Al-Obaidy KI, Eble JN, Cheng L, Williamson SR, Sakr WA, Gupta N, Idrees MT, Grignon DJ (August 2019). "Papillary Renal Neoplasm With Reverse Polarity: A Morphologic, Immunohistochemical, and Molecular Study". Am J Surg Pathol 43 (8): 1099–1111. doi:10.1097/PAS.0000000000001288. PMID 31135486.
- ↑ Delahunt, B.; Eble, JN. (Jun 1997). "Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study of 105 tumors.". Mod Pathol 10 (6): 537-44. PMID 9195569.
- ↑ Srigley, JR.; Delahunt, B. (Jun 2009). "Uncommon and recently described renal carcinomas.". Mod Pathol 22 Suppl 2: S2-S23. doi:10.1038/modpathol.2009.70. PMID 19494850.
- ↑ Hes, O.; Brunelli, M.; Michal, M.; Cossu Rocca, P.; Hora, M.; Chilosi, M.; Mina, M.; Boudova, L. et al. (Jun 2006). "Oncocytic papillary renal cell carcinoma: a clinicopathologic, immunohistochemical, ultrastructural, and interphase cytogenetic study of 12 cases.". Ann Diagn Pathol 10 (3): 133-9. doi:10.1016/j.anndiagpath.2005.12.002. PMID 16730306.
- ↑ Han, G.; Yu, W.; Chu, J.; Liu, Y.; Jiang, Y.; Li, Y.; Zhang, W. (Jan 2017). "Oncocytic papillary renal cell carcinoma: A clinicopathological and genetic analysis and indolent clinical course in 14 cases.". Pathol Res Pract 213 (1): 1-6. doi:10.1016/j.prp.2016.04.009. PMID 27931799.
- ↑ http://surgpathcriteria.stanford.edu/kidney/papillary-renal-cell-carcinoma/differential-diagnosis.html. Accessed on: 6 May 2014.
- ↑ Saleeb RM, Brimo F, Farag M, Rompré-Brodeur A, Rotondo F, Beharry V, Wala S, Plant P, Downes MR, Pace K, Evans A, Bjarnason G, Bartlett JMS, Yousef GM (December 2017). "Toward Biological Subtyping of Papillary Renal Cell Carcinoma With Clinical Implications Through Histologic, Immunohistochemical, and Molecular Analysis". Am J Surg Pathol 41 (12): 1618–1629. doi:10.1097/PAS.0000000000000962. PMID 28984673.
- ↑ Ono, Y.; Ito, T.; Tsujino, S.; Aizawa, S.; Suzuki, M. (Jun 1997). "[A study of papillary renal cell carcinoma. Clinicopathological, immunohistochemical features and its typing].". Nihon Hinyokika Gakkai Zasshi 88 (6): 587-95. PMID 9234615.
- ↑ Watanabe, S.; Naganuma, H.; Shimizu, M.; Ota, S.; Murata, S.; Nihei, N.; Matsushima, J.; Mikami, S. et al. (2013). "Adult nephroblastoma with predominant epithelial component: a differential diagnostic candidate of papillary renal cell carcinoma and metanephric adenoma-report of three cases.". Case Rep Pathol 2013: 675875. doi:10.1155/2013/675875. PMID 24083046.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1016. ISBN 0-7216-0187-1.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 292. ISBN 978-0781765275.