Difference between revisions of "Gestational trophoblastic disease"
Jump to navigation
Jump to search
m (→Entities - intermediate trophoblast: fix ddx) |
m |
||
| (52 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'''Gestational trophoblastic disease''' (GTD) includes [[choriocarcinoma]] and hydatidiform moles. | '''Gestational trophoblastic disease''' (abbreviated '''GTD'''), also '''gestational trophoblastic neoplasia''' (abbreviated '''GTN'''), includes [[choriocarcinoma]] and hydatidiform moles. | ||
=Overview= | =Overview= | ||
===Most common=== | ===Most common=== | ||
Overview of gestational trophoblastic disease: | Overview of gestational trophoblastic disease: | ||
{| class="wikitable" | {| class="wikitable sortable" | ||
! Type of mole | |||
! Gross | |||
! [[Nuclear atypia]] | |||
! [[Chorionic villi]] | |||
! [[IHC]] | |||
! DNA content | |||
! Micrographs | |||
|- | |- | ||
| Complete mole | | Complete mole | ||
| "snowstorm" | | "snowstorm" | ||
| +/- ? | | +/- ? | ||
| yes, all abnormal | | yes, all abnormal | ||
| p57(KIP2) -ve | | p57(KIP2) -ve | ||
| Paternal, diploid | | Paternal, diploid | ||
| Line 35: | Line 35: | ||
| beta-hCG +ve | | beta-hCG +ve | ||
| ? | | ? | ||
| [ | | [[Image:Choriocarcinoma_-2-_very_high_mag.jpg|thumb|center|120px|Choriocarcinoma. (WC)]] | ||
|- | |- | ||
|} | |} | ||
| Line 56: | Line 56: | ||
==Choriocarcinoma== | ==Choriocarcinoma== | ||
{{Main|Choriocarcinoma}} | {{Main|Choriocarcinoma}} | ||
==Hydatidiform moles== | ==Hydatidiform moles== | ||
| Line 115: | Line 75: | ||
===Microscopic=== | ===Microscopic=== | ||
Hydropic changes: | Hydropic changes: | ||
{| class="wikitable" | {| class="wikitable sortable" | ||
! Entity | |||
! [[Chorionic villi]] (outline) | |||
! Cisterns | |||
! [[Blood vessel]]s | |||
! Nucleated RBCs | |||
! p57 / Ki-67<ref>URL: [http://www.ihcworld.com/_newsletter/2003/focus_mar_2003.pdf http://www.ihcworld.com/_newsletter/2003/focus_mar_2003.pdf]. Accessed on: 28 May 2011.</ref> staining ‡ | |||
! Ploidy | |||
! Micrograph | |||
|- | |- | ||
| Complete mole | | Complete mole | ||
| Line 152: | Line 112: | ||
| [http://www.ipath-network.com/ipath/object/view/181344] | | [http://www.ipath-network.com/ipath/object/view/181344] | ||
|} | |} | ||
Note: | |||
* ‡ The amount of [[Ki-67]] staining varies considerably based on what one reads. Chen ''at al.''<ref>{{Cite journal | last1 = Chen | first1 = Y. | last2 = Shen | first2 = D. | last3 = Gu | first3 = Y. | last4 = Zhong | first4 = P. | last5 = Xie | first5 = J. | last6 = Song | first6 = Q. | title = The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion. | journal = Wien Klin Wochenschr | volume = 124 | issue = 5-6 | pages = 184-7 | month = Mar | year = 2012 | doi = 10.1007/s00508-011-0119-4 | PMID = 22218717 }}</ref> suggest 25% versus 5% for partial mole versus hydropic abortus. | |||
====Mole | ====Mole versus normal==== | ||
*Moles have large [[chorionic villi]] with edema and abnormal blood vessels.<ref>URL: [http://pathologyoutlines.com/placenta.html#hydatgeneral http://pathologyoutlines.com/placenta.html#hydatgeneral].</ref> | *Moles have large [[chorionic villi]] with edema and abnormal blood vessels.<ref>URL: [http://pathologyoutlines.com/placenta.html#hydatgeneral http://pathologyoutlines.com/placenta.html#hydatgeneral].</ref> | ||
====Non-molar | ====Non-molar versus partial versus complete - short version==== | ||
Features:<ref>{{Cite journal | last1 = Howat | first1 = AJ. | last2 = Beck | first2 = S. | last3 = Fox | first3 = H. | last4 = Harris | first4 = SC. | last5 = Hill | first5 = AS. | last6 = Nicholson | first6 = CM. | last7 = Williams | first7 = RA. | title = Can histopathologists reliably diagnose molar pregnancy? | journal = J Clin Pathol | volume = 46 | issue = 7 | pages = 599-602 | month = Jul | year = 1993 | doi = | PMID = 8157742 }}</ref> | Features:<ref name=pmid8157742>{{Cite journal | last1 = Howat | first1 = AJ. | last2 = Beck | first2 = S. | last3 = Fox | first3 = H. | last4 = Harris | first4 = SC. | last5 = Hill | first5 = AS. | last6 = Nicholson | first6 = CM. | last7 = Williams | first7 = RA. | title = Can histopathologists reliably diagnose molar pregnancy? | journal = J Clin Pathol | volume = 46 | issue = 7 | pages = 599-602 | month = Jul | year = 1993 | doi = | PMID = 8157742 | url = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC501384/?page=3 }}</ref> | ||
*Non-molar pregnancy: polar proliferation of trophoblastic tissue. | *Non-molar pregnancy: polar proliferation of trophoblastic tissue. | ||
*Partial mole: Norwegian fjord periphery, circumferential or multifocal trophoblastic proliferation, fetal parts. | *Partial mole: Norwegian fjord periphery, circumferential or multifocal trophoblastic proliferation, fetal parts. | ||
| Line 164: | Line 126: | ||
===IHC=== | ===IHC=== | ||
*p57(KIP2) - the gene is strongly paternally imprinted and the paternal copy is inactived; its expression is from the maternal gene. | *p57(KIP2) - the gene is strongly paternally imprinted and the paternal copy is inactived; its expression is from the maternal gene. | ||
**Complete moles | **Complete moles lack the maternal genome; thus, p57(KIP2) immunostaining (in the cytotrophoblasts and villous stromal cells) is absent.<ref name=pmid15754295>{{cite journal |author=Merchant SH, Amin MB, Viswanatha DS, Malhotra RK, Moehlenkamp C, Joste NE |title=p57KIP2 immunohistochemistry in early molar pregnancies: emphasis on its complementary role in the differential diagnosis of hydropic abortuses |journal=Hum. Pathol. |volume=36 |issue=2 |pages=180–6 |year=2005 |month=February |pmid=15754295 |doi=10.1016/j.humpath.2004.12.007 |url=}}</ref><ref name=pmid12514787>{{Cite journal | last1 = Fukunaga | first1 = M. | title = Immunohistochemical characterization of p57(KIP2) expression in early hydatidiform moles. | journal = Hum Pathol | volume = 33 | issue = 12 | pages = 1188-92 | month = Dec | year = 2002 | doi = 10.1053/hupa.2002.129421 | PMID = 12514787 }}</ref> | ||
***Intermediate trophoblasts and maternal tissue are positive controls.<ref name=pmid12514787/> | |||
**Memory device: | **Memory device: | ||
***'''''p'''57 is '''p'''ositive in '''p'''artial moles''. | ***'''''p'''57 is '''p'''ositive in '''p'''artial moles''. | ||
| Line 171: | Line 134: | ||
===Molecular=== | ===Molecular=== | ||
*The type of mole can be determined by [[cytogenetics]].<ref>[http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf]</ref> | *The type of mole can be determined by [[cytogenetics]].<ref>[http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf]</ref> | ||
==Hydropic abortus== | |||
===General=== | |||
*May be seen in the context of a previously detected fetal heart beat. | |||
===Microsopic=== | |||
Features: | |||
*Enlarged chorionic villi with some cisterns. | |||
DDx:<ref>{{cite journal |authors=Rios-Doria E, Pennington KP, Reiter DJ, Parker EU |title=Diagnostic challenges in differentiating between hydropic abortus, and complete and partial hydatidiform molar pregnancies in early gestation |journal=Int J Gynecol Cancer |volume=33 |issue=9 |pages=1482–1484 |date=September 2023 |pmid=37268312 |doi=10.1136/ijgc-2022-004104 |url=}}</ref> | |||
*Molar pregnancy. | |||
===Sign out=== | |||
<pre> | |||
Submitted as "Retained Products of Conception": | |||
- Small and large chorionic villi with cisterns, suggestive of hydropic abortus, see comment. | |||
- Benign decidual tissue present. | |||
- Negative for evidence of fetal tissue in sampled tissue, see comment. | |||
Comment: | |||
Imaging previously described a gestational sac and a fetal heart beat. | |||
</pre> | |||
==Partial hydatidiform mole== | ==Partial hydatidiform mole== | ||
| Line 186: | Line 171: | ||
***Contain fluid in the centre, i.e. are "hydropic". | ***Contain fluid in the centre, i.e. are "hydropic". | ||
**Villi with cytotrophoblastic inclusions. | **Villi with cytotrophoblastic inclusions. | ||
***Cytotrophoblast in the core of a villus (normally it is only at the surface of the villus). | ***[[Cytotrophoblast]] in the core of a villus (normally it is only at the surface of the villus). | ||
*May have fetal parts, such as nucleated RBCs. | *May have fetal parts, such as nucleated RBCs. | ||
*Trophoblastic proliferation. | *Trophoblastic proliferation. | ||
| Line 192: | Line 177: | ||
*"Norwegian fjord periphery"<ref name=pmid8157742>{{Cite journal | last1 = Howat | first1 = AJ. | last2 = Beck | first2 = S. | last3 = Fox | first3 = H. | last4 = Harris | first4 = SC. | last5 = Hill | first5 = AS. | last6 = Nicholson | first6 = CM. | last7 = Williams | first7 = RA. | title = Can histopathologists reliably diagnose molar pregnancy? | journal = J Clin Pathol | volume = 46 | issue = 7 | pages = 599-602 | month = Jul | year = 1993 | doi = | PMID = 8157742 | url = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC501384/?page=3 }}</ref> - jagged border / irregular sawtooth-like periphery. | *"Norwegian fjord periphery"<ref name=pmid8157742>{{Cite journal | last1 = Howat | first1 = AJ. | last2 = Beck | first2 = S. | last3 = Fox | first3 = H. | last4 = Harris | first4 = SC. | last5 = Hill | first5 = AS. | last6 = Nicholson | first6 = CM. | last7 = Williams | first7 = RA. | title = Can histopathologists reliably diagnose molar pregnancy? | journal = J Clin Pathol | volume = 46 | issue = 7 | pages = 599-602 | month = Jul | year = 1993 | doi = | PMID = 8157742 | url = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC501384/?page=3 }}</ref> - jagged border / irregular sawtooth-like periphery. | ||
**Complete moles tend to have a smooth border | **Complete moles tend to have a smooth border | ||
DDx: | |||
*[[Complete hydatidiform mole]]. | |||
*[[Placental mesenchymal dysplasia]]. | |||
*Hydropic abortus - see [[products of conception]] and [[chorionic villi]]. | |||
Images: | Images: | ||
*[http://www-medlib.med.utah.edu/WebPath/PLACHTML/PLAC067.html Partial mole (med.utah.edu)]. | *[http://www-medlib.med.utah.edu/WebPath/PLACHTML/PLAC067.html Partial mole (med.utah.edu)]. | ||
*[http://www.gfmer.ch/selected_images_v2/detail_list.php?cat1=12&cat2=86&cat3=795&cat4=3&stype=n Partial mole - several images (gfmer.ch)]. | *[http://www.gfmer.ch/selected_images_v2/detail_list.php?cat1=12&cat2=86&cat3=795&cat4=3&stype=n Partial mole - several images (gfmer.ch)]. | ||
===IHC=== | |||
Features:<ref name=pmid22218717>{{Cite journal | last1 = Chen | first1 = Y. | last2 = Shen | first2 = D. | last3 = Gu | first3 = Y. | last4 = Zhong | first4 = P. | last5 = Xie | first5 = J. | last6 = Song | first6 = Q. | title = The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion. | journal = Wien Klin Wochenschr | volume = 124 | issue = 5-6 | pages = 184-7 | month = Mar | year = 2012 | doi = 10.1007/s00508-011-0119-4 | PMID = 22218717 }}</ref> | |||
*Ki-67 ~ 25+/-5% of cytotrophoblasts and intermediate trophoblasts. | |||
**Hydropic abortus ~ 5+/-1%. | |||
*p53 ~ 22+/-12% of cytotrophoblasts and intermediate trophoblasts. | |||
**Hydropic abortus ~ 5+/-3%. | |||
==Complete hydatidiform mole== | ==Complete hydatidiform mole== | ||
| Line 208: | Line 205: | ||
*Male derived, i.e. arise from DNA in sperm; empty egg fertilized. | *Male derived, i.e. arise from DNA in sperm; empty egg fertilized. | ||
===Radiology=== | ===Gross/Radiology=== | ||
*"Snowstorm" appearance on ultrasound.<ref>URL:[http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589 http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589]. Accessed on: 27 July 2010.</ref> | *"Snowstorm" appearance on ultrasound.<ref>URL:[http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589 http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589]. Accessed on: 27 July 2010.</ref> | ||
*May be described as "grape-like" on gross exam.<ref name=pmid18162339>{{Cite journal | last1 = Abike | first1 = F. | last2 = Temizkan | first2 = O. | last3 = Payasli | first3 = A. | last4 = Avsar | first4 = F. | last5 = Karahan | first5 = N. | last6 = Baspinar | first6 = S. | title = Postmenopausal complete hydatidiform mole: a case report. | journal = Maturitas | volume = 59 | issue = 1 | pages = 95-8 | month = Jan | year = 2008 | doi = 10.1016/j.maturitas.2007.10.005 | PMID = 18162339 }}</ref> | |||
Image: | |||
*[http://library.med.utah.edu/WebPath/PLACHTML/PLAC063.html Complete mole (utah.edu)]. | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 217: | Line 218: | ||
**Very rarely nucleated [[RBC]]s. | **Very rarely nucleated [[RBC]]s. | ||
Images | ====Images==== | ||
<gallery> | |||
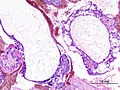
Image:Intermediate_trophoblast_3_-_low_mag.jpg | Complete mole and intermediate trophoblast - intermed. mag. (WC) | |||
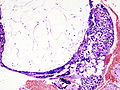
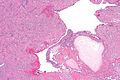
Image:Hydatidiform_mole_%281%29_complete_type.jpg | Complete mole - low mag. (WC) | |||
Image:Hydatidiform_mole_%282%29_complete_type.jpg | Complete mole - high mag. (WC) | |||
</gallery> | |||
==Invasive hydatidiform mole== | ==Invasive hydatidiform mole== | ||
*[[AKA]] ''invasive mole''. | |||
*[[AKA]] ''chorioadenoma destruens''.<ref name=pmid6300738>{{Cite journal | last1 = McDonald | first1 = TW. | last2 = Ruffolo | first2 = EH. | title = Modern management of gestational trophoblastic disease. | journal = Obstet Gynecol Surv | volume = 38 | issue = 2 | pages = 67-83 | month = Feb | year = 1983 | doi = | PMID = 6300738 }}</ref> | |||
===General=== | ===General=== | ||
*This is not a distinct subtype - see ''[[hydatidiform mole]]''. | *This is not a distinct subtype - see ''[[hydatidiform mole]]''. | ||
| Line 232: | Line 237: | ||
DDx: | DDx: | ||
*[[Choriocarcinoma]]. | *[[Choriocarcinoma]] - lack [[chorionic villi]], usu. hemorrhagic. | ||
====Images==== | |||
<gallery> | |||
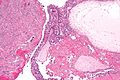
Image:Invasive hydatidiform mole - very low mag.jpg | Invasive mole - very low mag. (WC) | |||
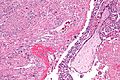
Image:Invasive_hydatidiform_mole_-_low_mag.jpg | Invasive mole - low mag. (WC) | |||
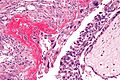
Image:Invasive_hydatidiform_mole_-_intermed_mag.jpg | Invasive mole - intermed. mag. (WC) | |||
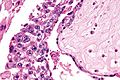
Image:Invasive_hydatidiform_mole_-_high_mag.jpg | Invasive mole - high mag. (WC) | |||
Image:Invasive hydatidiform mole - very high mag.jpg | Invasive mole - very high mag. (WC) | |||
</gallery> | |||
=Entities - intermediate trophoblast= | =Entities - intermediate trophoblast= | ||
| Line 247: | Line 261: | ||
| paucicellular, hyaline material | | paucicellular, hyaline material | ||
| no mitotic activity | | no mitotic activity | ||
| | | p16 -ve, MIB1 low | ||
| [[EPS]] | | [[EPS]], [[squamous carcinoma]] | ||
| post-partum | | post-partum | ||
| [http://www.ijpmonline.org/viewimage.asp?img=IndianJPatholMicrobiol_2009_52_2_240_48931_u4.jpg (ijpmonline.org)] | | [[Image:Placental_site_nodule_-_intermed_mag.jpg |thumb| center| 80px|PSN. (WC)]] [http://www.ijpmonline.org/viewimage.asp?img=IndianJPatholMicrobiol_2009_52_2_240_48931_u4.jpg (ijpmonline.org)] | ||
|- | |- | ||
| [[Exaggerated placental site]] (EPS) | | [[Exaggerated placental site]] (EPS) | ||
| Line 277: | Line 291: | ||
|- | |- | ||
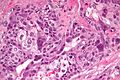
| [[Choriocarcinoma]] | | [[Choriocarcinoma]] | ||
| polygonal cells with clear cytoplasm ( | | polygonal cells with clear cytoplasm ([[cytotrophoblast]]s) | ||
| multinucleated cells with smudged nuclei ( | | multinucleated cells with smudged nuclei ([[syncytiotrophoblast]]s), '''no''' [[chorionic villi]] | ||
| beta-hCG +ve, p63 +ve | | beta-hCG +ve, p63 +ve | ||
| [[invasive hydatidiform mole]], [[PSTT]] | | [[invasive hydatidiform mole]], [[PSTT]] | ||
| elevated beta-hCG (serum); '''not''' intermediate trophoblast derived. | | elevated beta-hCG (serum); '''not''' intermediate trophoblast derived. | ||
| [http://www.webpathology.com/image.asp?case=36&n=1 (webpathology.com)] | | [[Image:Choriocarcinoma_-2-_very_high_mag.jpg|thumb|center|120px|Choriocarcinoma. (WC)]] [http://www.webpathology.com/image.asp?case=36&n=1 (webpathology.com)] | ||
|- <!-- | |- <!-- | ||
| Entity? | | Entity? | ||
| Line 295: | Line 309: | ||
==Placental site nodule== | ==Placental site nodule== | ||
*Abbreviated ''PSN''. | *Abbreviated ''PSN''. | ||
{{Main|Placental site nodule}} | |||
==Exaggerated placental site== | ==Exaggerated placental site== | ||
*Abbreviated ''EPS''. | *Abbreviated ''EPS''. | ||
*Previously known as ''syncytial endometritis''.<ref>URL: [http://www.webpathology.com/image.asp?case=565&n=7 http://www.webpathology.com/image.asp?case=565&n=7]. Accessed on: 22 May 2014.</ref> | |||
{{Main|Exaggerated placental site}} | |||
* | |||
==Placental site trophoblastic tumour== | ==Placental site trophoblastic tumour== | ||
| Line 386: | Line 348: | ||
DDx: | DDx: | ||
*[[Exaggerated placental site]] | *[[Exaggerated placental site]] - EPS has near zero Ki-67. | ||
*[[Choriocarcinoma]] - choriocarcinoma biphasic.<ref>URL: [http://www.webpathology.com/image.asp?n=3&Case=588 http://www.webpathology.com/image.asp?n=3&Case=588]. Accessed on: 1 January 2012.</ref> | |||
*[[Choriocarcinoma]] | |||
Images: | Images: | ||
*[http://www.webpathology.com/case.asp?case=588 Collection of PSTT images (webpathology.com)]. | *[http://www.webpathology.com/case.asp?case=588 Collection of PSTT images (webpathology.com)]. | ||
===IHC=== | |||
Features:<ref>{{Cite journal | last1 = Shih | first1 = IM. | last2 = Kurman | first2 = RJ. | title = Ki-67 labeling index in the differential diagnosis of exaggerated placental site, placental site trophoblastic tumor, and choriocarcinoma: a double immunohistochemical staining technique using Ki-67 and Mel-CAM antibodies. | journal = Hum Pathol | volume = 29 | issue = 1 | pages = 27-33 | month = Jan | year = 1998 | doi = | PMID = 9445130 }}</ref> | |||
*CD146 +ve. | |||
*p63 -ve. | |||
*Ki-67 ~14+/-7%. | |||
**Choriocarcinoma ~69+/-20%. | |||
==Epithelioid trophoblastic tumour== | ==Epithelioid trophoblastic tumour== | ||
| Line 403: | Line 370: | ||
*Vaginal bleeding. | *Vaginal bleeding. | ||
*Elevated beta-hCG. | *Elevated beta-hCG. | ||
===Gross=== | |||
Features:<ref name=pmid16258513>{{Cite journal | last1 = Fadare | first1 = O. | last2 = Parkash | first2 = V. | last3 = Carcangiu | first3 = ML. | last4 = Hui | first4 = P. | title = Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement. | journal = Mod Pathol | volume = 19 | issue = 1 | pages = 75-82 | month = Jan | year = 2006 | doi = 10.1038/modpathol.3800485 | PMID = 16258513 }}</ref> | |||
*Solid mass. | |||
*Flesh-like appearance. | |||
Image: | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 414: | Line 388: | ||
Images: | Images: | ||
*[http://www.webpathology.com/image.asp?case=589&n=2 ETT (webpathology.com)].<ref name=webp_ett/> | *[http://www.webpathology.com/image.asp?case=589&n=2 ETT (webpathology.com)].<ref name=webp_ett/> | ||
===IHC=== | ===IHC=== | ||
| Line 440: | Line 413: | ||
[[Category:Gynecologic pathology]] | [[Category:Gynecologic pathology]] | ||
[[Category:Gestational trophoblastic disease]] | |||
Latest revision as of 22:07, 7 December 2023
Gestational trophoblastic disease (abbreviated GTD), also gestational trophoblastic neoplasia (abbreviated GTN), includes choriocarcinoma and hydatidiform moles.
Overview
Most common
Overview of gestational trophoblastic disease:
| Type of mole | Gross | Nuclear atypia | Chorionic villi | IHC | DNA content | Micrographs |
|---|---|---|---|---|---|---|
| Complete mole | "snowstorm" | +/- ? | yes, all abnormal | p57(KIP2) -ve | Paternal, diploid | complete mole + intermed. trophoblast (WC), complete mole (WC) |
| Partial mole | grape-like clusters |
+/- | large villi, villi with cisterns, villi with cytotrophoblastic inclusions |
p57(KIP2) +ve | Maternal & paternal, tripoid | partial mole (utah.edu) |
| Choriocarcinoma | haemorrahagic, necrotic | marked | none | beta-hCG +ve | ? |
More comprehensive overview
Benign abnormal looking placenta:
- Placental site nodule (PSN).
- Exaggerated placental site (EPS).
Abnormal fertilization:
Tumours:
- Invasive mole.
- Choriocarcinoma.
- Placental site trophoblastic tumour (PSTT).
- Epithelioid trophoblastic tumour (ETT).
Entities
Choriocarcinoma
Main article: Choriocarcinoma
Hydatidiform moles
General
- Significance: increased risk for choriocarcinoma (in complete moles).
- Non-neoplastic proliferation.
Etymology:
- Hydatid is literally watery vesicle.[1]
Types
- Partial mole - see partial mole.
- Complete mole - see complete mole.
Extent:
- Invasive mole - not a subtype.
- Within uterine muscle +/- vessels.
Microscopic
Hydropic changes:
| Entity | Chorionic villi (outline) | Cisterns | Blood vessels | Nucleated RBCs | p57 / Ki-67[2] staining ‡ | Ploidy | Micrograph |
|---|---|---|---|---|---|---|---|
| Complete mole | bizarre; often not ovoid; fissures/slit-like gaps | well-developed | canalicular (thin walled) / few (???) | rare | -ve / ~70% | diploid / tetraploid | [1], [2], [3], [4] |
| Partial mole | jagged, still quasi ovoid | poorly developed / small | present | common | +ve / ~70% | triploid | [5], [6] |
| Hydropic abortus | smooth | poorly developed / small | common | common | +ve / ~20% | diploid | [7] |
Note:
- ‡ The amount of Ki-67 staining varies considerably based on what one reads. Chen at al.[3] suggest 25% versus 5% for partial mole versus hydropic abortus.
Mole versus normal
- Moles have large chorionic villi with edema and abnormal blood vessels.[4]
Non-molar versus partial versus complete - short version
Features:[5]
- Non-molar pregnancy: polar proliferation of trophoblastic tissue.
- Partial mole: Norwegian fjord periphery, circumferential or multifocal trophoblastic proliferation, fetal parts.
- Complete mole: grapes grossly, large villi with round borders.
IHC
- p57(KIP2) - the gene is strongly paternally imprinted and the paternal copy is inactived; its expression is from the maternal gene.
Molecular
- The type of mole can be determined by cytogenetics.[8]
Hydropic abortus
General
- May be seen in the context of a previously detected fetal heart beat.
Microsopic
Features:
- Enlarged chorionic villi with some cisterns.
DDx:[9]
- Molar pregnancy.
Sign out
Submitted as "Retained Products of Conception": - Small and large chorionic villi with cisterns, suggestive of hydropic abortus, see comment. - Benign decidual tissue present. - Negative for evidence of fetal tissue in sampled tissue, see comment. Comment: Imaging previously described a gestational sac and a fetal heart beat.
Partial hydatidiform mole
- AKA partial mole.
General
Genetics:
- Usually triploid (e.g. 69XXY).
Microscopic
Features:
- Abnormal chorionic villi.
- Villi too large (>0.1 mm ?).
- Villi with cisterns.
- Contain fluid in the centre, i.e. are "hydropic".
- Villi with cytotrophoblastic inclusions.
- Cytotrophoblast in the core of a villus (normally it is only at the surface of the villus).
- May have fetal parts, such as nucleated RBCs.
- Trophoblastic proliferation.
- Without atypia.[10]
- "Norwegian fjord periphery"[5] - jagged border / irregular sawtooth-like periphery.
- Complete moles tend to have a smooth border
DDx:
- Complete hydatidiform mole.
- Placental mesenchymal dysplasia.
- Hydropic abortus - see products of conception and chorionic villi.
Images:
IHC
Features:[11]
- Ki-67 ~ 25+/-5% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-1%.
- p53 ~ 22+/-12% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-3%.
Complete hydatidiform mole
General
Epidemiology:
- May precede choriocarcinoma[12] ~ 1-2% risk.
Genetics:
- Diploid - most are 46XX.
- Male derived, i.e. arise from DNA in sperm; empty egg fertilized.
Gross/Radiology
Image:
Microscopic
Features:
- No normal villi.
- No fetal parts seen.
- Very rarely nucleated RBCs.
Images
Invasive hydatidiform mole
General
- This is not a distinct subtype - see hydatidiform mole.
Microscopic
Features:
- Chorionic villi - abnormal +/- normal.
- Trophoblastic cells within uterine muscle +/- vessels - key feature.
DDx:
- Choriocarcinoma - lack chorionic villi, usu. hemorrhagic.
Images
Entities - intermediate trophoblast
| Entity | Key feature | Other histologic features | IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|
| Placental site nodule (PSN) | paucicellular, hyaline material | no mitotic activity | p16 -ve, MIB1 low | EPS, squamous carcinoma | post-partum | (ijpmonline.org) |
| Exaggerated placental site (EPS) | abundant intermediate trophoblasts - between muscle | no mitotic activity | MIB1 ~0% | PSTT, PSN | post-partum | Image? |
| Placental site trophoblastic tumour (PSTT) | abundant cytoplasm - not clear, dyscohesive | +/-multinucleation | MIB1 high, p63 -ve, CD146 +ve | EPS, choriocarcinoma | Other? | (webpathology.com) |
| Epithelioid trophoblastic tumour (ETT) | nests of cells in hyaline stroma | eosinophilic cytoplasm, central nucleus | MIB1 low, p63 +ve, CD146 -ve | squamous carcinoma | Other? | (webpathology.com) |
| Choriocarcinoma | polygonal cells with clear cytoplasm (cytotrophoblasts) | multinucleated cells with smudged nuclei (syncytiotrophoblasts), no chorionic villi | beta-hCG +ve, p63 +ve | invasive hydatidiform mole, PSTT | elevated beta-hCG (serum); not intermediate trophoblast derived. | (webpathology.com) |
Placental site nodule
- Abbreviated PSN.
Main article: Placental site nodule
Exaggerated placental site
- Abbreviated EPS.
- Previously known as syncytial endometritis.[16]
Main article: Exaggerated placental site
Placental site trophoblastic tumour
- Abbreviated PSTT.
- Malignant counterpart of exaggerated placental site (abbreviated EPS).
General
- Derived from intermediate trophoblast.
- Follows pregnancy.
- May be associated with nephrotic syndrome[17] with granular IgM staining.[18]
Clinical:
- Raised (serum) beta-hCG - but usually not has high as in choriocarcinoma.
- Prognosis dependent on time of diagnosis from last pregnancy.
- <48 months = good prognosis.[19]
Microscopic
Features:
- Large cells:
- Nuclear pleomorphism.
- Cytoplasm:
- Abundant.
- Solid, i.e. not vesicular.
- Light basophilic, not clear - key feature.
- NC ratio ~ normal.
- +/-Multinucleated cells.
- Ectatic blood vessels.
Note:
- No chorionic villi.
- If villi are present... it is probably a hydatidiform mole.
DDx:
- Exaggerated placental site - EPS has near zero Ki-67.
- Choriocarcinoma - choriocarcinoma biphasic.[21]
Images:
IHC
Features:[22]
- CD146 +ve.
- p63 -ve.
- Ki-67 ~14+/-7%.
- Choriocarcinoma ~69+/-20%.
Epithelioid trophoblastic tumour
- Abbreviated ETT.
General
- Often in endocervix.
- Malignant counterpart of placental site nodule or PSN.
Clinical:
- Vaginal bleeding.
- Elevated beta-hCG.
Gross
Features:[23]
- Solid mass.
- Flesh-like appearance.
Image:
Microscopic
Features:[24]
- Architecture: nests in hyaline matrix.
- Cytoplasm: abundant, eosinophilic.
DDx:
- Invasive squamous cell carcinoma.
Images:
IHC
Features:[25]
- Cyclin E +ve (nuclear).
- p16 -ve.
- +ve (nuclear) in squamous cell carcinoma of the cervix.
Others:
- HMCK -ve.
- SCC +ve.
Note:
- p63 not useful... +ve in both SCC and ETT.
See also
- Hydatid disease - due to Echinoccus spp. such as E. granulosus.
- Chorionic villi.
- Ectopic pregnancy.
- Placenta.
- Arias-Stella reaction - benign atypical changes of the endometrium associated with trophoblastic tissue.
References
- ↑ URL: http://dictionary.reference.com/browse/hydatid.
- ↑ URL: http://www.ihcworld.com/_newsletter/2003/focus_mar_2003.pdf. Accessed on: 28 May 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ URL: http://pathologyoutlines.com/placenta.html#hydatgeneral.
- ↑ 5.0 5.1 Howat, AJ.; Beck, S.; Fox, H.; Harris, SC.; Hill, AS.; Nicholson, CM.; Williams, RA. (Jul 1993). "Can histopathologists reliably diagnose molar pregnancy?". J Clin Pathol 46 (7): 599-602. PMID 8157742. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC501384/?page=3.
- ↑ Merchant SH, Amin MB, Viswanatha DS, Malhotra RK, Moehlenkamp C, Joste NE (February 2005). "p57KIP2 immunohistochemistry in early molar pregnancies: emphasis on its complementary role in the differential diagnosis of hydropic abortuses". Hum. Pathol. 36 (2): 180–6. doi:10.1016/j.humpath.2004.12.007. PMID 15754295.
- ↑ 7.0 7.1 Fukunaga, M. (Dec 2002). "Immunohistochemical characterization of p57(KIP2) expression in early hydatidiform moles.". Hum Pathol 33 (12): 1188-92. doi:10.1053/hupa.2002.129421. PMID 12514787.
- ↑ http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf
- ↑ Rios-Doria E, Pennington KP, Reiter DJ, Parker EU (September 2023). "Diagnostic challenges in differentiating between hydropic abortus, and complete and partial hydatidiform molar pregnancies in early gestation". Int J Gynecol Cancer 33 (9): 1482–1484. doi:10.1136/ijgc-2022-004104. PMID 37268312.
- ↑ URL: http://pathologyoutlines.com/placenta.html#incompletemole. Accessed on: 9 August 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1111. ISBN 0-7216-0187-1.
- ↑ URL:http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589. Accessed on: 27 July 2010.
- ↑ Abike, F.; Temizkan, O.; Payasli, A.; Avsar, F.; Karahan, N.; Baspinar, S. (Jan 2008). "Postmenopausal complete hydatidiform mole: a case report.". Maturitas 59 (1): 95-8. doi:10.1016/j.maturitas.2007.10.005. PMID 18162339.
- ↑ McDonald, TW.; Ruffolo, EH. (Feb 1983). "Modern management of gestational trophoblastic disease.". Obstet Gynecol Surv 38 (2): 67-83. PMID 6300738.
- ↑ URL: http://www.webpathology.com/image.asp?case=565&n=7. Accessed on: 22 May 2014.
- ↑ Bonazzi, C.; Urso, M.; Dell'Anna, T.; Sacco, S.; Buda, A.; Cantú, MG. (Aug 2004). "Placental site trophoblastic tumor: an overview.". J Reprod Med 49 (8): 585-8. PMID 15457847.
- ↑ Komatsuda, A.; Nakamoto, Y.; Asakura, K.; Yasuda, T.; Imai, H.; Miura, AB. (May 1992). "Case report: nephrotic syndrome associated with a total hydatidiform mole.". Am J Med Sci 303 (5): 309-12. PMID 1580319.
- ↑ 19.0 19.1 Schmid, P.; Nagai, Y.; Agarwal, R.; Hancock, B.; Savage, PM.; Sebire, NJ.; Lindsay, I.; Wells, M. et al. (Jul 2009). "Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study.". Lancet 374 (9683): 48-55. doi:10.1016/S0140-6736(09)60618-8. PMID 19552948.
- ↑ Baergen, RN.; Rutgers, JL.; Young, RH.; Osann, K.; Scully, RE. (Mar 2006). "Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance.". Gynecol Oncol 100 (3): 511-20. doi:10.1016/j.ygyno.2005.08.058. PMID 16246400.
- ↑ URL: http://www.webpathology.com/image.asp?n=3&Case=588. Accessed on: 1 January 2012.
- ↑ Shih, IM.; Kurman, RJ. (Jan 1998). "Ki-67 labeling index in the differential diagnosis of exaggerated placental site, placental site trophoblastic tumor, and choriocarcinoma: a double immunohistochemical staining technique using Ki-67 and Mel-CAM antibodies.". Hum Pathol 29 (1): 27-33. PMID 9445130.
- ↑ Fadare, O.; Parkash, V.; Carcangiu, ML.; Hui, P. (Jan 2006). "Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement.". Mod Pathol 19 (1): 75-82. doi:10.1038/modpathol.3800485. PMID 16258513.
- ↑ 24.0 24.1 URL: http://www.webpathology.com/image.asp?case=589&n=2. Accessed on: 15 August 2011.
- ↑ Mao, TL.; Seidman, JD.; Kurman, RJ.; Shih, IeM. (Sep 2006). "Cyclin E and p16 immunoreactivity in epithelioid trophoblastic tumor--an aid in differential diagnosis.". Am J Surg Pathol 30 (9): 1105-10. doi:10.1097/01.pas.0000209854.28282.87. PMID 16931955.