Difference between revisions of "Metastases"
| (32 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
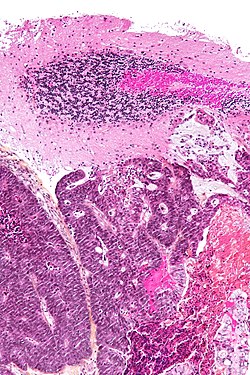
'''Metastases''' are usually an ominous finding. | [[Image:Metastatic adenocarcinoma - cerebellum - intermed mag.jpg|right|250px|thumb|A [[brain metastasis]]. [[H&E stain]].]] | ||
'''Metastases''' are tumours that have spread from elsewhere and are separate from the initial (primary) lesion; usually, they are an ominous finding. | |||
Metastases are not always obvious when encountered; thus, ''metastasis'' should be considered with every diagnosis of a [[cancer|malignant tumour]]. | |||
Seen from pathology, ''metastatic disease'' and ''direct extension of a tumour'' (on a biopsy) may be indistinguishable. Collectively, they may also be referred to as '''secondary tumours'''. | |||
'''''[[Cancers of unknown primary]]''''' are dealt with in the ''[[cancer]]'' article. A general approach to undifferentiated tumours is given in the ''[[basics]]'' article under the heading '''''[[modified general morphologic DDx of malignancy]]'''''. | '''''[[Cancers of unknown primary]]''''' are dealt with in the ''[[cancer]]'' article. A general approach to undifferentiated tumours is given in the ''[[basics]]'' article under the heading '''''[[modified general morphologic DDx of malignancy]]'''''. | ||
[[Lymph node]] metastases are dealt with in the article ''[[lymph node metastases]]''. | |||
A handful of things have metastatic-like behaviour but are not malignant. Examples of benign things with metastatic-like behaviour are: benign metastasizing leiomyoma,<ref name=pmid15099894>{{Cite journal | last1 = Pitts | first1 = S. | last2 = Oberstein | first2 = EM. | last3 = Glassberg | first3 = MK. | title = Benign metastasizing leiomyoma and lymphangioleiomyomatosis: sex-specific diseases? | journal = Clin Chest Med | volume = 25 | issue = 2 | pages = 343-60 | month = Jun | year = 2004 | doi = 10.1016/j.ccm.2004.01.014 | PMID = 15099894 }}</ref> [[endometriosis]], [[endosalpingiosis]] and [[Nodal nevus|benign nevus cells (in lymph nodes)]].<ref>{{Cite journal | last1 = Cook | first1 = MG. | title = Benign melanocytic lesions mimicking melanomas. | journal = Pathology | volume = 36 | issue = 5 | pages = 414-8 | month = Oct | year = 2004 | doi = 10.1080/00313020412331283842 | PMID = 15370110 }}</ref> | |||
=Special types= | =Special types= | ||
==In-transit metastasis== | ==In-transit metastasis== | ||
{{Main|In-transit metastasis}} | |||
{{Main|Tumour deposits}} | |||
*It is called "in-transit", as it happens while the tumour is on the way to the regional lymph node. | |||
*If a separate tumour nodule is close to the primary tumour, it is known as ''[[satellitosis]]''. | |||
Note: | |||
* | *The definitions vary based on the primary site. | ||
*'' | **The general definition (see the ''[[in-transit metastasis]]'' article) applies to [[dermatopathology]]. | ||
**In the [[colon]] and [[rectum]], they are generally known as ''[[tumour deposits]]'', ''discoutinuous extramural extension'' and ''peritumoral deposits''.<ref name=pmid19136930>{{Cite journal | last1 = Puppa | first1 = G. | last2 = Ueno | first2 = H. | last3 = Kayahara | first3 = M. | last4 = Capelli | first4 = P. | last5 = Canzonieri | first5 = V. | last6 = Colombari | first6 = R. | last7 = Maisonneuve | first7 = P. | last8 = Pelosi | first8 = G. | title = Tumor deposits are encountered in advanced colorectal cancer and other adenocarcinomas: an expanded classification with implications for colorectal cancer staging system including a unifying concept of in-transit metastases. | journal = Mod Pathol | volume = 22 | issue = 3 | pages = 410-5 | month = Mar | year = 2009 | doi = 10.1038/modpathol.2008.198 | PMID = 19136930 }}</ref> | |||
=Specific sites= | =Specific sites= | ||
===Internal organs=== | ===Internal organs=== | ||
{{Main|Liver metastasis}} | |||
{{Main|Lung metastasis}} | |||
{{Main|Kidney metastasis}} | |||
===Lymph node=== | ===Lymph node=== | ||
| Line 23: | Line 34: | ||
===Other=== | ===Other=== | ||
{{Main|Peritoneal metastasis}} | |||
{{Main|Testicular metastasis}} | |||
{{Main|Ovarian metastasis}} | |||
{{Main|Urinary bladder metastasis}} | |||
===Brain=== | ===Brain=== | ||
| Line 35: | Line 49: | ||
{{Main|Osteosarcoma}} | {{Main|Osteosarcoma}} | ||
*[[Giant cells]]. | *[[Giant cells]]. | ||
=IHC= | |||
*Dependent on (suspected) primary. | |||
Not necessary to do stains/[[immunostain]]s if all of the following are true: | |||
#A primary is already established by pathology. | |||
#The morphology of the lesion is compatible with the established primary. | |||
#The clinical impression is a metastasis. | |||
#The suspected primary is ''not'' [[breast cancer|breast]]. | |||
#*ASCO/CAP guidelines state that ''ER and PR (in breast cancer recurrences) should always be re-tested''.<ref name=pmid20586616>{{Cite journal | last1 = Hammond | first1 = ME. | last2 = Hayes | first2 = DF. | last3 = Dowsett | first3 = M. | last4 = Allred | first4 = DC. | last5 = Hagerty | first5 = KL. | last6 = Badve | first6 = S. | last7 = Fitzgibbons | first7 = PL. | last8 = Francis | first8 = G. | last9 = Goldstein | first9 = NS. | title = American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). | journal = Arch Pathol Lab Med | volume = 134 | issue = 7 | pages = e48-72 | month = Jul | year = 2010 | doi = 10.1043/1543-2165-134.7.e48 | PMID = 20586616 }}</ref> | |||
=Sign out= | =Sign out= | ||
| Line 68: | Line 92: | ||
The tumour cells stain as follows: | The tumour cells stain as follows: | ||
POSITIVE: CK7, ER, PR, | POSITIVE: CK7, ER, PR, MAMMAGLOBIN. | ||
NEGATIVE: CK20, TTF-1, CDX2, HER2, GCDFP. | NEGATIVE: CK20, TTF-1, CDX2, HER2, GCDFP. | ||
| Line 81: | Line 105: | ||
====Micro==== | ====Micro==== | ||
=====Probable lung metastasis===== | =====Probable lung metastasis===== | ||
The sections show atypical cohesive cuboidal-to-low columnar | The sections show atypical cohesive cuboidal-to-low columnar cells with moderate nuclear pleomorphism. The nuclei are round/ovoid and eccentrically placed in the cell. Nucleoli of moderate size are identified. Mitotic figures are present. The cytoplasm is lightly eosinophilic and vacuoles are seen focally. | ||
=See also= | =See also= | ||
*[[Cancer]]. | *[[Cancer]]. | ||
*[[Basics]]. | *[[Basics]]. | ||
*[[Pulmonary lymphangitic carcinomatosis]]. | |||
*[[Lytic metastases]]. | |||
=Reference= | =Reference= | ||
| Line 91: | Line 117: | ||
[[Category:Basics]] | [[Category:Basics]] | ||
[[Category:Cancer staging]] | |||
Latest revision as of 18:56, 3 January 2023
Metastases are tumours that have spread from elsewhere and are separate from the initial (primary) lesion; usually, they are an ominous finding.
Metastases are not always obvious when encountered; thus, metastasis should be considered with every diagnosis of a malignant tumour.
Seen from pathology, metastatic disease and direct extension of a tumour (on a biopsy) may be indistinguishable. Collectively, they may also be referred to as secondary tumours.
Cancers of unknown primary are dealt with in the cancer article. A general approach to undifferentiated tumours is given in the basics article under the heading modified general morphologic DDx of malignancy.
Lymph node metastases are dealt with in the article lymph node metastases.
A handful of things have metastatic-like behaviour but are not malignant. Examples of benign things with metastatic-like behaviour are: benign metastasizing leiomyoma,[1] endometriosis, endosalpingiosis and benign nevus cells (in lymph nodes).[2]
Special types
In-transit metastasis
- It is called "in-transit", as it happens while the tumour is on the way to the regional lymph node.
- If a separate tumour nodule is close to the primary tumour, it is known as satellitosis.
Note:
- The definitions vary based on the primary site.
- The general definition (see the in-transit metastasis article) applies to dermatopathology.
- In the colon and rectum, they are generally known as tumour deposits, discoutinuous extramural extension and peritumoral deposits.[3]
Specific sites
Internal organs
Lymph node
Other
Brain
Specific tumours
Melanoma
Osteosarcoma
IHC
- Dependent on (suspected) primary.
Not necessary to do stains/immunostains if all of the following are true:
- A primary is already established by pathology.
- The morphology of the lesion is compatible with the established primary.
- The clinical impression is a metastasis.
- The suspected primary is not breast.
- ASCO/CAP guidelines state that ER and PR (in breast cancer recurrences) should always be re-tested.[4]
Sign out
This depends somewhat on the tumour. A synoptic is not done. Margin status should be commented on. A morphologic description is useful if a subsequent resection is done.
Bowel
SMALL BOWEL, RESECTION: - METASTATIC ADENOCARCINOMA, SEE COMMENT. - SURGICAL MARGINS NEGATIVE FOR MALIGNANCY. COMMENT: The tumour involves only the outer aspect of the bowel wall; the bowel mucosa is not involved. The tumour consists of glands with cuboidal tumour cells that have a moderate quantity of pale cytoplasm, and round nuclei. The tumour is moderately differentiated.
Spine
Pending
VERTEBRAL LESION, L1, BIOPSY: - ADENOCARCINOMA -- PENDING IHC.
LESION OF T7 VERTEBRA, CORE BIOPSY: - METASTATIC CARCINOMA, CONSISTENT WITH BREAST PRIMARY, SEE COMMENT. COMMENT: The morphology is compatible with a metastatic breast carcinoma. The tumour cells stain as follows: POSITIVE: CK7, ER, PR, MAMMAGLOBIN. NEGATIVE: CK20, TTF-1, CDX2, HER2, GCDFP. The immunostaining profile is compatible with a metastatic breast carcinoma. ER, PR and HER2 are interpreted as Class I IHC tests (results used by pathologists), as per the CAP classification.[1] 1. Am J Clin Pathol 133 (3):354-65.
Micro
Probable lung metastasis
The sections show atypical cohesive cuboidal-to-low columnar cells with moderate nuclear pleomorphism. The nuclei are round/ovoid and eccentrically placed in the cell. Nucleoli of moderate size are identified. Mitotic figures are present. The cytoplasm is lightly eosinophilic and vacuoles are seen focally.
See also
Reference
- ↑ Pitts, S.; Oberstein, EM.; Glassberg, MK. (Jun 2004). "Benign metastasizing leiomyoma and lymphangioleiomyomatosis: sex-specific diseases?". Clin Chest Med 25 (2): 343-60. doi:10.1016/j.ccm.2004.01.014. PMID 15099894.
- ↑ Cook, MG. (Oct 2004). "Benign melanocytic lesions mimicking melanomas.". Pathology 36 (5): 414-8. doi:10.1080/00313020412331283842. PMID 15370110.
- ↑ Puppa, G.; Ueno, H.; Kayahara, M.; Capelli, P.; Canzonieri, V.; Colombari, R.; Maisonneuve, P.; Pelosi, G. (Mar 2009). "Tumor deposits are encountered in advanced colorectal cancer and other adenocarcinomas: an expanded classification with implications for colorectal cancer staging system including a unifying concept of in-transit metastases.". Mod Pathol 22 (3): 410-5. doi:10.1038/modpathol.2008.198. PMID 19136930.
- ↑ Hammond, ME.; Hayes, DF.; Dowsett, M.; Allred, DC.; Hagerty, KL.; Badve, S.; Fitzgibbons, PL.; Francis, G. et al. (Jul 2010). "American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version).". Arch Pathol Lab Med 134 (7): e48-72. doi:10.1043/1543-2165-134.7.e48. PMID 20586616.