Nephrotic syndrome
(Redirected from MCD)
Jump to navigation
Jump to search
Nephrotic syndrome is a constellation of clinical findings seen in a number of medical kidney diseases. This article deals with them. It should not be confused with nephritic syndrome which has an almost identical spelling.
An introduction to the medical kidney is in the medical kidney diseases article. In children nephrotic syndrome is assumed to be minimal change disease. Biopsies are done only there is no response to steroids.
Clinical definition
Features:
- Anasarca (whole body - edema).
- Proteinuria (>3.5 g/24h).
- Hypercholesterolemia.
- Hypoalbuminemia.
Overview
Immune complex negative:
Immune complex positive:
Other:
- Pre-eclampsia.[3]
Specific entities
Minimal change disease
- Abbreviated MCD.
General
- Responds to steroids.
- Most common cause of nephrotic syndrome in children.
- Onset rapid when compared to FSGS.
- Proteinuria usually higher in FSGS.
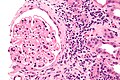
Microscopic
Features:
- No changes on light microscopy.
DDx:
- Focal segmental glomerulosclerosis - that is undersampled.
EM
Features:
- Diffuse loss of foot processes.
Note:
- Foot processes on urinary space side.
Image:
Focal segmental glomerulosclerosis
- Abbreviated FSGS.
General
- Presents as nephrotic syndrome.
- Does not respond to steroids (unlike MCD).
- Usually less rapid onset than MCD.
- Fibrosis usually takes some time.
Etiology
- Primary.
- May be familial.[4]
- Secondary.[5]
- HIV, parvovirus B19.[6]
- Drug use.
- Reduced renal mass.
| Feature | Primary | Secondary |
| Proteinuria (onset) | sudden | progressive |
| Albumnin | low | normal |
| Glomerulus size | normal | increased |
| Foot process effacement | diffuse | mild |
Notes:
- Primary FSGS needs ~70-80% foot process effacement.[7]
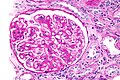
Microscopic
Features:
- Partial sclerosis of less than 50% of glomeruli.
- +/-Adhesions between the glomerular tuft and Bowman's capsule.
- +/-Glomerular enlargement.
DDx:
Images:
- www:
- WC:
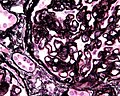
Histologic classification
FSGS can be subdivided into the following subgroups:[9]
| Subtype | Comment |
|---|---|
| Cellular | abrupt severe onset |
| Collapsing (AKA collapsing glomerulopathy[6]) | poor prognosis, viral/toxic etiology |
| Tip lesion | good prognosis |
| Perihilar | reduced renal mass |
| Not otherwise specified (NOS) | most common |
Stains
Features:[10]
- PAS +ve crescents.
IF
- No immune deposits.
- No IgG.
- No IgA.
Note:
- IgM, C3 - may be focally positive due to trapping.
EM
- Foot process loss.
- Secondary causes tend to have a thinner foot process width.
Membranous nephropathy
- AKA membranous glomerulonephritis.
- Abbreviated MN.
General
- Presents as nephrotic syndrome.
- Variable course.
- Pathogenesis: autoantibodies directed against phospholipase A2 receptor 1, abbreviated PLA2R.[11][12]
Clinical DDx:[13]
- Hepatitis B.
- Hepatitis C.
- Carcinoma.
- NSAID toxicity.
- SLE.
- Idiopathic.
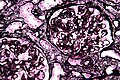
Microscopic
Features:
- Rigid (thickened) loop-like (glomerular) capillaries due to subepithelial immune complex deposition:
- Spikes or pinholes - seen on silver stain - key light microscopy feature.
- +/-Tram-tracking - seen in advanced lesions.
Note:
- Normal glomerular capillaries have a wavy wall with some undulation.
- Early lesions may have an essential normal appearance on light microscopy.
Lame memory device Oh ABCDEs:
- Nephrotic syndrome (caused by) autoimmune disorders, hepatitis B, cancer, drugs (with), subepithelial deposits & spikes.
Images
www:
IF
- Diffuse granular capillary loop - IgG, C3, kappa, lambda.
EM
- Diffuse subepithelial deposits - spike forming.
- The size of the deposits measured perpendicular to the basement membrane is smaller than seen in post-infectious glomerulonephritis (PIGN), and more diffuse. In other words, MN has a thin band-like deposits. PIGN has scattered tombstone-like ones.
Image:
C1q nephropathy
General
- Distinct entity[15] or a variant of focal segmental glomerulosclerosis (FSGS)[16] -- entity is controversial.[17]
- Nephrotic syndrome.
- Steroid resistant - like FSGS.[15]
- ANA -ve.
Microscopic
Features:
- +/-Focal segmental glomerulosclerosis.
- +/-Glomeular enlargement.
IF
- C1q +ve - key feature.
See also
References
- ↑ Komatsuda, A.; Wakui, H.; Yasuda, T.; Imai, H.; Miura, AB.; Tsuda, A.; Nakamoto, Y. (Nov 1994). "Successful delivery in a pregnant women with crescentic IgA nephropathy.". Intern Med 33 (11): 723-6. PMID 7849391.
- ↑ Kim, JK.; Kim, JH.; Lee, SC.; Kang, EW.; Chang, TI.; Moon, SJ.; Yoon, SY.; Yoo, TH. et al. (Mar 2012). "Clinical features and outcomes of IgA nephropathy with nephrotic syndrome.". Clin J Am Soc Nephrol 7 (3): 427-36. doi:10.2215/CJN.04820511. PMID 22322610.
- ↑ Wei, Q.; Zhang, L.; Liu, X. (Feb 2011). "Outcome of severe preeclampsia manifested as nephrotic syndrome.". Arch Gynecol Obstet 283 (2): 201-4. doi:10.1007/s00404-009-1338-z. PMID 20033418.
- ↑ Sánchez de la Nieta MD, Arias LF, Alcázar R, et al. (2003). "[Familial focal and segmentary hyalinosis]" (in Spanish; Castilian). Nefrologia 23 (2): 172–6. PMID 12778884.
- ↑ URL: http://www.kidneypathology.com/English_version/Focal_segmental_GS.html. Accessed on: 11 February 2011.
- ↑ Jump up to: 6.0 6.1 Schwimmer, JA.; Markowitz, GS.; Valeri, A.; Appel, GB. (Mar 2003). "Collapsing glomerulopathy.". Semin Nephrol 23 (2): 209-18. doi:10.1053/snep.2003.50019. PMID 12704581.
- ↑ Jump up to: 7.0 7.1 D'Agati, V. (Mar 2003). "Pathologic classification of focal segmental glomerulosclerosis.". Semin Nephrol 23 (2): 117-34. doi:10.1053/snep.2003.50012. PMID 12704572.
Cite error: Invalid
<ref>tag; name "pmid12704572" defined multiple times with different content - ↑ Noël, LH. (1999). "Morphological features of primary focal and segmental glomerulosclerosis.". Nephrol Dial Transplant 14 Suppl 3: 53-7. PMID 10382983.
- ↑ Thomas, DB.; Franceschini, N.; Hogan, SL.; Ten Holder, S.; Jennette, CE.; Falk, RJ.; Jennette, JC. (Mar 2006). "Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants.". Kidney Int 69 (5): 920-6. doi:10.1038/sj.ki.5000160. PMID 16518352.
- ↑ URL: http://www.kidneypathology.com/English_version/Focal_segmental_GS.html. Accessed on: 11 February 2011.
- ↑ Glassock, RJ. (Mar 2012). "The pathogenesis of membranous nephropathy: evolution and revolution.". Curr Opin Nephrol Hypertens. doi:10.1097/MNH.0b013e3283522ea8. PMID 22388552.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 604939
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 241. ISBN 978-1416002741.
- ↑ URL: http://missinglink.ucsf.edu/lm/IDS_102_cases_glomerular/Nephrotic_syndrome.htm. Accessed on: 2 April 2012.
- ↑ Jump up to: 15.0 15.1 Jennette, JC.; Hipp, CG. (Aug 1985). "C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome.". Am J Kidney Dis 6 (2): 103-10. PMID 3875286.
- ↑ Markowitz, GS.; Schwimmer, JA.; Stokes, MB.; Nasr, S.; Seigle, RL.; Valeri, AM.; D'Agati, VD. (Oct 2003). "C1q nephropathy: a variant of focal segmental glomerulosclerosis.". Kidney Int 64 (4): 1232-40. doi:10.1046/j.1523-1755.2003.00218.x. PMID 12969141.
- ↑ Reeves-Daniel, AM.; Iskandar, SS.; Bowden, DW.; Bostrom, MA.; Hicks, PJ.; Comeau, ME.; Langefeld, CD.; Freedman, BI. (May 2010). "Is collapsing C1q nephropathy another MYH9-associated kidney disease? A case report.". Am J Kidney Dis 55 (5): e21-4. doi:10.1053/j.ajkd.2009.10.060. PMID 20116156.