Difference between revisions of "Salivary glands"
| Line 258: | Line 258: | ||
Image:Chronic_sialadenitis.jpg | Chronic sialadenitis. (WC/Nephron) | Image:Chronic_sialadenitis.jpg | Chronic sialadenitis. (WC/Nephron) | ||
</gallery> | </gallery> | ||
===Sign out=== | |||
<pre> | |||
SUBMANDIULAR GLAND, RIGHT, EXCISION: | |||
- CHRONIC SIALOLITHIASIS. | |||
</pre> | |||
====Micro==== | |||
The sections show salivary gland with a moderate patchy mononuclear cell infiltrate, fibrosis and a large calcification. No zonal necrosis is identified. Significant nuclear atypia is not identified. | |||
==Salivary gland mucocele== | ==Salivary gland mucocele== | ||
Revision as of 16:35, 20 December 2013
The salivary glands help digest food. ENT surgeons take 'em out and want you to diagnose 'em. Cytopathology of the salivary glands is covered in the Head and neck cytopathology article.
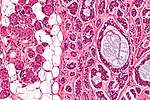
Normal salivary glands
Types of salivary glands
Types of glands:[1]
- Serrous - eosinophilic cytoplasmic granules, acinar arrangement - vaguely resembles the acinar morphology of the pancreas.
- Mucinous - light eosinophilic staining.
Identifying the glands
The three main glands:
- Parotid:
- Serous glands - lower viscosity, acini (lobules).[2]
- Most tumours in this gland are benign.
- Submandibular:
- Serous and mucinous glands.
- Serous ~90% of gland.
- Mucinous ~10% of gland.
- Serous demilunes = mucinous gland with "cap" consisting of a serous glandular component.
- Demilune = crescent.[3]
- Image: Serous demilunes (duke.edu).[4]
- Serous and mucinous glands.
- Sublingual:
- Mucinous glands.
Other:
- Adipose tissue is found between the glands.
- It increases with age.
Images:
Memory devices:
- The parotid gland vaguely resembles the pancreas.
- Submandibular = glands are mixed.
Overview
Benign tumours
Tabular form - adapted from Thompson[5]
| Entity | Architecture | Morphology | Cell borders | Cytoplasm | Nucleus | DDx | Other | Image |
|---|---|---|---|---|---|---|---|---|
| Pleomorphic adenoma | var. | mixed pop.; must include: (1) myoepithelium, (2) mesenchymal stroma, and (3) epithelium (ductal cells) or chondromyxoid stroma | var. | var. | (1) plasmacytoid | adenoid cystic carcinoma | occ. encapsulated, mixed pop. of glandular, myoepithelial and mesenchymal cells |
|
| Warthin tumour | papillary, bilayer |
cuboid (basal), columnar (apical) | clearly seen | eosinophilic, abundant | unremarkable | sebaceous lymphadenoma | AKA papillary cystadenoma lymphomatosum | |
| Basal cell adenoma | var., islands surrounded by hyaline bands, lesion encapsulated |
basaloid | subtle | scant, hyperchromatic |
granular | basal cell adenocarcinoma | - | - |
| Canalicular adenoma | chains of cells | cuboid or columnar | subtle | scant, hyperchromatic |
granular | basal cell adenoma | exclusively oral cavity, 80% in upper lip; IHC: p63- | (webpathology.com), (webpathology.com) |
| Sialoblastoma | var., islands surrounded by loose fibrous stroma |
basaloid | subtle | scant, hyperch. | granular | basal cell adenocarcinoma | - | - |
Malignant tumours
Tabular form - adapted from Thompson[6]
| Entity | Architecture | Morphology | Cell borders | Cytoplasm | Nucleus | DDx | Other | Image |
|---|---|---|---|---|---|---|---|---|
| Mucoepidermoid carcinoma | cystic & solid | epithelioid | distinct | fuffy, clear, abundant |
nuclei sm. | SCC (?) | IHC: p63+ | |
| Adenoid cystic carcinoma (AdCC) | pseudocysts, cribriform, solid, hyaline stroma |
epithelioid | subtle | scant, hyperchromatic |
small +/-"carrot-shaped" |
pleomorphic adenoma, PLGA | Stains: PAS+ (pseudocyst material), CD117+, cyclin D1+ | |
| Acinic cell carcinoma (AcCC) | sheets, acinar (islands) | epithelioid | clear | granular abundant | stippled, +/-occ. nucleoli | adenocarcinoma not otherwise specified, oncocytoma of salivary gland | Stains: PAS +ve, PAS-D +ve; IHC: S-100 -ve, p63 -ve | |
| Salivary duct carcinoma | glandular, cribriform | columnar | subtle/clear | hyperchromatic | columnar | metastatic breast carcinoma | similar to ductal breast carcinoma; male>female |
|
| Polymorphous low-grade adenocarcinoma | variable, often small nests, may be targetoid |
epithelioid | indistinct | eosinophilic | ovoid & small with small nucleoli |
AdCC | minor salivary gland tumour, often in palate, cytologically monotonous; IHC: S100+, CK+, vim.+, GFAP+/-, BCL2+/- |
|
| Epithelial-myoepithelial carcinoma | nests (myoepithelial) with tubules (epithelial) | epithelioid | not distinct | eosinophilic cytoplasm; epithelial: scant; myoepithelial: moderate | focal clearing | AdCC, pleomorphic adenoma | rare | |
| Basal cell adenocarcinoma | var., islands surrounded by hyaline bands, lesion not encapsulated |
basaloid | subtle | scant, hyperchromatic |
granular | basal cell adenoma | rare, usu. parotid gland, may arise from a basal cell adenoma |
DDx
Palate
Benign parotid tumours
Oncocytic tumours
- Benign:
- Oncocytoma.
- Warthin tumour.
- Malignant:
- Mucoepidermoid carcinoma, oncocytic variant.
- Salivary duct carcinoma.
- Carcinoma ex pleomorphic carcinoma with a salivary duct carcinoma component.
- Apocrine carcinoma.
- Oncocytic carcinoma.
- Acinic cell carcinoma, oncocytic variant.
Clear cell tumours
- Mucoepidermoid carcinoma, clear cell variant.
- Acinic cell carcinoma, clear cell variant.
- Hyalinizing clear cell carcinoma.
- Epithelial-myoepithelial carcinoma.
- Metastatic clear cell carcinoma.
- Metastatic clear cell renal cell carcinoma.
IHC overview
General:
- Usually has limited value.
Specifics:
- Luminal markers: CK7, CK19, CAM5.2 (LMWK).
- Basal markers: p63, HMWK, CK14.
- Myoepithelial markers: calponin, actin.
- Uncommitted: S-100.
Notes:
- p63 and S-100 are sometimes call myoepithelial.
Benign
General DDx:
- Inflammation.
- Neoplasm.
- Ductal obstrution.
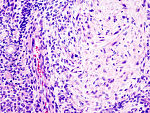
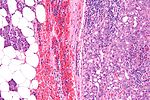
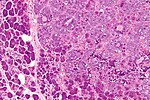
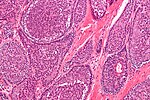
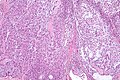
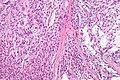
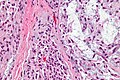
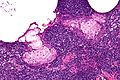
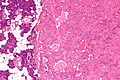
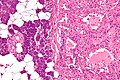
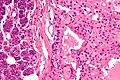
Chronic sialadenitis
- Chronic sailolithiasis redirect here.
General
Etiology:[7]
- Infection.
- Autoimmune (e.g. Sjögren syndrome, systemic lupus erythematosus).
- Other.
Microscopic
Features:
- Non-neoplastic mononuclear inflammatory infiltrate (lymphocytes, plasma cells).
- Fibrosis.
- +/-Calcifications.
Note:
- If the infiltrate is predominantly lymphocytes Sjögren's is a possibility, and reporting a Focus score should be considered.
DDx:
- Lymphoma - especially MALT lymphoma.[8]
Image
Sign out
SUBMANDIULAR GLAND, RIGHT, EXCISION: - CHRONIC SIALOLITHIASIS.
Micro
The sections show salivary gland with a moderate patchy mononuclear cell infiltrate, fibrosis and a large calcification. No zonal necrosis is identified. Significant nuclear atypia is not identified.
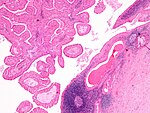
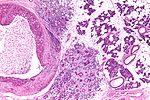
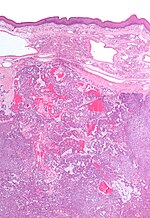
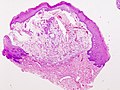
Salivary gland mucocele
General
- Benign.
- Infected mucocele = mucopyocele.
Microscopic
Features:[9]
- Granulation tissue-like and pseudocyst-like.
- Granulation tissue-like:
- Fibroblasts.
- Small caliber blood vessels.
- Histocytes.
- Neutrophils.
- Pseudocyst:
- No epithelial lining.
- Poorly circumscribed.
- Granulation tissue-like:
- Pale pink extracellular material (mucous) - key feature.
- +/-Granulomas.[10]
DDx:
- Granulation tissue.
- Signet ring cell carcinoma - muciphages may mimic signet ring cells.
Images
www:
Sign out
LESION, LEFT LOWER LIP, EXCISION: - BENIGN MUCOCELE.
Micro
The sections show a stratified squamous epithelium with a thin layer of parakeratosis, minor salivary glands, and a well-circumscribed cystic lesion.
The cystic lesion has a mildly fibrotic appearing wall, is lined by histiocytes intermixed with rare lymphocytes, and contains mucous and macrophages. No significant nuclear atypia is identified. Mitotic activity is not readily apparent.
Pleomorphic adenoma
Myoepithelioma
General
- Usually benign.
- May be malignant.
Location - head and neck:[11]
- Parotid gland ~50%.
- Palate ~25%
- Submandibular gland ~12%.
Notes:
Microsopic
Features:[14]
- Myoepithelial cells - may be:
- Spindled.
- Plasmacytoid.
- Epithelioid.
- Clear (rare).
- Lack tubules, i.e. epithelial component.
- May be up to 10% (or 5%[15]).
DDx:
Images
IHC
Features:[14]
- S100 +ve.
- GFAP +ve.
- CK14 +ve.
Others:[16]
- SMA +ve.
- Calponin +ve.
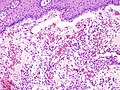
Basal cell adenoma
General
- ~2% of salivary gland tumours.
- May be multifocal.
- Usually parotid gland, occasionally submandibular gland.
- Female:male = ~2:1.
- May be seen in association with dermal cylindromas in the context of a genetic mutation.[17]
- Malignant transformation - rarely.
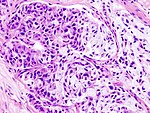
Microscopic
Features:
- Basal component.
- Basophilic cells - key feature.
- Usu. in nests.
- May be bilayered tubules or trabeculae.
- Large basophilic nucleus.
- Minimal-to-moderate eosinophilic cytoplasm.
- Stromal cells.
- Plump spindle cells without significant nuclear atypia - distinguishing feature.
- Stromal cell nuclei width ~= diameter RBC.
- Dense hyaline stroma.
- Plump spindle cells without significant nuclear atypia - distinguishing feature.
- Tubular component.
- Within basal component, may be minimal.
- Lesion is encapsulated - key feature.
Notes:
- No chondromyxoid stroma.
- Chondromyxoid stroma present -> pleomorphic adenoma.
- Neoplastic cells embedded in stroma ("stromal invasion") = basal cell adenocarcinoma.
- Basal cell adenocarcinoma may be cytologically indistinguishable from basal cell adenoma, i.e. "bad" architecture makes it a basal cell adenocarcinoma.
DDx:
- Adenoid cystic carcinoma - not encapsulated.
- Basal cell adenocarcinoma - not encapsulated.
- Canalicular adenoma - different site; canalicular adenoma is the in oral cavity, usually upper lip.
Images:
IHC
- Luminal stains +ve: CK7 +ve, CAM5.2 +ve.
- p63 +ve -- basal component.
- S100 +ve -- spindle cells in the stroma.
Canalicular adenoma
General
- Exclusively oral cavity.
- 80% of lesions on upper lip.
Microscopic
Features:
- Channels - "beading of cell".
- Mucoid/hemorrhagic stroma.
DDx:
- Basal cell adenoma.
Images:
- Canalicular adenoma - low mag. (webpathology.com).
- Canalicular adenoma - high mag. (webpathology.com).
IHC
- p63 -ve.
- Basal cell adenoma p63 +ve.
Warthin tumour
Sebaceous adenoma
- Benign counterpart of sebaceous carcinoma.
Sebaceous lymphadenoma
General
- Rare salivary gland tumour.[19]
- Benign.
Microscopic
Features:[19]
- Sebaceous glands within lymphoid tissue - key feature.
DDx:[20]
- Warthin tumour.
- Sebaceous lymphadenocarcinoma.
- Mucoepidermoid carcinoma.
- Lymphoma.
Images
www:
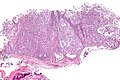
Oncocytoma of the salivary gland
- AKA salivary gland oncocytoma.
General
- No risk of malignant transformation.
- ~1% of all salivary gland tumours.
- Typical age: 60s-80s.
- Associated with radiation exposure.
- Major salivary glands - usually parotid gland.[21]
Gross
- Golden brown appearance.
Image
Microscopic
Features:
- Like oncocytomas elsewhere.
- Eosinophilic cytoplasm (on H&E stain).
- Due to increased number of mitochrondria.
- Fine capillaries.
- Eosinophilic cytoplasm (on H&E stain).
- Architecture: solid sheets, trabeculae or duct-like structure.[21]
Notes:
- May have clear cell change.
- Multiple small incidental lesions = oncocytosis - not oncocytoma.
DDx:
Images
www:
IHC
- p63 +ve[22] focally in nucleus.
Malignant
One approach:
- Differentiate -- luminal vs. myoepithelial vs. basal (mucoepideroid).
Mucoepidermoid carcinoma
Acinic cell carcinoma
Adenoid cystic carcinoma
- See: Adenoid cystic carcinoma of the breast for the breast tumour.
Salivary duct carcinoma
Polymorphous low-grade adenocarcinoma
- Abbreviated PLGA.
Carcinoma ex pleomorphic adenoma
- Abbreviated Ca ex PA.
Epithelial-myoepithelial carcinoma
Basal cell adenocarcinoma
Sebaceous carcinoma
It is similar to the tumour found in the skin.
Hyalinizing clear cell carcinoma
See also
References
- ↑ http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Oral/oral.htm#LABSALIVA
- ↑ http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Epithelia/Epithel.htm
- ↑ URL: http://dictionary.reference.com/browse/demilune. Accessed on: 19 August 2011.
- ↑ URL: http://pathology.mc.duke.edu/research/pth225.html. Accessed on: 19 August 2011.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 295-319. ISBN 978-0443069604.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 325-357. ISBN 978-0443069604.
- ↑ URL: http://emedicine.medscape.com/article/882358-overviewhttp://emedicine.medscape.com/article/882358-overview. Accessed on: 10 January 2011.
- ↑ Beasley, MJ. (Apr 2012). "Lymphoma of the Thyroid and Head and Neck.". Clin Oncol (R Coll Radiol). doi:10.1016/j.clon.2012.02.010. PMID 22475637.
- ↑ URL: http://emedicine.medscape.com/article/1076717-workup. Accessed on: 6 March 2012.
- ↑ Seifert, G.; Donath, K.; von Gumberz, C. (Jun 1981). "[Mucoceles of the minor salivary glands. Extravasation mucoceles (mucus granulomas) and retention mucoceles (mucus retention cysts) (author's transl)].". HNO 29 (6): 179-91. PMID 7251405.
- ↑ Barnes, L.; Appel, BN.; Perez, H.; El-Attar, AM. (Jan 1985). "Myoepithelioma of the head and neck: case report and review.". J Surg Oncol 28 (1): 21-8. PMID 2982059.
- ↑ Saksela, E.; Tarkkanen, J.; Wartiovaara, J. (Sep 1972). "Parotid clear-cell adenoma of possible myoepithelial origin.". Cancer 30 (3): 742-8. PMID 5075358.
- ↑ Kutzner, H.; Mentzel, T.; Kaddu, S.; Soares, LM.; Sangueza, OP.; Requena, L. (Mar 2001). "Cutaneous myoepithelioma: an under-recognized cutaneous neoplasm composed of myoepithelial cells.". Am J Surg Pathol 25 (3): 348-55. PMID 11224605.
- ↑ 14.0 14.1 Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 130. ISBN 978-0470519035.
- ↑ I. Weinreb. 24 October 2011.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 18. ISBN 978-0470519035.
- ↑ Choi, HR.; Batsakis, JG.; Callender, DL.; Prieto, VG.; Luna, MA.; El-Naggar, AK. (Jun 2002). "Molecular analysis of chromosome 16q regions in dermal analogue tumors of salivary glands: a genetic link to dermal cylindroma?". Am J Surg Pathol 26 (6): 778-83. PMID 12023583.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com/Com304-3-Diss.htm. Accessed on: 25 October 2011.
- ↑ 19.0 19.1 Mishra, A.; Tripathi, K.; Mohanty, L.; Nayak, M.. "Sebaceous lymphadenoma of the parotid gland.". Indian J Pathol Microbiol 54 (1): 131-2. doi:10.4103/0377-4929.77364. PMID 21393895. http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2011;volume=54;issue=1;spage=131;epage=132;aulast=Mishra.
- ↑ While, B.; Whiteside, OJ.; Desai, V.; Gurr, P. (Aug 2010). "Sebaceous lymphadenoma: a case report and review of the literature.". Ear Nose Throat J 89 (8): E22-3. PMID 20737364.
- ↑ 21.0 21.1 Zhou, CX.; Gao, Y. (Dec 2009). "Oncocytoma of the salivary glands: a clinicopathologic and immunohistochemical study.". Oral Oncol 45 (12): e232-8. doi:10.1016/j.oraloncology.2009.08.004. PMID 19796983.
- ↑ 22.0 22.1 McHugh, JB.; Hoschar, AP.; Dvorakova, M.; Parwani, AV.; Barnes, EL.; Seethala, RR. (Dec 2007). "p63 immunohistochemistry differentiates salivary gland oncocytoma and oncocytic carcinoma from metastatic renal cell carcinoma.". Head Neck Pathol 1 (2): 123-31. doi:10.1007/s12105-007-0031-4. PMC 2807526. PMID 20614263. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2807526/.