Pneumonia
Jump to navigation
Jump to search
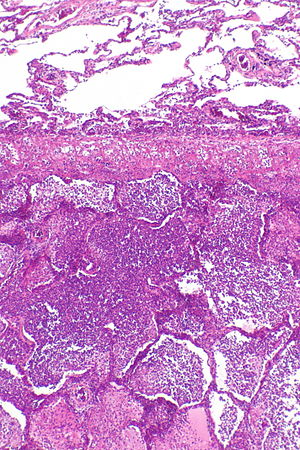
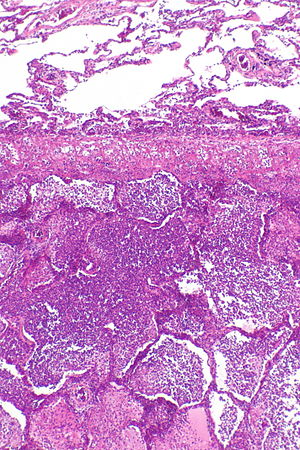
Acute pneumonia. H&E stain. (WC)
Pneumonia is inflammation of the lung, which includes infectious and non-infectious etiologies.
It is a subset of the medical lung diseases. This article primarily deals with the infectious pneumonias.
Idiopathic interstitial pneumonias are listed at the bottom; they are dealt with in detail in the diffuse lung diseases article.
Infectious pnemonia
Anatomical classification of pneumonia
- Generally, not used by clinicians.
- Use of the terms without qualification is discouraged... as they do not make explicit the etiology.
Bronchopneumonia
- Multiple foci of (acute) inflammation involving the bronchi.
- This is the most common form of (infectious) pneumonia.
Lobar pneumonia
- Pneumonia that involves a whole lobe.
- Rarely seen in areas where antibiotic treatments are widely available.
Acute infectious pneumonia
Main article: Acute infectious pneumonia
The most common form of pneumonia. It is usually diagnosed clinically.
Chronic infectious pneumonia
General
Common microorganisms:[1]
- Nocardia.
- Actinomyces.
- Mycobacterium tuberculosis.
- Atypical mycobacterium, e.g. Mycobacterium avium-intracellulare.
- Histoplasma capsulatum.
- Coccidioides immitis.
- Blastomyces dermatitidis.
Note:
- All of the later ones are granulomatous.
Microscopic
Features:
- Inflammation.
- +/-Granulomas.
Aspiration pneumonia
Main article: Aspiration pneumonia
Cytomegalovirus pneumonia
Main article: Cytomegalovirus
General
- Immunodeficiency.
- Critical illness.[2]
Microscopic
Features:
- CMV nuclear changes:
- Large red nucleus with a pale halo.
- Eosinophilic granular cytoplasmic inclusions.
Images:
IHC
- CMV +ve -- cytoplasmic inclusions, large nucleus.
Diffuse lung diseases
Main article: Diffuse lung disease
- AKA idiopathic interstitial pneumonia.
Histologic pattern:
- Organizing pneumonia.
- Usual interstitial pneumonia.
- Nonspecific interstitial pneumonia.
- Lymphocytic interstitial pneumonia.
- Desquamative interstitial pneumonia.
- Diffuse alveolar damage.
See also
References
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 711. ISBN 978-1416031215.
- ↑ Limaye, AP.; Boeckh, M. (Nov 2010). "CMV in critically ill patients: pathogen or bystander?". Rev Med Virol 20 (6): 372-9. doi:10.1002/rmv.664. PMID 20931610.
- ↑ URL: http://www.pathologyoutlines.com/topic/lungnontumorCMV.html. Accessed on: 23 January 2012.