Difference between revisions of "Bacteria"
Jump to navigation
Jump to search
(→Mycobacterium tuberculosis: +DDx) |
m (vauthors) |
||
| (22 intermediate revisions by 2 users not shown) | |||
| Line 14: | Line 14: | ||
==Actinomycetes== | ==Actinomycetes== | ||
===General=== | ===General=== | ||
*IUD needs to be removed if found on a pap test<ref name=Ref_WMSP446>{{Ref WMSP|446}}</ref> - see ''[[Gynecologic cytopathology#Actinomycetes|gynecologic cytopathology]]''. | *[[IUD]] needs to be removed if found on a pap test<ref name=Ref_WMSP446>{{Ref WMSP|446}}</ref> - see ''[[Gynecologic cytopathology#Actinomycetes|gynecologic cytopathology]]''. | ||
*Gram-positive branching rods. | *[[Gram]]-positive branching rods. | ||
*Common in the tonsils. | *Common in the tonsils. | ||
*Part of the large [[Actinobacteria]] group.<ref name=pmid17804669>{{Cite journal | last1 = Ventura | first1 = M. | last2 = Canchaya | first2 = C. | last3 = Tauch | first3 = A. | last4 = Chandra | first4 = G. | last5 = Fitzgerald | first5 = GF. | last6 = Chater | first6 = KF. | last7 = van Sinderen | first7 = D. | title = Genomics of Actinobacteria: tracing the evolutionary history of an ancient phylum. | journal = Microbiol Mol Biol Rev | volume = 71 | issue = 3 | pages = 495-548 | month = Sep | year = 2007 | doi = 10.1128/MMBR.00005-07 | PMID = 17804669 | PMC = 2168647}}</ref> | *Part of the large [[Actinobacteria]] group.<ref name=pmid17804669>{{Cite journal | last1 = Ventura | first1 = M. | last2 = Canchaya | first2 = C. | last3 = Tauch | first3 = A. | last4 = Chandra | first4 = G. | last5 = Fitzgerald | first5 = GF. | last6 = Chater | first6 = KF. | last7 = van Sinderen | first7 = D. | title = Genomics of Actinobacteria: tracing the evolutionary history of an ancient phylum. | journal = Microbiol Mol Biol Rev | volume = 71 | issue = 3 | pages = 495-548 | month = Sep | year = 2007 | doi = 10.1128/MMBR.00005-07 | PMID = 17804669 | PMC = 2168647}}</ref> | ||
| Line 21: | Line 21: | ||
Notes: | Notes: | ||
*''Mycete'' = fungus; these organisms have a fungus-like appearance. | *''Mycete'' = fungus; these organisms have a fungus-like appearance. | ||
** Also called ''pseudomycosis''. | |||
===Gross=== | ===Gross=== | ||
| Line 36: | Line 37: | ||
*Sulfur granule may be seen grossly - yellow.<ref name=medsc>URL: [http://pathmicro.med.sc.edu/mycology/mycology-2.htm http://pathmicro.med.sc.edu/mycology/mycology-2.htm]. Accessed on: 14 September 2011.</ref> | *Sulfur granule may be seen grossly - yellow.<ref name=medsc>URL: [http://pathmicro.med.sc.edu/mycology/mycology-2.htm http://pathmicro.med.sc.edu/mycology/mycology-2.htm]. Accessed on: 14 September 2011.</ref> | ||
Images | ====Images==== | ||
<gallery> | |||
Image:Actinomyces_-_high_mag.jpg | Actinomyces - high mag. (WC) | |||
Image:Actinomyces_-_very_high_mag.jpg | Actinomyces - very high mag. (WC) | |||
File:Actinomycetes_CNS_HE.jpg | Purulent encephalitis with actinomyces in HE. (WC/jensflorian) | |||
File:Actinomycetes_CNS_grocott.jpg | Purulent encephalitis with actinomyces in Grocott. (WC/jensflorian) | |||
</gallery> | |||
*[http://pathology.class.kmu.edu.tw/ch05/Slide42.htm Actinobacteria (kmu.edu.tw)]. | *[http://pathology.class.kmu.edu.tw/ch05/Slide42.htm Actinobacteria (kmu.edu.tw)]. | ||
| Line 47: | Line 52: | ||
*PAS +ve. | *PAS +ve. | ||
**May be confused with a fungus! | **May be confused with a fungus! | ||
*Grocott +ve. | |||
==Helicobacter pylori== | ==Helicobacter pylori== | ||
*Commonly abbreviated ''H. pylori'' or ''HP''. | |||
===General=== | |||
*[[Gram stain|Gram]]-negative rods.<ref name=pmid21290743>{{Cite journal | last1 = Mobley | first1 = HLT. | last2 = Mendz | first2 = GL. | last3 = Hazell | first3 = SL. | last4 = Andersen | first4 = LP. | last5 = Wadström | first5 = T. | title = Basic Bacteriology and Culture | journal = | volume = | issue = | pages = | month = | year = | doi = | PMID = 21290743 | url = http://www.ncbi.nlm.nih.gov/books/NBK2444/}} </ref> | |||
*Causes [[gastritis]] - specifically [[Helicobacter gastritis]]. | |||
*Associated with [[peptic ulcer disease]], [[MALT lymphoma]] and [[gastric carcinoma]]. | |||
===Microscopy=== | |||
:See ''[[Helicobacter gastritis]]''. | :See ''[[Helicobacter gastritis]]''. | ||
==Clostridium difficile== | ==Clostridium difficile== | ||
*Commonly ''C. difficile''. | *Commonly ''C. difficile''. | ||
*Classic cause of [[pseudomembranous colitis]]. | |||
===General=== | ===General=== | ||
| Line 83: | Line 96: | ||
*May mimic a malignancy. | *May mimic a malignancy. | ||
*Strong association with [[HIV]]. | *Strong association with [[HIV]]. | ||
*TB has characteristics of Gram positive and Gram negative bacteria.<ref name=pmid12356459>{{Cite journal | last1 = Fu | first1 = LM. | last2 = Fu-Liu | first2 = CS. | title = Is Mycobacterium tuberculosis a closer relative to Gram-positive or Gram-negative bacterial pathogens? | journal = Tuberculosis (Edinb) | volume = 82 | issue = 2-3 | pages = 85-90 | month = | year = 2002 | doi = | PMID = 12356459 }}</ref> | |||
**Gram stain: subtle positive,<ref name=pmid22476652>{{Cite journal | last1 = Kawakami | first1 = S. | last2 = Kawamura | first2 = Y. | last3 = Nishiyama | first3 = K. | last4 = Hatanaka | first4 = H. | last5 = Fujisaki | first5 = R. | last6 = Ono | first6 = Y. | last7 = Miyazawa | first7 = Y. | last8 = Nishiya | first8 = H. | title = Case of Mycobacterium tuberculosis meningitis: Gram staining as a useful initial diagnostic clue for tuberculous meningitis. | journal = J Infect Chemother | volume = 18 | issue = 6 | pages = 931-6 | month = Dec | year = 2012 | doi = 10.1007/s10156-012-0382-y | PMID = 22476652 }}</ref> often weak positive/little staining.<ref name=pmid21327691>{{Cite journal | last1 = Atsukawa | first1 = Y. | last2 = Kawakami | first2 = S. | last3 = Asahara | first3 = M. | last4 = Ishigaki | first4 = S. | last5 = Tanaka | first5 = T. | last6 = Ono | first6 = Y. | last7 = Nishiya | first7 = H. | last8 = Fujisaki | first8 = R. | last9 = Koga | first9 = I. | title = The usefulness of changing focus during examination using Gram staining as initial diagnostic clue for infective tuberculosis. | journal = J Infect Chemother | volume = 17 | issue = 4 | pages = 571-4 | month = Aug | year = 2011 | doi = 10.1007/s10156-011-0216-3 | PMID = 21327691 }}</ref> | |||
**Genetically closer to Gram negative microorganism than Gram positive organisms - when the whole genome is considered.<ref name=pmid12143965>{{Cite journal | last1 = Fu | first1 = LM. | last2 = Fu-Liu | first2 = CS. | title = Genome comparison of Mycobacterium tuberculosis and other bacteria. | journal = OMICS | volume = 6 | issue = 2 | pages = 199-206 | month = | year = 2002 | doi = 10.1089/153623102760092797 | PMID = 12143965 }}</ref> | |||
====Clinical==== | ====Clinical==== | ||
| Line 100: | Line 116: | ||
Treatment: | Treatment: | ||
*Multiple drugs for a long time (months). | *Multiple drugs for a long time (months). | ||
**Commonly used drugs: isoniazid, rifampin, pyrazinamide, and ethambutol. | **Commonly used drugs: isoniazid, rifampin, pyrazinamide, and ethambutol. | ||
===Gross=== | ===Gross=== | ||
| Line 157: | Line 173: | ||
==Mycobacterium avium complex== | ==Mycobacterium avium complex== | ||
*Abbreviated ''MAC''. | *Abbreviated ''[[MAC]]''. | ||
*Previously referred to as ''Mycobacterium avium-intracellulare'', abbreviated ''MAI''. | *Previously referred to as ''Mycobacterium avium-intracellulare'', abbreviated ''MAI''. | ||
===General=== | ===General=== | ||
| Line 175: | Line 191: | ||
===Stains=== | ===Stains=== | ||
*AFB +ve. | *AFB +ve. | ||
Note: | |||
*[[Fite stain]] considered the preferred stain for MAC.<ref name=pmid21327589>{{cite journal |authors=Ilyas S, Youssef D, Chaudhary H, Al-Abbadi MA |title=Myocbacterium-avium intracellulare associated inflammatory pseudotumor of the anterior nasal cavity |journal=Head Neck Pathol |volume=5 |issue=3 |pages=296–301 |date=September 2011 |pmid=21327589 |pmc=3173547 |doi=10.1007/s12105-011-0248-0 |url=}}</ref> | |||
==Coxiella burnetii== | ==Coxiella burnetii== | ||
| Line 210: | Line 229: | ||
*Similar to pyogenic granuloma - ''see [[pyogenic granuloma]]''. | *Similar to pyogenic granuloma - ''see [[pyogenic granuloma]]''. | ||
Features - ''cat-scratch disease'': | Features - ''[[cat-scratch disease]]'': | ||
*Stellate granulomas. | *Stellate granulomas. | ||
| Line 218: | Line 237: | ||
Image: | Image: | ||
*[http://commons.wikimedia.org/wiki/File:Blood_culture_negative_endocarditis.jpg Bartonella henselae (WC)]. | *[http://commons.wikimedia.org/wiki/File:Blood_culture_negative_endocarditis.jpg Bartonella henselae (WC)]. | ||
==Lactobacillus== | |||
===General=== | |||
*Gram positive bacilli. | |||
*Normal vaginal flora. | |||
===Microscopic=== | |||
Features: | |||
*Slender bacilli. | |||
<gallery> | |||
Image:Lactobacillus_sp_01.png | Lactobacilli. (WC) | |||
</gallery> | |||
==Pseudomonas== | |||
===General=== | |||
*Gram-negative bacteria. | |||
*Common pathogenic ''Pseudomonas aeruginosa''. | |||
*Community-acquired [[bronchopneumonia]]. | |||
**May be seen under nail - causes green nails.<ref name=pmid23064921>{{Cite journal | last1 = Barankin | first1 = B. | last2 = Levy | first2 = J. | title = Dermacase. Can you identify this condition? Pseudomonas aeruginosa infection. | journal = Can Fam Physician | volume = 58 | issue = 10 | pages = 1103-4 | month = Oct | year = 2012 | doi = | PMID = 23064921 }}</ref><ref>{{Cite journal | last1 = Hengge | first1 = UR. | last2 = Bardeli | first2 = V. | title = Images in clinical medicine. Green nails. | journal = N Engl J Med | volume = 360 | issue = 11 | pages = 1125 | month = Mar | year = 2009 | doi = 10.1056/NEJMicm0706497 | PMID = 19279344 }}</ref> | |||
===Gross=== | |||
*Green [[nail]]. | |||
Images: | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3470509/figure/f1-0581103/ Green nail (nih.gov)].<ref name=pmid23064921/> | |||
==Sarcina== | |||
{{Main|Sarcina}} | |||
==See also== | ==See also== | ||
Latest revision as of 17:15, 25 March 2021
Bacteria are single celled microorganisms, without a nucleus (prokaryotes), that can cause lots of morbidity and mortality. They are not infrequently seen by pathologists.
Actinobacteria
General
- A very large group of bacteria.
It includes:[1]
- Actinomycetes.
- Corynebacterium.
- Mycobacterium.
- Nocardia.
- Streptomyces.
Actinomycetes
General
- IUD needs to be removed if found on a pap test[2] - see gynecologic cytopathology.
- Gram-positive branching rods.
- Common in the tonsils.
- Part of the large Actinobacteria group.[1]
Notes:
- Mycete = fungus; these organisms have a fungus-like appearance.
- Also called pseudomycosis.
Gross
- Yellow granules.[3]
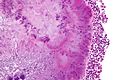
Microscopic
- Branching rods.
- Typically form pink/purple granules ("sulfur granule") that is surrounded by inflammatory cells (lymphocytes or neutrophils).
DDx:
- Nocardia.
Notes:
- Sulfur granule may be seen grossly - yellow.[3]
Images
Stains
- Gram +ve.
- AFB -ve.
- Nocardia +ve.
- PAS +ve.
- May be confused with a fungus!
- Grocott +ve.
Helicobacter pylori
- Commonly abbreviated H. pylori or HP.
General
- Gram-negative rods.[5]
- Causes gastritis - specifically Helicobacter gastritis.
- Associated with peptic ulcer disease, MALT lymphoma and gastric carcinoma.
Microscopy
Clostridium difficile
- Commonly C. difficile.
- Classic cause of pseudomembranous colitis.
General
- Gram positive bacillus.
One virulent strain is:[6][7] BI/NAP1.
- Deletion of tcdC locus.
- Resistant to fluoroquinolones (gatifloxacin and moxifloxacin).
Chlamydia trachomatis
- May be referred to as Chlamydia.
General
- Common.
- May cause lymphogranuloma venereum.
Note:
- Often co-exists with gonorrhea.
Microscopic
- Variable.
Lymphogranuloma venereum:
- See: Cat-scratch disease.
Mycobacterium tuberculosis
- Abbreviated TB.
General
- Causes tuberculosis.
- May mimic a malignancy.
- Strong association with HIV.
- TB has characteristics of Gram positive and Gram negative bacteria.[8]
Clinical
Classic features - pulmonary/systemic:
- Cough.
- Fever.
- Weight loss.
CNS manifestations:
- Tuberculoma (mass).
- Meningitis.
- Abscess.
Tests:
Treatment:
- Multiple drugs for a long time (months).
- Commonly used drugs: isoniazid, rifampin, pyrazinamide, and ethambutol.
Gross
Ghon complex
Consists of two components:[12][13]
- Peripheral focus - subpleural, calcified.
- Central focus - the hilar lymph node that drains the peripheral focus.
Image:
Microscopic
Features:
- Necrotizing granulomas with rod-shaped bacteria.
Note:
- May be non-necrotizing.
DDx:
Images:
- Tuberculosis - case 1 - several images (upmc.edu).
- Tuberculosis - case 2 - several images (upmc.edu).
- Tuberculosis - case 3 - several images (upmc.edu).
Stains
- Ziehl-Neelsen stain - red rod-shaped bacteria - key feature.
- Very small - must use 40x objective.
Image:
Molecular
- Can be diagnosed with PCR.
Mycobacterium leprae
General
- Causes leprosy.
Clinical:
- Nerve damage -> injuries -> disability.
Microscopic
Features:
- Granulomas with rod-shaped bacteria.
Stains
- Fite stain - red rod-shaped bacteria - key feature.
- Very small - must use 40x objective.
Images:
Mycobacterium avium complex
- Abbreviated MAC.
- Previously referred to as Mycobacterium avium-intracellulare, abbreviated MAI.
General
- Refers to an infection with both:[16]
- Mycobacterium avium
- Mycobacterium intracellulare.
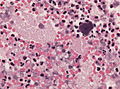
Microscopic
Features:
- Small rod-shaped organisms - within histocytes.
- +/-Granulomas.
DDx:
- Tuberculosis.
- Whipple disease - esp. in the duodenum.
Stains
- AFB +ve.
Note:
- Fite stain considered the preferred stain for MAC.[17]
Coxiella burnetii
General
- Causes: Q fever.
Features:
- Intracellular bacterium.
- Gram negative.
Clinical:
- Flu-like symptoms.
Microscopic
Features:
- Fibrin ring granuloma.
- Epithelioid macrophages (i.e. a granuloma) surrounding a thin pink (fibrin) ring.
DDx:[18]
- Infections (Coxiella burnetii, CMV, EBV + others).
- Drug reaction.
- Malignancy (e.g. Hodgkin lymphoma[19]).
Images:
Bartonella henselae
General
Causative agent in:
Microscopic
Features - bacillary angiomatosis:
- Similar to pyogenic granuloma - see pyogenic granuloma.
Features - cat-scratch disease:
- Stellate granulomas.
Stains
- Warthin-Starry stain +ve.
Image:
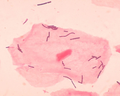
Lactobacillus
General
- Gram positive bacilli.
- Normal vaginal flora.
Microscopic
Features:
- Slender bacilli.
Pseudomonas
General
- Gram-negative bacteria.
- Common pathogenic Pseudomonas aeruginosa.
- Community-acquired bronchopneumonia.
Gross
- Green nail.
Images:
Sarcina
Main article: Sarcina
See also
References
- ↑ 1.0 1.1 Ventura, M.; Canchaya, C.; Tauch, A.; Chandra, G.; Fitzgerald, GF.; Chater, KF.; van Sinderen, D. (Sep 2007). "Genomics of Actinobacteria: tracing the evolutionary history of an ancient phylum.". Microbiol Mol Biol Rev 71 (3): 495-548. doi:10.1128/MMBR.00005-07. PMC 2168647. PMID 17804669. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2168647/.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 446. ISBN 978-0781765275.
- ↑ 3.0 3.1 3.2 URL: http://pathmicro.med.sc.edu/mycology/mycology-2.htm. Accessed on: 14 September 2011.
- ↑ URL: http://pathology.class.kmu.edu.tw/ch05/Slide42.htm . Accessed on: 14 September 2011.
- ↑ Mobley, HLT.; Mendz, GL.; Hazell, SL.; Andersen, LP.; Wadström, T.. Basic Bacteriology and Culture. PMID 21290743. http://www.ncbi.nlm.nih.gov/books/NBK2444/.
- ↑ URL: http://www.medpagetoday.com/InfectiousDisease/PublicHealth/2254. Accessed on: 15 August 2011.
- ↑ McDonald, LC.; Killgore, GE.; Thompson, A.; Owens, RC.; Kazakova, SV.; Sambol, SP.; Johnson, S.; Gerding, DN. (Dec 2005). "An epidemic, toxin gene-variant strain of Clostridium difficile.". N Engl J Med 353 (23): 2433-41. doi:10.1056/NEJMoa051590. PMID 16322603.
- ↑ Fu, LM.; Fu-Liu, CS. (2002). "Is Mycobacterium tuberculosis a closer relative to Gram-positive or Gram-negative bacterial pathogens?". Tuberculosis (Edinb) 82 (2-3): 85-90. PMID 12356459.
- ↑ Kawakami, S.; Kawamura, Y.; Nishiyama, K.; Hatanaka, H.; Fujisaki, R.; Ono, Y.; Miyazawa, Y.; Nishiya, H. (Dec 2012). "Case of Mycobacterium tuberculosis meningitis: Gram staining as a useful initial diagnostic clue for tuberculous meningitis.". J Infect Chemother 18 (6): 931-6. doi:10.1007/s10156-012-0382-y. PMID 22476652.
- ↑ Atsukawa, Y.; Kawakami, S.; Asahara, M.; Ishigaki, S.; Tanaka, T.; Ono, Y.; Nishiya, H.; Fujisaki, R. et al. (Aug 2011). "The usefulness of changing focus during examination using Gram staining as initial diagnostic clue for infective tuberculosis.". J Infect Chemother 17 (4): 571-4. doi:10.1007/s10156-011-0216-3. PMID 21327691.
- ↑ Fu, LM.; Fu-Liu, CS. (2002). "Genome comparison of Mycobacterium tuberculosis and other bacteria.". OMICS 6 (2): 199-206. doi:10.1089/153623102760092797. PMID 12143965.
- ↑ Rose, Alan G. (2008). Atlas of Gross Pathology with Histologic Correlation (1st ed.). Cambridge University Press. pp. 112. ISBN 978-0521868792.
- ↑ URL: http://pathhsw5m54.ucsf.edu/case32/image324.html. Accessed on: 27 February 2012.
- ↑ URL: http://www.medscape.com/viewarticle/576467_2. Accessed on: 2 January 2012.
- ↑ URL: http://www.meddean.luc.edu/lumen/MedEd/orfpath/bfsrinf.htm. Accessed on: 1 April 2012.
- ↑ Turenne, CY.; Wallace, R.; Behr, MA. (Apr 2007). "Mycobacterium avium in the postgenomic era.". Clin Microbiol Rev 20 (2): 205-29. doi:10.1128/CMR.00036-06. PMC 1865596. PMID 17428883. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1865596/.
- ↑ Ilyas S, Youssef D, Chaudhary H, Al-Abbadi MA (September 2011). "Myocbacterium-avium intracellulare associated inflammatory pseudotumor of the anterior nasal cavity". Head Neck Pathol 5 (3): 296–301. doi:10.1007/s12105-011-0248-0. PMC 3173547. PMID 21327589. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3173547/.
- ↑ Tjwa M, De Hertogh G, Neuville B, Roskams T, Nevens F, Van Steenbergen W (2001). "Hepatic fibrin-ring granulomas in granulomatous hepatitis: report of four cases and review of the literature". Acta Clin Belg 56 (6): 341–8. PMID 11881318.
- ↑ de Bayser L, Roblot P, Ramassamy A, Silvain C, Levillain P, Becq-Giraudon B (July 1993). "Hepatic fibrin-ring granulomas in giant cell arteritis". Gastroenterology 105 (1): 272–3. PMID 8514044.
- ↑ 20.0 20.1 Barankin, B.; Levy, J. (Oct 2012). "Dermacase. Can you identify this condition? Pseudomonas aeruginosa infection.". Can Fam Physician 58 (10): 1103-4. PMID 23064921.
- ↑ Hengge, UR.; Bardeli, V. (Mar 2009). "Images in clinical medicine. Green nails.". N Engl J Med 360 (11): 1125. doi:10.1056/NEJMicm0706497. PMID 19279344.