Pulmonary pathology

This article introduces pulmonary pathology and discusses an approach to lung specimens.
Medical lung disease is dealt with in the medical lung disease article. Tumours of the lung are dealt with in lung tumours article. Lung cytopathology is dealt with in the pulmonary cytopathology article.
Lung specimens
- CT-guided or ultrasound-guided needle core biopsy - for peripheral lesions.
- Transbronchial biopsy - for central lesions.
- "Open lung biopsy" - typically a video-assisted thoracic surgery (VATS) - done for diffuse lung diseases.
- These specimens should be sectioned to create pieces with a large surface area; ideally, it should be one large piece per block, so one can appreciate the architecture.
- Lobectomy - usually for cancer.
- Pneumonectomy - usually for cancer.
- Explantation - in the context of lung transplantation - done for cystic fibrosis Idiopathic pulmonary fibrosis and other causes.
Lung core biopsies
- Inadequacy rate for percutaneous biopsies ~5% in one series.[1]
- Length 0.5-1.5 cm enough for EGFR testing.[2]
Basic approach
All lung pathology can be grouped into one of six categories (as per Leslie). The radiology directly correlates to the pathologic grouping, except that air space disease encompasses three pathologic categories (ALI, CCI, AFD).
Pathologic groups:
| Lung pathology | |||||||||||||||||||||||||||||||||||||||||||||||
| Acute lung injury | Fibrosis | Chronic cellular infiltrates (ALI) | Alveolar filling defect (AFD) | Nodules | Near normal histology | ||||||||||||||||||||||||||||||||||||||||||
Identification of the groups:
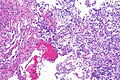
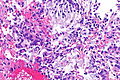
- Acute lung injury: hyaline membranes (very pink on H&E).
- Fibrosis = thick walls - pink on H&E.
- Chronic cellular infiltrates = inflammation (blue on H&E).
- Nodules = look at the history/radiology - should say mass or nodule.
- Alveolar filling defect = crap in the alveoli.
- Near normal = looks almost normal.
Radiologic groups:
| Lung radiology | |||||||||||||||||||||||||||||||
| Air space disease | Interstitial disease | Mass/nodules | Near normal | ||||||||||||||||||||||||||||
Radiologic-pathologic correlation:
- Air space disease (radiologic).
- Acute lung injury.
- Chronic cellular infiltrates.
- Alveolar filling defects.
- Interstitial disease (radiologic).
- Fibrosis.
- Mass/nodules (radiologic).
- Nodules.
- Near normal (radiologic).
- Near normal histology.
Most of the things that come to pathology are in the mass/nodules category and lung tumours (discussed below). The other categories are dealt with in the medical lung disease article.
Anatomical approach:
- Pleura - thickening?
- Airspace - filling?
- Alveolar walls - thickening?
- Airways - inflammation?
- Vessels - thickening?
Normal lung
- Benign lung redirects here.
Lung anatomy
Airway
- Bronchus = has cartilage.
- Bronchiole = non-cartilaginous airway.
Small airways
The trip to the alveolus:[3]
- Membranous bronchiole.
- Terminal bronchiole - dilation distal to this = emphysema.
- Respiratory bronchiole.
- Alveolar duct - dilated in ARDS.
- Alveolus.
Pleura
- Visceral pleura = covers the lung.[4]
- Parietal pleura = covers the chest wall.
Note:
- Pleural invasion is an important prognosticator in lung cancer and should be considered if the tumour is close to the pleura.
Lung lobule
Lung lobule:[5]
- Arterial vessels travels with the bronchus.
- Venules travel in the septae.
Note:
- Arterial vessels in the lung should be approximately the same size as its accompanying airway.[6]
Memory device:
- Arteries (which were once thought to contain air) are with the airway.
Lung histology
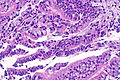
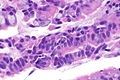
Bronchial mucosa
- Ciliated pseudostratified epithelium.
- Minimal/mild inflammation.
- Small amount of smooth muscle.
Metaplastic changes:
- Goblet cells - described in association asthma and COPD.[7]
- Squamous - may precede dysplasia and malignancy.
Lung parenchyma
Common:
- Type I pneumocyte - cover most of the alveolar surface.
- Type II pneumocyte - stem cell, produce surfactant.
- Typical location: "angle of alveolus".
- Macrophages.
Rare:
- Pulmonary neuroendocrine cells:[8]
- Histomorphology:
- Single cells.
- Small clusters ~ 6 cells ("neuroepithelial bodies").
- Identified with immunostains:
- Serotonin.
- Bombesin.
- Chromogranin A.
- Synaptic vesicle 2.
- Histomorphology:
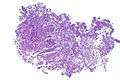
Images
www:
Sign out
Missed endobronchial biopsy
RIGHT UPPER LOBE, ENDOBRONCHIAL BIOPSY: - SMALL FRAGMENT OF BENIGN BRONCHIAL MUCOSA WITH INFLAMMATION. COMMENT: The clinical history of a mass is noted. This biopsy does not show neoplastic tissue; however, the biopsy may not be representative of the lesion seen.
Missed lung biopsy
Submitted as "Lung Mass" (Left Lower Lobe), Core Biopsy: - Tiny cluster of indeterminate cells insufficient for a diagnosis, see comment. - Benign lung parenchyma. - NEGATIVE for definite lesion. Comment: Deepers were cut (x3). The radiologic findings are noted. A re-biopsy is recommended.
Alternate
Lung, Left Lower Lobe, Endobronchial Biopsy: - Respiratory bronchiolitis. - Benign bronchial epithelium. - NEGATIVE for granulomatous inflammation. - NEGATIVE for evidence of mass lesion. Comment: Immunostains were done and compatible with bronchial epithelium (napsin negative, TTF-1 negative, CK7 positive, CK20 negative, CDX2 negative, beta-catenin membranous staining) and lung parenchyma (napsin positive, TTF-1 positive, CK7 positive, CK20 negative, CDX2 negative, beta-catenin membranous staining).
Pathology terminology
- Siderophages = mononuclear phagocyte with hemosiderin.[9]
- Hyaline membrane = glassy layering of an alveolus/small airways with material that is eosinophilic on H&E.[10]
- Entomology of Hyaline: "... of glass" (Greek).
- Image: Hyaline membrane (path.upmc.edu).
- Bronchiolization = ciliated (respiratory) epithelium or goblet cells in (distal) air space.[11]
- Image: Bronchiolization (ucsf.edu).
- Smoker's macrophages = brown-pigmented macrophages - assoc. with smoking.[12]
Detail articles
Malignancy - lung cancer
This pretty much always comes to the pathologist.
Medical lung disease
There are separate articles for:
Lung transplant pathology
Specific diagnoses
Bronchogenic cyst
General
- Benign.
- Usually in mediastinum or hilum.[13]
- Fit into the bigger category of foregut cyst.
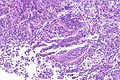
Microscopic
Features:[14]
- Cyst lined by respiratory epithelium.
Images
www:
Pulmonary hamartoma
Malformations
Come in three flavours:
- Congenital pulmonary airway malformation (CPAM).
- Extralobar sequestration (ELS).
- Intralobar sequestrations (ILS).
Congenital pulmonary airway malformation
- Previously known as congenital cystic adenomatoid malformation (CCAM).[15]
General:
- Classified according to density:[16]
- Type I = mostly large cysts.
- Type II = mostly small cysts.
- Type III = solid mass.
Gross
- Cystic or solid mass.
Image:
Microscopic
Features:[16]
- Irregular cystic spaces with bronchial epithelium.
- Bronchial epithelium = cilia, pseudostratified.
Extralobar sequestration
General:
- Typically not connected to airway tree/trachea.
- Blood supply arises from aorta, not the pulmonary artery.
- Mass lesion.
- Associated with other congenital anomalies.[13] The most common are diaphragmatic abnormalities - including congenital diaphragmatic hernia.[18]
Microscopic
Features:[16]
- Abnormal airways:
- Dilated irregularly shaped bronchi.
- Wavy luminal contour/undulating contour (normal ~ round/ovoid).
- Distal airways with ciliated epithelium.
- Dilated irregularly shaped bronchi.
- +/-Infection.
- +/-Interstitial fibrosis due to inflammation.
Image:
Intralobar sequestration
General:
- Classically identified due to recurrent infections or bronchiectasis.[13]
- Intralobular sequestration can be considered a variant of ELS; it is like an ELS but surrounded by normal lung.
Bronchopulmonary dysplasia
- Abbreviated BPD.
General
- Developmental.
- Assoc. with prematurity.[19]
Microscopic
Features:
- Large alveoli.
- Bronchiolar fibrosis.
- Interstitial fibrosis.
Images:
Pulmonary infarct
- AKA lung infarct, lung infarction, pulmonary infarction.
See also
References
- ↑ McSweeney, SE.; O'Regan, KN.; Mc Laughlin, PD.; Crush, L.; Maher, MM. (2012). "Evaluation of the efficacy and safety of percutaneous biopsy of lung.". Open Respir Med J 6: 82-8. doi:10.2174/1874306401206010082. PMID 22977650.
- ↑ Zhuang, YP.; Wang, HY.; Shi, MQ.; Zhang, J.; Feng, Y. (Dec 2011). "Use of CT-guided fine needle aspiration biopsy in epidermal growth factor receptor mutation analysis in patients with advanced lung cancer.". Acta Radiol 52 (10): 1083-7. doi:10.1258/ar.2011.110150. PMID 22006985.
- ↑ Hegele. 27 October 2009.
- ↑ URL: http://www.ouhsc.edu/histology/Glass%20slides/14_15.jpg. Accessed on: 10 October 2012.
- ↑ http://lib.hku.hk/denlib/exhibition/rarebook/mouth_hygiene_plate.jpg
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 266. ISBN 978-0443066313.
- ↑ Rogers DF (January 2003). "The airway goblet cell". Int J Biochem Cell Biol 35 (1): 1–6. doi:10.1016/s1357-2725(02)00083-3. PMID 12467641.
- ↑ Cutz E, Yeger H, Pan J (2007). "Pulmonary neuroendocrine cell system in pediatric lung disease-recent advances". Pediatr. Dev. Pathol. 10 (6): 419–35. doi:10.2350/07-04-0267.1. PMID 18001162.
- ↑ http://medical-dictionary.thefreedictionary.com/siderophore
- ↑ http://medical-dictionary.thefreedictionary.com/hyaline+membrane
- ↑ http://pathhsw5m54.ucsf.edu/case27/image277.html
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 236. ISBN 978-0443066313.
- ↑ 13.0 13.1 13.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 363. ISBN 978-1416054542.
- ↑ Chen, C.; Zheng, H. (Jun 2008). "Extralobar pulmonary sequestration in the hilum.". Asian Cardiovasc Thorac Ann 16 (3): 246-8. PMID 18515678. http://asianannals.ctsnetjournals.org/cgi/content/full/16/3/246.
- ↑ URL: http://radiopaedia.org/articles/congenital-pulmonary-airway-malformation. Accessed on: 10 February 2012.
- ↑ 16.0 16.1 16.2 Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 100. ISBN 978-1416002741.
- ↑ URL: http://www.humpath.com/spip.php?article8685&id_document=22510. Accessed on: 8 April 2012.
- ↑ Rosado-de-Christenson, ML.; Frazier, AA.; Stocker, JT.; Templeton, PA. (Mar 1993). "From the archives of the AFIP. Extralobar sequestration: radiologic-pathologic correlation.". Radiographics 13 (2): 425-41. PMID 8460228. http://radiographics.rsnajnls.org/cgi/pmidlookup?view=long&pmid=8460228.
- ↑ Chang, LW. (Sep 2011). "[Incidence and risk factors of bronchopulmonary dysplasia in premature infants in 10 hospitals in China].". Zhonghua Er Ke Za Zhi 49 (9): 655-62. PMID 22176899.