Lymphovascular invasion
Lymphovascular invasion, also lymphovascular space invasion, is (non-hematologic) malignant cells within blood vessels and/or lymphatics. It is abbreviated LVI.
In some contexts, vascular invasion (also angioinvasion) must be separated from lymphovascular invasion.[1]
The term lymphovascular invasion was traditionally preferred to vascular invasion, as it is difficult to differentiate morphologically small lymphatics and small vascular spaces, without immunohistochemistry.
General
- LVI, in the TNM staging system, does not affect tumour stage; however, there are exceptions.
- Exceptions:
- Seminoma.
- Squamous cell carcinoma of the penis.
- Intrahepatic bile duct carcinoma (cholangiocarcinoma).[2]
- Hepatocellular carcinoma.[3]
- Exceptions:
- Absence of LVI in the context of proven lymph node metastasis = sampling error.[4]
- The prognostic significance of LVI, generally, is dependent on the tumour type and may depend on the tumour stage and lymph node status.
- Most generally -- LVI = poorer prognosis.[5]
Specific tumours and LVI
| Tumour | Prognosis | Comment |
|---|---|---|
| Urothelial carcinoma | independent predictor of a poor prognosis in bladder tumours | LVI has more predictive power than tumour stage in the urinary bladder;[6] appears to be less important in upper urinary tract disease[7] |
| Breast cancer | not an independent predictor[8] | |
| Colorectal carcinoma | independent predictor of poorer prognosis (sporadic cancers)[9] | may be used as a quality measure; 25% of cases should have vascular invasion[10] |
Microscopic
Rosen criteria for LVI (in the breast):[11][12]
- Must be outside of the tumour proper.
- LVI is usually very close -- typically within 0.1 cm.
- Contour of cells should differ from possible vessel wall.
- DCIS with retraction artifact mimicing LVI has a contour that matches its surrounding fibrous tissue.
- Endothelium (usu. flat) should be visible.
- Lymphatics are found adjacent to blood vessels - vessels should be present in the vicinity.
Memory device LUBE-O:
- LVI has a Unique contour, Blood vessels and Endothelium in the vicinity, and is Outside of the tumour.
Notes:
- Criteria for LVI vary by the site/tumour.
- In some sites, the first criterium (tumour cells outside of the tumour proper) isn't required.
Images
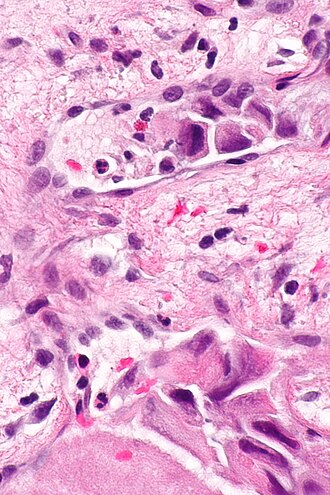
Small focus of LVI in a merkel cell carcinoma. (WC/Nephron)
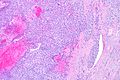
LVI - low mag. (WC/Nephron)
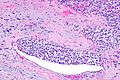
CRC with LVI - very low mag. (WC/Nephron)
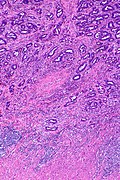
Stains
- Movat stain - especially useful in colorectal carcinoma so one can readily identify blood vessels.[13]
- Elastin stain.
Images
CRC with LVI - elastin - very low mag. (WC/Nephron)
IHC
Vascular markers:
- CD31.
- CD34.
Markers with high specific to lymphatic spaces:
See also
References
- ↑ Mete O, Erickson LA, Juhlin CC, de Krijger RR, Sasano H, Volante M, Papotti MG (March 2022). "Overview of the 2022 WHO Classification of Adrenal Cortical Tumors". Endocr Pathol 33 (1): 155–196. doi:10.1007/s12022-022-09710-8. PMC 8920443. PMID 35288842. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8920443/.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/IntrahepBileDucts_12protocol_3101.pdf. Accessed on: 23 May 2013.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Hepatocellular_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ Han, JS.; Molberg, KH.; Sarode, V.. "Predictors of invasion and axillary lymph node metastasis in patients with a core biopsy diagnosis of ductal carcinoma in situ: an analysis of 255 cases.". Breast J 17 (3): 223-9. doi:10.1111/j.1524-4741.2011.01069.x. PMID 21545433.
- ↑ Moreira, LF.; Kenmotsu, M.; Gochi, A.; Tanaka, N.; Orita, K. (1999). "Lymphovascular and neural invasion in low-lying rectal carcinoma.". Cancer Detect Prev 23 (2): 123-8. PMID 10101593.
- ↑ Cheng, L.; Montironi, R.; Davidson, DD.; Lopez-Beltran, A. (Jun 2009). "Staging and reporting of urothelial carcinoma of the urinary bladder.". Mod Pathol 22 Suppl 2: S70-95. doi:10.1038/modpathol.2009.1. PMID 19494855.
- ↑ Kim, HS.; Kim, M.; Jeong, CW.; Kwak, C.; Kim, HH.; Ku, JH. (Jun 2014). "Presence of lymphovascular invasion in urothelial bladder cancer specimens after transurethral resections correlates with risk of upstaging and survival: A systematic review and meta-analysis.". Urol Oncol. doi:10.1016/j.urolonc.2014.05.008. PMID 24954108.
- ↑ Ejlertsen, B.; Jensen, MB.; Rank, F.; Rasmussen, BB.; Christiansen, P.; Kroman, N.; Kvistgaard, ME.; Overgaard, M. et al. (May 2009). "Population-based study of peritumoral lymphovascular invasion and outcome among patients with operable breast cancer.". J Natl Cancer Inst 101 (10): 729-35. doi:10.1093/jnci/djp090. PMID 19436035.
- ↑ Lim, SB.; Yu, CS.; Jang, SJ.; Kim, TW.; Kim, JH.; Kim, JC. (Apr 2010). "Prognostic significance of lymphovascular invasion in sporadic colorectal cancer.". Dis Colon Rectum 53 (4): 377-84. doi:10.1007/DCR.0b013e3181cf8ae5. PMID 20305435.
- ↑ Messenger, DE.; Driman, DK.; Riddell, R.; McLeod, R.; Kirsch, R. (2012). [http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/ "Is Venous Invasion in Colorectal Cancer an Under-Reported Finding among Canadian Pathologists? Results of a Population-Based Survey of Ontario Pathologists."]. Can J Pathol 2 (4): 46-9. http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/.
- ↑ Rosen, PP. (1983). "Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance.". Pathol Annu 18 Pt 2: 215-32. PMID 6674861.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2009/InvasiveBreast_09protocol.pdf. Accessed on: 5 August 2011.
- ↑ Howlett, CJ.; Tweedie, EJ.; Driman, DK. (Nov 2009). "Use of an elastic stain to show venous invasion in colorectal carcinoma: a simple technique for detection of an important prognostic factor.". J Clin Pathol 62 (11): 1021-5. doi:10.1136/jcp.2009.065615. PMID 19861561.