Squamous cell carcinoma of the head and neck
| Squamous cell carcinoma of the head and neck | |
|---|---|
| Diagnosis in short | |
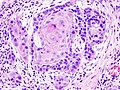
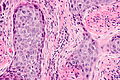
 Squamous cell carcinoma of the head and neck (larynx). H&E stain. | |
|
| |
| Synonyms | squamous cell carcinoma of the head and neck not otherwise specified |
| Subtypes | keratinizing type, undifferentiated type, nonkeratinizing type |
| LM DDx | squamous dysplasia of the head and neck, HPV-associated head and neck squamous cell carcinoma, nasopharyngeal carcinoma, malignant melanoma, metastatic squamous cell carcinoma (esp. skin SCC of lateral head), NUT carcinoma, pseudoepitheliomatous hyperplasia |
| IHC | p63 +ve, CK5/6, p16 -ve, EBER -ve |
| Site | head and neck - tongue (dealt with separately) |
|
| |
| Clinical history | smoking, excessive drinking |
| Prevalence | common |
| Prognosis | moderate-to-poor |
| Treatment | surgery, radiation |
Squamous cell carcinoma of the head and neck, abbreviated head and neck SCC, is a common malignant epithelium neoplasm of the head and neck.
This is an overview article that deals only with the usual squamous cell carcinoma of the head and neck, or squamous cell carcinoma of the head and neck not otherwise specified (abbreviated SCC of the H&N NOS).
Tongue squamous cell carcinoma is dealt with in separate article.
The human papilloma virus-associated SCC is dealt with in HPV-associated head and neck squamous cell carcinoma. Nasopharyngeal carcinoma is also dealt with separately.
General
- Most common malignant tumour of the head & neck.
- Most common spindle cell tumour of the head & neck.
Classification
SCC is subdivided by the WHO into:[1]
- Keratinizing type (KT).
- Worst prognosis.
- Undifferentiated type (UT).
- Intermediate prognosis.
- EBV association.
- Nonkeratinizing type (NT).
- Good prognosis.
- EBV association.
Microscopic
Features based on classification:[1]
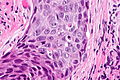
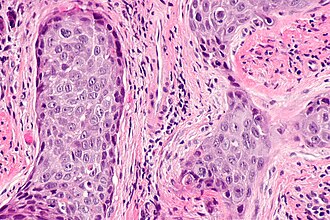
- Keratinizing type (KT) subtype:
- Keratinization & intercellular bridges through-out most of the malignant lesion.
- Undifferentiated type (UT):
- Non-distinct borders/syncytial pattern.
- Nucleoli.
- Nonkeratinizing (NT):
- Well-defined cell borders.
DDx:
- SMARCB1-deficient sinonasal carcinoma.
- Sinonasal undifferentiated carcinoma.
- Human papillomavirus-related multiphenotypic sinonasal carcinoma - previously known as HPV-related carcinoma with adenoid cystic-like features.
- NUT carcinoma - has well-differentiated squamous "islands" that are sharply demarcated from poorly differentiated surrounding tumour.
- Neuroendocrine tumour.
- Metastatic squamous cell carcinoma of skin - esp. parotid lesions, history of skin SCC (esp. lateral aspect of head).[2]
- Pseudoepitheliomatous hyperplasia.
Invasion
Features:
- Eosinophilia.
- Extra large nuclei/bizarre nuclei.
- Inflammation (lymphocytes, plasma cells).
- Long rete ridges.
- Numerous beeds/blobs of epithelial cells that seem unlikely to be rete ridges.
Pitfalls:
- Tangential cuts.
- If you can trace the squamous cells from a gland to the surface it is less likely to be invasive cancer.
Notes on invasion:
- Reviewed by Wenig.[3]
- See SCC of the cervix versus CIN III.
Images
Overview of subtypes
There are several subtypes:[4]
- Basaloid - poor prognosis, usu. diagnosed by recognition of typical SCC.
- Warty (Condylomatous).
- Verrucous - good prognosis, rare.
- Papillary.
- Lymphoepithelial, rare.
- Spindle cell, a common spindle cell lesion of the H&N.
Verrucous squamous cell carcinoma
Features:
- Exophytic growth.
- Well-differentiated.
- "Glassy" appearance.
- Pushing border.
DDx: papilloma.
Spindle cell squamous carcinoma
- Key to diagnosis is finding a component of conventional squamous cell carcinoma.
IHC:
- Typically keratin -ve.
- p63 +ve.
DDx:
- Spindle cell melanoma.
- Mesenchymal neoplasm.
Basaloid squamous cell carcinoma
- May mimic adenoid cystic carcinoma.
- Classically base of tongue.[5]
- Typically poor prognosis.
Features:
- Need keratinization. (???)
Lymphoepithelial (squamous cell) carcinoma
IHC
- p63 +ve.
- p16 -ve.
- Positive suggests HPV-associated head and neck squamous cell carcinoma.
- Bcl2 +ve/-ve.
- Positive = poor prognosis.[6]
Molecular
- EBER -ve.
- Positive suggests nasopharyngeal carcinoma.
Sign out
LESION, TONGUE/FLOOR OF MOUTH BORDER, BIOPSY: - INVASIVE KERATINIZING SQUAMOUS CELL CARCINOMA, MODERATELY DIFFERENTIATED.
LEFT NECK (LONG SUTURE LEVEL IA AND SHORT SUTURE LEVEL IIB), LEVEL I-IV, DISSECTION: - LEVEL IA: -- ONE LYMPH NODE WITH SQUAMOUS CELL CARCINOMA, AND FOUR LYMPH NODES NEGATIVE FOR MALIGNANCY (1 POSITIVE/5). -- BENIGN SALIVARY GLAND. -- SEE COMMENT. - LEVEL IIA: -- FIVE LYMPH NODES NEGATIVE FOR MALIGNANCY (0 POSITIVE/5). - LEVEL III: -- FIVE LYMPH NODES NEGATIVE FOR MALIGNANCY (0 POSITIVE/5). - LEVEL IV: -- TEN LYMPH NODES NEGATIVE FOR MALIGNANCY (0 POSITIVE/10). COMMENT: The squamous cell carcinoma is moderately differentiated and shows rare keratinization. The tumour lies adjacent to benign (submandibular) salivary gland which it does not involve.
Micro
Biopsy
The section shows atypical (squamous) cells with moderate grey cytoplasm, central nuclei with small nucleoli, infiltrating between fibrous tissue. Abundant keratin pearls are present. The nuclei are predominantly pale staining and focally have irregular nuclear membranes and irregular chromatin. Mitotic activity is not readily apparent. Necrosis is present focally.
See also
References
- ↑ 1.0 1.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 975. ISBN 978-0781740517.
- ↑ Vauterin TJ, Veness MJ, Morgan GJ, Poulsen MG, O'Brien CJ (September 2006). "Patterns of lymph node spread of cutaneous squamous cell carcinoma of the head and neck". Head Neck 28 (9): 785–91. doi:10.1002/hed.20417. PMID 16783833.
- ↑ Wenig BM (March 2002). "Squamous cell carcinoma of the upper aerodigestive tract: precursors and problematic variants". Mod. Pathol. 15 (3): 229–54. doi:10.1038/modpathol.3880520. PMID 11904340. http://www.nature.com/modpathol/journal/v15/n3/pdf/3880520a.pdf.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970297-2. Accessed on: March 9, 2010.
- ↑ URL: http://www.biomedcentral.com/1471-2407/6/146. Accessed on: March 9, 2010.
- ↑ Nichols AC, Finkelstein DM, Faquin WC, et al. (April 2010). "Bcl2 and human papilloma virus 16 as predictors of outcome following concurrent chemoradiation for advanced oropharyngeal cancer". Clin. Cancer Res. 16 (7): 2138–46. doi:10.1158/1078-0432.CCR-09-3185. PMID 20233885.