Eye
The eye is rarely seen by pathologists. Typically, they go to neuropathologists, as the eye is really part of the brain. The article also covers many of the lesions found around the eye. The lacrimal gland is covered in the lacrimal gland article. Eyelid lesions are covered in the eyelid article.
An introduction to neuropathology is in the neuropathology article.
Procedures
- Evisceration - eye muscles left intact.
- Enucleation.
- Exenteration - extensive resection.
Anatomy
Anterior to posterior
- Cornea.
- Iris.
- Lens.
- Conjunctiva - edge of cornea.
- Sclera.
- Similar to cornea - normally has blood vessels.
Optic nerve
- Surrounded by CSF.
- Covered by dura.
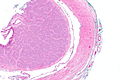
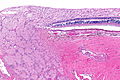
Images
Inside to outside
- Retina.
- Retinal pigment epithelium (RPE).
- Choroid.
- Sclera.
Image
Anterior angle
- Angle between cornea and iris.
Canthi
The canthi are where the upper and lower eyelids meet:
- Medial canthus.
- Lateral canthus.
Note:
- The most common malignant canthus lesion is basal cell carcinoma.[1]
Histology
Eye muscles
- The muscles that move the eye have a high nerve:muscle ratio = ~1:4.[2]
- Other muscles in the body ~1:250.
Conjunctiva
Features:[3]
- Stratified squamous.
- May be stratified columnar
- Goblet cells.
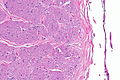
Cornea
Layers:[4]
- Epithelium layer.
- Squamoid cells.
- Bowman's layer.
- Indistinct.
- Stroma.
- Fibrous tissue.
- No blood vessels.
- Descemet’s layer.
- Indistinct.
- PAS -ve.
- Endothelium.
- Single layer.
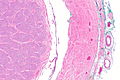
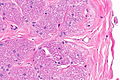
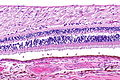
Retina
Simplified structure - eosinophilic material separating:
- Intermediate size, round, pale-staining nuclei (ganglion cells).
- Two layers of small round nuclei (inner and outer nuclear layer).
- Eosinophilic ellipsoid structures - rods/cones (photoreceptors).
- Single layer of cuboidal cells (retinal pigment epithelium.
Detailed structure - in direction light travels:
- Inner limiting membrane.
- Nerve fibre layer.
- Ganglion layer.
- Inner plexiform layer.
- Inner nuclear layer.
- Outer plexiform layer.
- Outer nuclear layer.
- Layer of rods and cones.
- External limiting membrane.
- Retinal pigment epithelium.
Images
Retina - high mag. (WC)
www:
Eye structures with melanocytes
Melanoma may arise from these sites:
- Iris.
- Conjunctiva.
- Ciliary bodies.
- Choroid.
Benign entities
Conjunctivitis
General
- Benign.
- Never biopsied.
- It is an incidental finding in a biopsy for something else.
Gross
- Red eye.
Microscopic
Features:
- Conjunctival epithelium - stratified squamous epithelium with goblet cells.
- Inflammatory cells.
Conjunctival cyst
| Conjunctival cyst | |
|---|---|
| External resources | |
| EHVSC | 10173 |
General
- Rare.
- May be due to surgery, trauma, or congenital (very rare).[5]
Microscopic
Features:
- Conjunctival mucosa with atypia.
- Stratified squamous epithelium with goblet cells.
DDx:
- Ocular surface squamous neoplasia.
- Cystic squamous cell carcinoma.
Image:
Sign out
CONJUNCTIVA, RIGHT SUPERIOR, BIOPSY: - BENIGN CONJUNCTIVAL MUCOSA -- COMPATIBLE WITH CYST LINIG.
Pinguecula
- Plural Pingueculae.
General
- Raizada et al.[7] suggest it is an early pterygium; however, this is disputed.
- Due to ultraviolet light exposure, e.g. sunlight.[8]
- Tend to be older than individuals afflicted with a pterygium.
Gross
- Yellow spot.
Microscopic
Features:
- Similar to pterygium.[8]
Pterygium
- AKA surfer eye.
Eccrine hidrocystoma
- Occasionally spelled eccrine hydrocystoma.[9]
Chalazion
Retinal hemorrhage
Image:
Glaucoma
General
- Leading cause of irreversible blindness.
Classification:
- Open angle - more common.
- Closed angle.
Microscopic
Features (closed angle):
- Cornea and iris opposed to one another.
Retinal detachment
General
- Blindness.
Causes:
- Trauma (classic) - pathologist doesn't usually see.
- Tumours - common in pathology specimens.
Microscopic
Features:
- Retina separated from retinal pigment epithelium.
- Eosinophilic exudate containing macrophages.
Blepharochalasis
General
Clinical:
- Swelling of eyelids - recurrent.[12]
- Onset in childhood.
- Leads to ptosis.
Clinical DDx:[11]
- Recurrent angioedema.
- Hereditary angioedema.
- Contact dermatitis.
- Melkersson-Rosenthal syndrome.
- Dermatochalasis.
- Floppy-eyelid syndrome.
- Lax eyelid syndrome.
- Cutis laxa.
Note:
- The term may be abused; it may be used when an eyelid tuck is done for other reasons.[citation needed]
Microscopic
Features:[11]
- Edema.
DDx:
- Angioedema.[13]
Stains
- Elastin stain - shows loss of elastin.[14]
Sign out
EYELID, LEFT UPPER, PTOSIS REPAIR: - SQUAMOUS EPITHELIUM WITHIN NORMAL LIMITS. - SUBEPITHELIAL TISSUE WITH MILD EDEMA. - SOLAR ELASTOSIS. - NEGATIVE FOR MALIGNANCY.
Lower eyelids in an older individual labelled blepharochalasis
A. EYELID, LEFT LOWER, BLEPHAROPLASTY: - BENIGN SKIN WITH MILD SOLAR ELASTOSIS. - BENIGN SKELETAL MUSCLE AND ADIPOSE TISSUE. - NEGATIVE FOR MALIGNANCY. B. EYELID, RIGHT LOWER, BLEPHAROPLASTY: - BENIGN SKIN WITH MILD SOLAR ELASTOSIS. - BENIGN SKELETAL MUSCLE AND ADIPOSE TISSUE. - NEGATIVE FOR MALIGNANCY.
Papilloma of the caruncle
Corneal ulcer
Keratoconus
Corneal scar
General
- Trauma to the cornea.
Microscopic
Features:
- Compact hyaline tissue - darker staining.
- Fibroblasts.
DDx:
- Squamous dysplasia.
Sign out
Corneal Button, Right Eye, Keratoplasty: - Consistent with corneal scar. - NEGATIVE for dysplasia.
Conjunctival nevus
Tumours of the eye
Optic glioma
General
- Associated with Neurofibromatosis type 1.
- Often nerve sheath thickening or tortuosity.
- Approx 3% of all pediatric gliomas.
- Histology in most cases a pilocytic astrocytoma.
Retinoblastoma
Malignant melanoma
Common malignancy in the eye in adults.
See also
References
- ↑ URL: https://iovs.arvojournals.org/article.aspx?articleid=2372910. Accessed on: 2022 Nov 17.
- ↑ Bilbao. 24 November 2010.
- ↑ URL: http://www.lab.anhb.uwa.edu.au/mb140/corepages/eye/eye.htm. Accessed on: 20 October 2011.
- ↑ URL: http://www.ophthobook.com/questions/question-name-the-layers-of-the-cornea-and-their-function. Accessed on: 26 January 2012.
- ↑ Robb, RM.; Elliott, AT.; Robson, CD. (Apr 2012). "Developmental conjunctival cyst of the eyelid in a child.". J AAPOS 16 (2): 196-8. doi:10.1016/j.jaapos.2012.02.001. PMID 22525180.
- ↑ Elshazly, LH. (Jan 2011). "A clinicopathologic study of excised conjunctival lesions.". Middle East Afr J Ophthalmol 18 (1): 48-54. doi:10.4103/0974-9233.75886. PMID 21572734.
- ↑ Raizada, IN.; Bhatnagar, NK. (Jul 1976). "Pinguecula and pterygium (a histopathological study).". Indian J Ophthalmol 24 (2): 16-8. PMID 1031388.
- ↑ 8.0 8.1 Hill, JC.; Maske, R. (1989). "Pathogenesis of pterygium.". Eye (Lond) 3 ( Pt 2): 218-26. doi:10.1038/eye.1989.31. PMID 2695353.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid10065300 - ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/fofrm.html. Accessed on: 6 December 2010.
- ↑ 11.0 11.1 11.2 11.3 Koursh, DM.; Modjtahedi, SP.; Selva, D.; Leibovitch, I.. "The blepharochalasis syndrome.". Surv Ophthalmol 54 (2): 235-44. doi:10.1016/j.survophthal.2008.12.005. PMID 19298902.
- ↑ Bergin, DJ.; McCord, CD.; Berger, T.; Friedberg, H.; Waterhouse, W. (Nov 1988). "Blepharochalasis.". Br J Ophthalmol 72 (11): 863-7. PMID 3207663.
- ↑ Wang, G.; Li, C.; Gao, T. (Apr 2009). "Blepharochalasis: a rare condition misdiagnosed as recurrent angioedema.". Arch Dermatol 145 (4): 498-9. doi:10.1001/archdermatol.2009.19. PMID 19380685.
- ↑ Kaneoya, K.; Momota, Y.; Hatamochi, A.; Matsumoto, F.; Arima, Y.; Miyachi, Y.; Shinkai, H.; Utani, A. (Jan 2005). "Elastin gene expression in blepharochalasis.". J Dermatol 32 (1): 26-9. PMID 15841657.