Difference between revisions of "Lymph node metastasis"
Jump to navigation
Jump to search
| (37 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
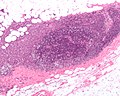
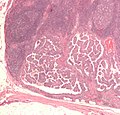
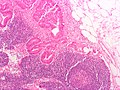
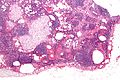
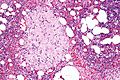
| Caption = Lymph node metastasis (colorectal carcinoma). [[H&E stain]]. | | Caption = Lymph node metastasis (colorectal carcinoma). [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = malignant cells foreign to the lymph node - dependent on specific cancer | | Micro = malignant cells foreign to the lymph node - typically subcapsular sinus; morphology dependent on specific cancer | ||
| Subtypes = micrometastasis, | | Subtypes = dependent on primary tumour - macrometastasis, micrometastasis, isolated tumour cells | ||
| LMDDx = [[endometriosis]], ectopic [[decidua]], [[endosalpingiosis]], melanocytic nevus, [[dermatopathic lymphadenopathy]], [[sinus histiocytosis]], [[tumour deposit]] (dependent on site) | | LMDDx = [[endometriosis]], ectopic [[decidua]], [[endosalpingiosis]], [[nodal nevus|nodal (melanocytic) nevus]], [[dermatopathic lymphadenopathy]], [[sinus histiocytosis]], [[tumour deposit]] (dependent on site), pathology of the lymph node - see ''[[lymph node pathology]]'' and ''[[lymphoma]]'' | ||
| Stains = dependent on tumour | | Stains = dependent on tumour | ||
| IHC = dependent on tumour | | IHC = dependent on tumour | ||
| Line 13: | Line 13: | ||
| Molecular = | | Molecular = | ||
| IF = | | IF = | ||
| Gross = enlarged lymph node, esp. spherical, white mass | | Gross = enlarged lymph node, esp. spherical, white mass with an irregular border +/-extension into surround adipose tissue | ||
| Grossing = | | Grossing = | ||
| Site = [[lymph node]] - see ''[[lymph node pathology]]'' | | Site = [[lymph node]] - see ''[[lymph node pathology]]'' | ||
| Line 19: | Line 19: | ||
| Syndromes = | | Syndromes = | ||
| Clinicalhx = +/-suspicion of cancer | | Clinicalhx = +/-suspicion of cancer | ||
| Signs = +/- | | Signs = +/-large lymph node/mass | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = common - esp. in advanced cancer | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = | ||
| Line 28: | Line 28: | ||
| Other = | | Other = | ||
| ClinDDx = reactive lymphadenopathy, [[lymphoma]], other benign causes of lymphadenopathy - see ''[[lymph node pathology]]'' | | ClinDDx = reactive lymphadenopathy, [[lymphoma]], other benign causes of lymphadenopathy - see ''[[lymph node pathology]]'' | ||
| Tx = dependent on underlying cancer | | Tx = dependent on underlying cancer (type and [[cancer staging|stage]]) | ||
}} | }} | ||
'''Lymph node metastasis''' is [[cancer]] that has spread to a [[lymph node]]. | '''Lymph node metastasis''' is [[cancer]] that has spread to a [[lymph node]]. | ||
| Line 38: | Line 38: | ||
==Gross== | ==Gross== | ||
*Outside: | *Outside/surface of lymph node: | ||
**"Large" - size varies by site. | **"Large" - size varies by site.‡ | ||
***Neck >10 mm.<ref name=pmid18337039>{{Cite journal | last1 = Mack | first1 = MG. | last2 = Rieger | first2 = J. | last3 = Baghi | first3 = M. | last4 = Bisdas | first4 = S. | last5 = Vogl | first5 = TJ. | title = Cervical lymph nodes. | journal = Eur J Radiol | volume = 66 | issue = 3 | pages = 493-500 | month = Jun | year = 2008 | doi = 10.1016/j.ejrad.2008.01.019 | PMID = 18337039 }}</ref> | ***Neck >10 mm.<ref name=pmid18337039>{{Cite journal | last1 = Mack | first1 = MG. | last2 = Rieger | first2 = J. | last3 = Baghi | first3 = M. | last4 = Bisdas | first4 = S. | last5 = Vogl | first5 = TJ. | title = Cervical lymph nodes. | journal = Eur J Radiol | volume = 66 | issue = 3 | pages = 493-500 | month = Jun | year = 2008 | doi = 10.1016/j.ejrad.2008.01.019 | PMID = 18337039 }}</ref> | ||
**Shape - round more suspicious than oval. | **Shape - round more suspicious than oval. | ||
*Sectioned: | *Sectioned lymph node: | ||
**White firm lesion with irregular border - classic appearance. | **White firm lesion with irregular border - classic appearance. | ||
**Non-fatty hilum.<ref name=pmid18337039/> | **Non-fatty hilum.<ref name=pmid18337039/> | ||
Note: | |||
*‡ Small lymph nodes (<3 mm) infrequently affect the stage - at least in [[colorectal adenocarcinoma]].<ref name=pmid24676735>{{Cite journal | last1 = Sloothaak | first1 = DA. | last2 = Grewal | first2 = S. | last3 = Doornewaard | first3 = H. | last4 = van Duijvendijk | first4 = P. | last5 = Tanis | first5 = PJ. | last6 = Bemelman | first6 = WA. | last7 = van der Zaag | first7 = ES. | last8 = Buskens | first8 = CJ. | title = Lymph node size as a predictor of lymphatic staging in colonic cancer. | journal = Br J Surg | volume = 101 | issue = 6 | pages = 701-6 | month = May | year = 2014 | doi = 10.1002/bjs.9451 | PMID = 24676735 }}</ref> | |||
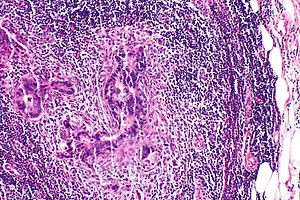
==Microscopic== | ==Microscopic== | ||
| Line 68: | Line 71: | ||
#[[Soft_tissue_lesions#Lymph_node_metastases_in_sarcomas|Lymph node metastases in sarcomas]] are uncommon; they are seen in <3% of cases.<ref name=pmid8424704>{{Cite journal | last1 = Fong | first1 = Y. | last2 = Coit | first2 = DG. | last3 = Woodruff | first3 = JM. | last4 = Brennan | first4 = MF. | title = Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients. | journal = Ann Surg | volume = 217 | issue = 1 | pages = 72-7 | month = Jan | year = 1993 | doi = | PMID = 8424704 | PMC = 1242736}}</ref> | #[[Soft_tissue_lesions#Lymph_node_metastases_in_sarcomas|Lymph node metastases in sarcomas]] are uncommon; they are seen in <3% of cases.<ref name=pmid8424704>{{Cite journal | last1 = Fong | first1 = Y. | last2 = Coit | first2 = DG. | last3 = Woodruff | first3 = JM. | last4 = Brennan | first4 = MF. | title = Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients. | journal = Ann Surg | volume = 217 | issue = 1 | pages = 72-7 | month = Jan | year = 1993 | doi = | PMID = 8424704 | PMC = 1242736}}</ref> | ||
#Fatty lymph nodes (esp. fatty hilus<ref name=pmid18337039>{{Cite journal | last1 = Mack | first1 = MG. | last2 = Rieger | first2 = J. | last3 = Baghi | first3 = M. | last4 = Bisdas | first4 = S. | last5 = Vogl | first5 = TJ. | title = Cervical lymph nodes. | journal = Eur J Radiol | volume = 66 | issue = 3 | pages = 493-500 | month = Jun | year = 2008 | doi = 10.1016/j.ejrad.2008.01.019 | PMID = 18337039 }}</ref>) are less likely to harbor metastases.<ref name=pmid21972135>{{Cite journal | last1 = Korteweg | first1 = MA. | last2 = Veldhuis | first2 = WB. | last3 = Mali | first3 = WP. | last4 = Diepstraten | first4 = SC. | last5 = Luijten | first5 = PR. | last6 = van den Bosch | first6 = MA. | last7 = Eijkemans | first7 = RM. | last8 = van Diest | first8 = PJ. | last9 = Klomp | first9 = DW. | title = Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy. | journal = J Magn Reson Imaging | volume = 35 | issue = 2 | pages = 387-92 | month = Feb | year = 2012 | doi = 10.1002/jmri.22820 | PMID = 21972135 }}</ref> | #Fatty lymph nodes (esp. fatty hilus<ref name=pmid18337039>{{Cite journal | last1 = Mack | first1 = MG. | last2 = Rieger | first2 = J. | last3 = Baghi | first3 = M. | last4 = Bisdas | first4 = S. | last5 = Vogl | first5 = TJ. | title = Cervical lymph nodes. | journal = Eur J Radiol | volume = 66 | issue = 3 | pages = 493-500 | month = Jun | year = 2008 | doi = 10.1016/j.ejrad.2008.01.019 | PMID = 18337039 }}</ref>) are less likely to harbor metastases.<ref name=pmid21972135>{{Cite journal | last1 = Korteweg | first1 = MA. | last2 = Veldhuis | first2 = WB. | last3 = Mali | first3 = WP. | last4 = Diepstraten | first4 = SC. | last5 = Luijten | first5 = PR. | last6 = van den Bosch | first6 = MA. | last7 = Eijkemans | first7 = RM. | last8 = van Diest | first8 = PJ. | last9 = Klomp | first9 = DW. | title = Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy. | journal = J Magn Reson Imaging | volume = 35 | issue = 2 | pages = 387-92 | month = Feb | year = 2012 | doi = 10.1002/jmri.22820 | PMID = 21972135 }}</ref> | ||
# Cancer within adipose tissue may be classified as a ''lymph node metastasis''. | |||
#* In the context of breast cancer: breast cancer in axillary adipose tissue in the absence of normal breast tissue, absence of in situ breast carcinoma and absence of residual lymphoid tissue is classified as a lymph node metastasis/micrometastasis/isolated tumour cells in lymph node.<ref name=cap_breast_inv_ver4p5p0p0>College of American Pathologists. Cancer Protocol Templates - Breast Invasive, Resection. Version 4.5.0.0. Available at: [https://documents.cap.org/protocols/Breast.Invasive_4.5.0.0.REL_CAPCP.docx https://documents.cap.org/protocols/Breast.Invasive_4.5.0.0.REL_CAPCP.docx]. Accessed on: August 8, 2021.</ref> | |||
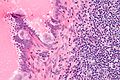
DDx - mimics of metastatic disease: | DDx - mimics of metastatic disease: | ||
| Line 73: | Line 78: | ||
*Ectopic [[decidua]].<ref name=pmid15859655>{{Cite journal | last1 = Wu | first1 = DC. | last2 = Hirschowitz | first2 = S. | last3 = Natarajan | first3 = S. | title = Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall. | journal = Arch Pathol Lab Med | volume = 129 | issue = 5 | pages = e117-20 | month = May | year = 2005 | doi = 10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2 | PMID = 15859655 }}</ref> | *Ectopic [[decidua]].<ref name=pmid15859655>{{Cite journal | last1 = Wu | first1 = DC. | last2 = Hirschowitz | first2 = S. | last3 = Natarajan | first3 = S. | title = Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall. | journal = Arch Pathol Lab Med | volume = 129 | issue = 5 | pages = e117-20 | month = May | year = 2005 | doi = 10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2 | PMID = 15859655 }}</ref> | ||
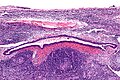
*[[Endosalpingiosis]].<ref name=pmid20631604>{{Cite journal | last1 = Corben | first1 = AD. | last2 = Nehhozina | first2 = T. | last3 = Garg | first3 = K. | last4 = Vallejo | first4 = CE. | last5 = Brogi | first5 = E. | title = Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma. | journal = Am J Surg Pathol | volume = 34 | issue = 8 | pages = 1211-6 | month = Aug | year = 2010 | doi = 10.1097/PAS.0b013e3181e5e03e | PMID = 20631604 }}</ref> | *[[Endosalpingiosis]].<ref name=pmid20631604>{{Cite journal | last1 = Corben | first1 = AD. | last2 = Nehhozina | first2 = T. | last3 = Garg | first3 = K. | last4 = Vallejo | first4 = CE. | last5 = Brogi | first5 = E. | title = Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma. | journal = Am J Surg Pathol | volume = 34 | issue = 8 | pages = 1211-6 | month = Aug | year = 2010 | doi = 10.1097/PAS.0b013e3181e5e03e | PMID = 20631604 }}</ref> | ||
* | *[[Nodal nevus|Nodal (melanocytic) nevus]] - intracapsular or within the trabeculae.<ref name=pmid12717252>{{Cite journal | last1 = Biddle | first1 = DA. | last2 = Evans | first2 = HL. | last3 = Kemp | first3 = BL. | last4 = El-Naggar | first4 = AK. | last5 = Harvell | first5 = JD. | last6 = White | first6 = WL. | last7 = Iskandar | first7 = SS. | last8 = Prieto | first8 = VG. | title = Intraparenchymal nevus cell aggregates in lymph nodes: a possible diagnostic pitfall with malignant melanoma and carcinoma. | journal = Am J Surg Pathol | volume = 27 | issue = 5 | pages = 673-81 | month = May | year = 2003 | doi = | PMID = 12717252 }}</ref> | ||
**Incidence estimated at ~ 0.5% in axillary lymph nodes.<ref name=pmid8037154>{{cite journal |author=Bautista NC, Cohen S, Anders KH |title=Benign melanocytic nevus cells in axillary lymph nodes. A prospective incidence and immunohistochemical study with literature review |journal=Am. J. Clin. Pathol. |volume=102 |issue=1 |pages=102–8 |year=1994 |month=July |pmid=8037154 |doi= |url=}}</ref> | |||
*[[Dermatopathic lymphadenopathy]].{{fact}} | *[[Dermatopathic lymphadenopathy]].{{fact}} | ||
*[[Sinus histiocytosis]] - especially for the junior resident. | *[[Sinus histiocytosis]] - especially for the junior resident. | ||
*[[Tumour deposit]] (discoutinuous extramural extension) - definition dependent on primary tumour | *[[Tumour deposit]] (discoutinuous extramural extension) - definition dependent on primary tumour. | ||
**In the head & neck they are generally considered tumour replaced lymph nodes - though this appears to be evolving.<ref name=pmid25546631>{{Cite journal | last1 = Sarioglu | first1 = S. | last2 = Akbulut | first2 = N. | last3 = Iplikci | first3 = S. | last4 = Aydin | first4 = B. | last5 = Dogan | first5 = E. | last6 = Unlu | first6 = M. | last7 = Ellidokuz | first7 = H. | last8 = Ada | first8 = E. | last9 = Akman | first9 = F. | title = Tumor deposits in head and neck carcinomas. | journal = Head Neck | volume = 38 Suppl 1 | issue = | pages = E256-60 | month = Apr | year = 2016 | doi = 10.1002/hed.23981 | PMID = 25546631 }}</ref> | |||
**In the colon and rectum tumour deposits are considered separately and not counted as lymph nodes. | |||
*Benign thyroid inclusion - somewhat controversial, see ''[[aberrant thyroid tissue]]''.<ref name=pmid15744160 >{{Cite journal | last1 = León | first1 = X. | last2 = Sancho | first2 = FJ. | last3 = García | first3 = J. | last4 = Sañudo | first4 = JR. | last5 = Orús | first5 = C. | last6 = Quer | first6 = M. | title = Incidence and significance of clinically unsuspected thyroid tissue in lymph nodes found during neck dissection in head and neck carcinoma patients. | journal = Laryngoscope | volume = 115 | issue = 3 | pages = 470-4 | month = Mar | year = 2005 | doi = 10.1097/01.mlg.0000157841.63283.87 | PMID = 15744160 }}</ref> | |||
===Images=== | ===Images=== | ||
| Line 93: | Line 102: | ||
Image:Endosalpingiosis_in_lymph_node_-_very_high_mag.jpg | Endosalpingiosis in a LN - very high mag. (WC) | Image:Endosalpingiosis_in_lymph_node_-_very_high_mag.jpg | Endosalpingiosis in a LN - very high mag. (WC) | ||
</gallery> | </gallery> | ||
==Staging== | |||
It is customary to record: | |||
# The size of the largest lymph node metastasis. ‡ | |||
#* It is a dictum of the ''Association of Directors of Anatomic and Surgical pathology''<ref name=pmid11007046>{{Cite journal | title = Recommendations for the reporting of specimens containing oral cavity and oropharynx neoplasms. | journal = Mod Pathol | volume = 13 | issue = 9 | pages = 1038-41 | month = Sep | year = 2000 | doi = 10.1038/modpathol.3880188 | PMID = 11007046 }}</ref> that masses >3 cm are matted lymph nodes/confluent lymph nodes ''or'' a tumour mass. | |||
# The presence/absence of extranodal extension. | |||
#* Tumour grows into the surrounding fat ''or'' extends beyond the contour of the lymph node in association with [[desmoplasia]]. | |||
Note: | |||
*‡ Large size is considered significant at some anatomical [[site]]s, e.g. pharynx. It may change the N stage. | |||
===Number of lymph nodes=== | |||
*The number of lymph nodes is important for [[staging]], as a small number may lead to stage migration (Will Rogers phenomenon);<ref name=pmid24744586>{{Cite journal | last1 = Deng | first1 = JY. | last2 = Liang | first2 = H. | title = Clinical significance of lymph node metastasis in gastric cancer. | journal = World J Gastroenterol | volume = 20 | issue = 14 | pages = 3967-75 | month = Apr | year = 2014 | doi = 10.3748/wjg.v20.i14.3967 | PMID = 24744586 }}</ref> thus, the number of lymph nodes is often used as a [[quality]] measure. | |||
Selected cancers and standard (minimum number of lymph nodes): | |||
*Stomach cancer - 16 lymph nodes.<ref name=pmid24744586/> | |||
*Colorectal cancer - 12 lymph nodes. | |||
*Esophageal cancer - no minimum as per UICC/AJCC staging - based on Li ''et al.''<ref name=pmid23124992>{{Cite journal | last1 = Li | first1 = Q. | last2 = Wu | first2 = SG. | last3 = Gao | first3 = JM. | last4 = Xu | first4 = JJ. | last5 = Hu | first5 = LY. | last6 = Xu | first6 = T. | title = Impact of esophageal cancer staging on overall survival and disease-free survival based on the 2010 AJCC classification by lymph nodes. | journal = J Radiat Res | volume = 54 | issue = 2 | pages = 307-14 | month = Mar | year = 2013 | doi = 10.1093/jrr/rrs096 | PMID = 23124992 }}</ref> - several studies give different numbers (18 lymph nodes Greenstein ''et al.'',<ref name=pmid18224663>{{Cite journal | last1 = Greenstein | first1 = AJ. | last2 = Litle | first2 = VR. | last3 = Swanson | first3 = SJ. | last4 = Divino | first4 = CM. | last5 = Packer | first5 = S. | last6 = Wisnivesky | first6 = JP. | title = Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer. | journal = Cancer | volume = 112 | issue = 6 | pages = 1239-46 | month = Mar | year = 2008 | doi = 10.1002/cncr.23309 | PMID = 18224663 }}</ref> 23 lymph nodes Peyre ''et al.''<ref name=pmid18936567>{{Cite journal | last1 = Peyre | first1 = CG. | last2 = Hagen | first2 = JA. | last3 = DeMeester | first3 = SR. | last4 = Altorki | first4 = NK. | last5 = Ancona | first5 = E. | last6 = Griffin | first6 = SM. | last7 = Hölscher | first7 = A. | last8 = Lerut | first8 = T. | last9 = Law | first9 = S. | title = The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. | journal = Ann Surg | volume = 248 | issue = 4 | pages = 549-56 | month = Oct | year = 2008 | doi = 10.1097/SLA.0b013e318188c474 | PMID = 18936567 }}</ref>). | |||
====Counting lymph nodes==== | |||
The number of lymph nodes is usually based on: | |||
#Number of possible lymph nodes at the time of gross or [[cut-up]]. | |||
#Number of tissue fragments with definite lymph node. | |||
#*Lymph node = lymphoid tissue + capsule. | |||
#Whether tumour nodules without lymphoid tissue are classified as lymph nodes or [[tumour deposits]] - dependent somewhat on the anatomical [[site]]. | |||
Notes: | |||
*Generally, the number of lymph nodes in a block should not exceed the number of possible lymph nodes seen at gross. | |||
==Sign out== | |||
<pre> | |||
Lymph Nodes, Left Axilla, Radical Lymph Node Dissection: | |||
- Three lymph nodes with METASTATIC MALIGNANT MELANOMA | |||
of twenty lymph nodes (3/20). | |||
-- Largest focus of melanoma: 2.1 cm. | |||
-- Extranodal extension: ABSENT. | |||
- Benign skin. | |||
</pre> | |||
===Matted lymph nodes - comment=== | |||
<pre> | |||
Comment: | |||
The size of the largest lymph node metastasis is indeterminate, as the large tumour mass (6.5 cm maximal dimension) consists of matted nodes. Clinical and radiologic correlation is suggested. | |||
</pre> | |||
==See also== | ==See also== | ||
| Line 98: | Line 151: | ||
*[[Cancer]]. | *[[Cancer]]. | ||
*[[Cancer staging]]. | *[[Cancer staging]]. | ||
*[[Lateral aberrant thyroid tissue]]. | |||
*[[Sentinel lymph node]]. | |||
*[[Extranodal extension]]. | |||
*[[Residual cancer burden index]]. | |||
==References== | ==References== | ||
| Line 103: | Line 160: | ||
[[Category:Lymph node pathology]] | [[Category:Lymph node pathology]] | ||
[[Category:Cancer staging]] | |||
Latest revision as of 13:38, 16 October 2024
| Lymph node metastasis | |
|---|---|
| Diagnosis in short | |
 Lymph node metastasis (colorectal carcinoma). H&E stain. | |
|
| |
| LM | malignant cells foreign to the lymph node - typically subcapsular sinus; morphology dependent on specific cancer |
| Subtypes | dependent on primary tumour - macrometastasis, micrometastasis, isolated tumour cells |
| LM DDx | endometriosis, ectopic decidua, endosalpingiosis, nodal (melanocytic) nevus, dermatopathic lymphadenopathy, sinus histiocytosis, tumour deposit (dependent on site), pathology of the lymph node - see lymph node pathology and lymphoma |
| Stains | dependent on tumour |
| IHC | dependent on tumour |
| Gross | enlarged lymph node, esp. spherical, white mass with an irregular border +/-extension into surround adipose tissue |
| Site | lymph node - see lymph node pathology |
|
| |
| Clinical history | +/-suspicion of cancer |
| Signs | +/-large lymph node/mass |
| Prevalence | common - esp. in advanced cancer |
| Prognosis | dependent on specific type of cancer, +/-number of nodes affected |
| Clin. DDx | reactive lymphadenopathy, lymphoma, other benign causes of lymphadenopathy - see lymph node pathology |
| Treatment | dependent on underlying cancer (type and stage) |
Lymph node metastasis is cancer that has spread to a lymph node.
General
- Determination of lymph node status is one of the most common indications for the examination of lymph nodes.
- It is a good idea to look at the tumour (if available) ...before looking at the LNs for mets.
- Lymph node metastasis, in the absence of other metastases, often up-stage a cancer from stage II to stage III.
Gross
- Outside/surface of lymph node:
- "Large" - size varies by site.‡
- Neck >10 mm.[1]
- Shape - round more suspicious than oval.
- "Large" - size varies by site.‡
- Sectioned lymph node:
- White firm lesion with irregular border - classic appearance.
- Non-fatty hilum.[1]
Note:
- ‡ Small lymph nodes (<3 mm) infrequently affect the stage - at least in colorectal adenocarcinoma.[2]
Microscopic
Features:
- Foreign cell population - key feature.
- Classic location: subcapsular sinuses.
- +/-Cells with cytologic features of malignancy.
- Nuclear pleomorphism (variation in size, shape and staining).
- Nuclear atypia:
- Nuclear enlargement.
- Irregular nuclear membrane.
- Irregular chromatin pattern, esp. asymmetry.
- Large or irregular nucleolus.
- Abundant mitotic figures.
- +/-Cells in architectural arrangements seen in malignancy; highly variable - dependent on tumour type and differentiation.
- +/-Gland formation.
- +/-Single cells.
- +/-Small clusters of cells.
Notes:
- Cytologic features of malignancy may not be present; some tumours, e.g. gallbladder carcinoma, do not always have overt cytologic features of malignancy.
- The diagnosis is based on the fact that they are foreign to the lymph node and architecturally consistent with a well-differentiated malignancy.
- Lymph node metastases in sarcomas are uncommon; they are seen in <3% of cases.[3]
- Fatty lymph nodes (esp. fatty hilus[1]) are less likely to harbor metastases.[4]
- Cancer within adipose tissue may be classified as a lymph node metastasis.
- In the context of breast cancer: breast cancer in axillary adipose tissue in the absence of normal breast tissue, absence of in situ breast carcinoma and absence of residual lymphoid tissue is classified as a lymph node metastasis/micrometastasis/isolated tumour cells in lymph node.[5]
DDx - mimics of metastatic disease:
- Endometriosis.
- Ectopic decidua.[6]
- Endosalpingiosis.[7]
- Nodal (melanocytic) nevus - intracapsular or within the trabeculae.[8]
- Incidence estimated at ~ 0.5% in axillary lymph nodes.[9]
- Dermatopathic lymphadenopathy.[citation needed]
- Sinus histiocytosis - especially for the junior resident.
- Tumour deposit (discoutinuous extramural extension) - definition dependent on primary tumour.
- In the head & neck they are generally considered tumour replaced lymph nodes - though this appears to be evolving.[10]
- In the colon and rectum tumour deposits are considered separately and not counted as lymph nodes.
- Benign thyroid inclusion - somewhat controversial, see aberrant thyroid tissue.[11]
Images
Mimics
Staging
It is customary to record:
- The size of the largest lymph node metastasis. ‡
- It is a dictum of the Association of Directors of Anatomic and Surgical pathology[12] that masses >3 cm are matted lymph nodes/confluent lymph nodes or a tumour mass.
- The presence/absence of extranodal extension.
- Tumour grows into the surrounding fat or extends beyond the contour of the lymph node in association with desmoplasia.
Note:
- ‡ Large size is considered significant at some anatomical sites, e.g. pharynx. It may change the N stage.
Number of lymph nodes
- The number of lymph nodes is important for staging, as a small number may lead to stage migration (Will Rogers phenomenon);[13] thus, the number of lymph nodes is often used as a quality measure.
Selected cancers and standard (minimum number of lymph nodes):
- Stomach cancer - 16 lymph nodes.[13]
- Colorectal cancer - 12 lymph nodes.
- Esophageal cancer - no minimum as per UICC/AJCC staging - based on Li et al.[14] - several studies give different numbers (18 lymph nodes Greenstein et al.,[15] 23 lymph nodes Peyre et al.[16]).
Counting lymph nodes
The number of lymph nodes is usually based on:
- Number of possible lymph nodes at the time of gross or cut-up.
- Number of tissue fragments with definite lymph node.
- Lymph node = lymphoid tissue + capsule.
- Whether tumour nodules without lymphoid tissue are classified as lymph nodes or tumour deposits - dependent somewhat on the anatomical site.
Notes:
- Generally, the number of lymph nodes in a block should not exceed the number of possible lymph nodes seen at gross.
Sign out
Lymph Nodes, Left Axilla, Radical Lymph Node Dissection:
- Three lymph nodes with METASTATIC MALIGNANT MELANOMA
of twenty lymph nodes (3/20).
-- Largest focus of melanoma: 2.1 cm.
-- Extranodal extension: ABSENT.
- Benign skin.
Matted lymph nodes - comment
Comment: The size of the largest lymph node metastasis is indeterminate, as the large tumour mass (6.5 cm maximal dimension) consists of matted nodes. Clinical and radiologic correlation is suggested.
See also
- Lymph node pathology.
- Cancer.
- Cancer staging.
- Lateral aberrant thyroid tissue.
- Sentinel lymph node.
- Extranodal extension.
- Residual cancer burden index.
References
- ↑ 1.0 1.1 1.2 Mack, MG.; Rieger, J.; Baghi, M.; Bisdas, S.; Vogl, TJ. (Jun 2008). "Cervical lymph nodes.". Eur J Radiol 66 (3): 493-500. doi:10.1016/j.ejrad.2008.01.019. PMID 18337039.
- ↑ Sloothaak, DA.; Grewal, S.; Doornewaard, H.; van Duijvendijk, P.; Tanis, PJ.; Bemelman, WA.; van der Zaag, ES.; Buskens, CJ. (May 2014). "Lymph node size as a predictor of lymphatic staging in colonic cancer.". Br J Surg 101 (6): 701-6. doi:10.1002/bjs.9451. PMID 24676735.
- ↑ Fong, Y.; Coit, DG.; Woodruff, JM.; Brennan, MF. (Jan 1993). "Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients.". Ann Surg 217 (1): 72-7. PMC 1242736. PMID 8424704. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242736/.
- ↑ Korteweg, MA.; Veldhuis, WB.; Mali, WP.; Diepstraten, SC.; Luijten, PR.; van den Bosch, MA.; Eijkemans, RM.; van Diest, PJ. et al. (Feb 2012). "Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy.". J Magn Reson Imaging 35 (2): 387-92. doi:10.1002/jmri.22820. PMID 21972135.
- ↑ College of American Pathologists. Cancer Protocol Templates - Breast Invasive, Resection. Version 4.5.0.0. Available at: https://documents.cap.org/protocols/Breast.Invasive_4.5.0.0.REL_CAPCP.docx. Accessed on: August 8, 2021.
- ↑ Wu, DC.; Hirschowitz, S.; Natarajan, S. (May 2005). "Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall.". Arch Pathol Lab Med 129 (5): e117-20. doi:10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2. PMID 15859655.
- ↑ Corben, AD.; Nehhozina, T.; Garg, K.; Vallejo, CE.; Brogi, E. (Aug 2010). "Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma.". Am J Surg Pathol 34 (8): 1211-6. doi:10.1097/PAS.0b013e3181e5e03e. PMID 20631604.
- ↑ Biddle, DA.; Evans, HL.; Kemp, BL.; El-Naggar, AK.; Harvell, JD.; White, WL.; Iskandar, SS.; Prieto, VG. (May 2003). "Intraparenchymal nevus cell aggregates in lymph nodes: a possible diagnostic pitfall with malignant melanoma and carcinoma.". Am J Surg Pathol 27 (5): 673-81. PMID 12717252.
- ↑ Bautista NC, Cohen S, Anders KH (July 1994). "Benign melanocytic nevus cells in axillary lymph nodes. A prospective incidence and immunohistochemical study with literature review". Am. J. Clin. Pathol. 102 (1): 102–8. PMID 8037154.
- ↑ Sarioglu, S.; Akbulut, N.; Iplikci, S.; Aydin, B.; Dogan, E.; Unlu, M.; Ellidokuz, H.; Ada, E. et al. (Apr 2016). "Tumor deposits in head and neck carcinomas.". Head Neck 38 Suppl 1: E256-60. doi:10.1002/hed.23981. PMID 25546631.
- ↑ León, X.; Sancho, FJ.; García, J.; Sañudo, JR.; Orús, C.; Quer, M. (Mar 2005). "Incidence and significance of clinically unsuspected thyroid tissue in lymph nodes found during neck dissection in head and neck carcinoma patients.". Laryngoscope 115 (3): 470-4. doi:10.1097/01.mlg.0000157841.63283.87. PMID 15744160.
- ↑ "Recommendations for the reporting of specimens containing oral cavity and oropharynx neoplasms.". Mod Pathol 13 (9): 1038-41. Sep 2000. doi:10.1038/modpathol.3880188. PMID 11007046.
- ↑ 13.0 13.1 Deng, JY.; Liang, H. (Apr 2014). "Clinical significance of lymph node metastasis in gastric cancer.". World J Gastroenterol 20 (14): 3967-75. doi:10.3748/wjg.v20.i14.3967. PMID 24744586.
- ↑ Li, Q.; Wu, SG.; Gao, JM.; Xu, JJ.; Hu, LY.; Xu, T. (Mar 2013). "Impact of esophageal cancer staging on overall survival and disease-free survival based on the 2010 AJCC classification by lymph nodes.". J Radiat Res 54 (2): 307-14. doi:10.1093/jrr/rrs096. PMID 23124992.
- ↑ Greenstein, AJ.; Litle, VR.; Swanson, SJ.; Divino, CM.; Packer, S.; Wisnivesky, JP. (Mar 2008). "Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer.". Cancer 112 (6): 1239-46. doi:10.1002/cncr.23309. PMID 18224663.
- ↑ Peyre, CG.; Hagen, JA.; DeMeester, SR.; Altorki, NK.; Ancona, E.; Griffin, SM.; Hölscher, A.; Lerut, T. et al. (Oct 2008). "The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection.". Ann Surg 248 (4): 549-56. doi:10.1097/SLA.0b013e318188c474. PMID 18936567.