Brenner tumour
(Redirected from Brenner tumor)
Jump to navigation
Jump to search
| Brenner tumour | |
|---|---|
| Diagnosis in short | |
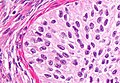
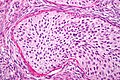
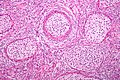
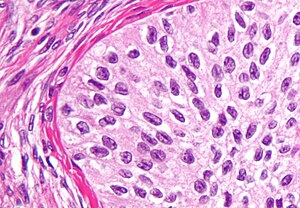 Brenner tumour. H&E stain. | |
|
| |
| LM | nests cells that have a "coffee bean nucleus" (nucleus = elliptical shape, nuclear groove along long axis), distinct nucleoli, moderate-to-abundant gray/pale cytoplasm, dense fibrous stroma around nests |
| Subtypes | benign (most common), borderline, malignant |
| LM DDx | granulosa cell tumour, ovarian fibroma, thecoma, Walthard cell rest |
| IHC | AR +ve, calretinin -ve |
| Gross | classically solid (may be cystic), usu. well-circumscribed, light yellow colour |
| Site | ovary (see ovarian tumours), fallopian tube |
|
| |
| Prevalence | uncommon |
| Prognosis | usu. good, may be poor |
The Brenner tumour, abbreviated BT, is an ovarian tumour in the epithelial group of ovarian tumours.
General
- Considered to be rare[1] - 1-2% of ovarian neoplasms.[2]
- Traditionally, BT has been grouped within the transistional cell tumours category in the surface epithelial group of ovarian tumours.
- Recently, transistional cell carcinoma of the ovary has been related to serous carcinoma; TCC of the ovary is probably distinct from the malignant Brenner tumour.[3]
- May arise from the fallopian tube.[4]
- Can be seen in the testis.[5]
Epidemiology
- Mostly benign clinical course - 99% of Brenner tumours benign.[6]
- Thought to arise from Walthard cell rest.
- Frequently an incidental finding, i.e. oophorectomy was done for another reason.
- May be malignant - rarely (~1% of Brenner tumours[7]).
Gross
Features:[8]
- Classically solid, well-circumscribed, light yellow.
- May be cystic.
Note:
- Borderline tumours classically solid and cystic with papillary projections into the cystic component.[8]
Microscopic
Features:
- Nests of transitional epithelium with cells that have:[9]
- A "coffee bean nucleus".
- Elliptical shape (nucleus).
- Nuclear grooves.
- Distinct nucleoli.
- Moderate-to-abundant gray/pale cytoplasm.
- A "coffee bean nucleus".
- Dense fibrous stroma around nests.
Notes:
- Main DDx of Coffee bean nucleus = granulosa cell tumour.
- Stromal component may be predominant.
Subclassification:
- Benign.
- Borderline.
- Malignant <5% of tumour.[10]
DDx:[6]
- Benign:
- Endometrioid adenofibroma.
- Ovarian fibroma.
- Borderline:
- Benign Brenner tumour.
- Malignant Brenner tumour.
- Metastatic papillary urothelial carcinoma.
- Malignant:
- Undifferentiated carcinoma - no Brenner tumour component.
- Granulosa cell tumour.
- Serous carcinoma.
- Metastatic urothelial carcinoma.
- Walthard cell rest - typically one nest of cells, lacks the surrounding fibromatous stroma.
Images
IHC
Features:[4]
See also
References
- ↑ Bilici, A.; Inanc, M.; Ulas, A.; Akman, T.; Seker, M.; Babacan, NA.; Inal, A.; Bal, O. et al. (2013). "Clinical and pathologic features of patients with rare ovarian tumors: multi-center review of 167 patients by the anatolian society of medical oncology.". Asian Pac J Cancer Prev 14 (11): 6493-9. PMID 24377556.
- ↑ Arnogiannaki, N.; Grigoriadis, C.; Zygouris, D.; Terzakis, E.; Sebastiadou, M.; Tserkezoglou, A. (2011). "Proliferative Brenner tumor of the ovary. clinicopathological study of two cases and review of the literature.". Eur J Gynaecol Oncol 32 (5): 576-8. PMID 22053680.
- ↑ Ali, RH.; Seidman, JD.; Luk, M.; Kalloger, S.; Gilks, CB. (Nov 2012). "Transitional cell carcinoma of the ovary is related to high-grade serous carcinoma and is distinct from malignant brenner tumor.". Int J Gynecol Pathol 31 (6): 499-506. doi:10.1097/PGP.0b013e31824d7445. PMID 23018212.
- ↑ 4.0 4.1 4.2 Kuhn, E.; Ayhan, A.; Shih, IeM.; Seidman, JD.; Kurman, RJ. (Dec 2013). "Ovarian Brenner tumour: a morphologic and immunohistochemical analysis suggesting an origin from fallopian tube epithelium.". Eur J Cancer 49 (18): 3839-49. doi:10.1016/j.ejca.2013.08.011. PMID 24012099.
- ↑ Amin MB (February 2005). "Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors". Mod. Pathol. 18 Suppl 2: S131–45. doi:10.1038/modpathol.3800314. PMID 15502808.
- ↑ 6.0 6.1 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 437. ISBN 978-0443069208.
- ↑ Gezginç, K.; Karatayli, R.; Yazici, F.; Acar, A.; Çelik, Ç.; Çapar, M.; Tavli, L. (Aug 2012). "Malignant Brenner tumor of the ovary: analysis of 13 cases.". Int J Clin Oncol 17 (4): 324-9. doi:10.1007/s10147-011-0290-7. PMID 21796330.
- ↑ 8.0 8.1 Borah, T.; Mahanta, RK.; Bora, BD.; Saikia, S. (Jan 2011). "Brenner tumor of ovary: An incidental finding.". J Midlife Health 2 (1): 40-1. doi:10.4103/0976-7800.83273. PMC 3156501. PMID 21897739. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3156501/.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1098. ISBN 0-7216-0187-1.
- ↑ Zhang Y, Staley SA, Tucker K, Clark LH (May 2019). "Malignant Brenner tumor of the ovary: Case series and review of treatment strategies". Gynecol Oncol Rep 28: 29–32. doi:10.1016/j.gore.2019.02.003. PMC 6378317. PMID 30815527. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6378317/.