Muscularis propria invasion in the urinary bladder
The presence or absence of muscularis propria invasion in the urinary bladder is a very important determination, as the clinical management changes between T1 and T2:
- T1: usually conservative treatment (local excision).
- T2: radical treatment (cystectomy or cystoprostatectomy).
A thin layer of discontinous muscularis mucuosae (MM) is present and, especially if hypertrophic, may be confused with muscuaris propria (MP).
Staging of bladder cancer is dealt with in the bladder cancer staging article.
Muscle invasive bladder cancer redirects to this article and refers to invasion of the muscularis propria.
Bladder muscularis propria invasion and urinary bladder muscularis propria invasion redirect to this article.
General
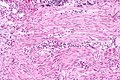
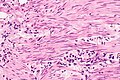
Comparing muscularis propria and muscularis mucosae
A comparison between muscularis propria and muscularis mucosae - adapted from Paner et al.:[1]
| Feature | Muscularis mucosae | Muscularis propria |
|---|---|---|
| Outline/border | typically irregular (frayed edges) | usually regular (circumscribed) |
| Size of bundles ‡ | classically "small", often "large" (hypertrophic) | usually "large" |
| Isolated fibres | yes | no |
| Location in bladder | less common in trigone, dome very common | everywhere |
| Depth † | superficial, occ. deep | deep |
Notes:
- † The lamina propria thickness varies with location. It is thinnest in the trigone (0.5-1.6 mm) and thickest in the dome (1.0-3.1 mm).
- ‡ Small is defined as <4 muscle fibres; large >= 4 muscle fibres.
- The presence of hyperplastic bundles ranges from ~20% in the trigone to ~70% in the dome.
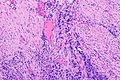
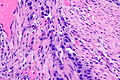
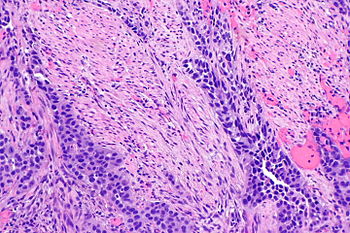
Images
Microscopic
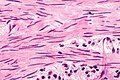
Rational assessment of muscularis propria invasion
To call muscularis propria invasion:
- Definite tumour must be between muscle.
- Muscle bundles must be thick.
- Multiple bundles must be adjacent to one another.
- Should not be superficial - surface epithelium if present should be distant.
DDx:
- Invasion of hypertrophic muscularis mucosae.
Images
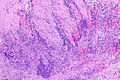
IHC
Smoothelin immunostain:[2]
- Muscularis propria - usu. strong. †
- Muscularis mucosae - negative/weak. †
Note:
- † Overlap between the patterns is described;[3] this limits the utility of the immunostain.
- Immunostain not used in many practice environments.
Sign out
Cannot exclude MP invasion
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE UROTHELIAL CARCINOMA. -- Extensive invasion into at least the lamina propria. - Negative for definite muscularis propria, see comment. Comment: The tumour is seen around bundles of smooth muscle that are favoured to represent muscularis mucosa; however, obliterated muscularis propria cannot be excluded. Correlation with the clinical findings is required. Additional transurethral sampling and/or imaging to assess the muscularis propria is suggested.
See also
References
- ↑ Paner, GP.; Ro, JY.; Wojcik, EM.; Venkataraman, G.; Datta, MW.; Amin, MB. (Sep 2007). "Further characterization of the muscle layers and lamina propria of the urinary bladder by systematic histologic mapping: implications for pathologic staging of invasive urothelial carcinoma.". Am J Surg Pathol 31 (9): 1420-9. doi:10.1097/PAS.0b013e3180588283. PMID 17721199.
- ↑ Paner, GP.; Shen, SS.; Lapetino, S.; Venkataraman, G.; Barkan, GA.; Quek, ML.; Ro, JY.; Amin, MB. (Jan 2009). "Diagnostic utility of antibody to smoothelin in the distinction of muscularis propria from muscularis mucosae of the urinary bladder: a potential ancillary tool in the pathologic staging of invasive urothelial carcinoma.". Am J Surg Pathol 33 (1): 91-8. doi:10.1097/PAS.0b013e3181804727. PMID 18936687.
- ↑ Miyamoto, H.; Sharma, RB.; Illei, PB.; Epstein, JI. (Mar 2010). "Pitfalls in the use of smoothelin to identify muscularis propria invasion by urothelial carcinoma.". Am J Surg Pathol 34 (3): 418-22. doi:10.1097/PAS.0b013e3181ce5066. PMID 20154589.