Nodular hyperplasia of the prostate gland
(Redirected from Benign prostatic hyperplasia)
Jump to navigation
Jump to search
| Nodular hyperplasia of the prostate gland | |
|---|---|
| Diagnosis in short | |
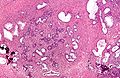
 Nodular hyperplasia of the prostate gland. H&E stain. | |
|
| |
| Synonyms | benign prostatic hyperplasia, benign prostatic hypertrophy (misnomer) |
|
| |
| LM | stromal and/or glandular hyperplasia |
| LM DDx | smooth muscle tumour of uncertain malignant potential, subtle prostate carcinoma |
| Gross | enlarged prostate gland, nodularity |
| Grossing notes | prostate chips, radical prostatectomy |
| Site | prostate gland |
|
| |
| Clinical history | old man |
| Signs | hematuria, weak urine stream, incomplete urinary emptying, post-void dribbling, prolonged voiding, intermittency, hesitancy |
| Symptoms | increased frequency of urination, straining |
| Prevalence | very common, esp. elderly |
| Blood work | +/-elevation of PSA (mild) |
| Prognosis | benign |
| Clin. DDx | other causes of hematuria (urothelial carcinoma, renal cell carcinoma, cystitis), other causes of obstruction (prostate carcinoma, urothelial carcinoma) |
| Treatment | medical, TURP, others |
Nodular hyperplasia of the prostate gland, also benign prostatic hyperplasia (abbreviated BPH), is a common benign pathology of the prostate gland.
It is also known as prostatic nodular hyperplasia. Occasionally, it is referred to as benign prostatic hypertrophy; this is a misnomer. This pathology is not a hypertrophy.
General
- Very common.
- Incidence increases with age.
Clinical - mnemonic I WISH 2p:[1]
- Intermittency.
- Weak stream.
- Incomplete emptying.
- Straining.
- Hesitancy.
- Post-void dribbling.
- Prolonged voiding.
Others:
- Hematuria - common.[2]
Treatment:
- Medications.
- Transurethral resection of the prostate (TURP).
- Rezum.[3]
- Laser treatment (GreenLight).[4]
Gross
- Enlargement of the prostate.
- Nodularity of the prostate.
Microscopic
Features:
- Stromal and/or glandular hyperplasia.
- Stromal component has small blood vessels.
Notes:
- Should not be diagnosed on core biopsy!
- One series suggests clinically relevant prostate cancer is seen in ~1.5% of resections for BPH.[5]
DDx:
- Urothelial carcinoma - significant nuclear atypia.
- Prostate carcinoma - especially low-grade.
- Prostatic stromal tumour of uncertain malignant potential - lacks small vessels.[6]
Images
Sign out
Urothelium present
Prostate Tissue, Transurethral Resection of Prostate (TURP): - Benign prostatic tissue with glandular and stromal proliferation. - Benign urothelial mucosa with inflammation. - NEGATIVE for malignancy.
Prostate Tissue, Transurethral Resection of Prostate (TURP): - Benign prostatic tissue. - Benign urothelial mucosa with mild inflammation and calcification. - NEGATIVE for malignancy.
Block letters
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION. - UROTHELIAL MUCOSA WITH A MILD LYMPHOCYTIC INFILTRATE. - NEGATIVE FOR MALIGNANCY.
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP) AND URINARY BLADDER NECK: - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION. - UROTHELIUM WITH THE CHANGES OF CYSTITIS CYSTICA ET GLANDULARIS. - NEGATIVE FOR MALIGNANCY.
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP) AND URINARY BLADDER NECK: - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION, AND FOCAL ACUTE AND CHRONIC INFLAMMATION. - UROTHELIUM WITH THE CHANGES OF CYSTITIS CYSTICA ET GLANDULARIS. - NEGATIVE FOR MALIGNANCY.
No urothelium present
PROSTATE GLAND, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION.
Post-TURP granuloma present
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION WITH PROMINENT BLOOD VESSELS AND SQUAMOUS METAPLASIA. - PALISADING GRANULOMA WITH NECROTIC CORE, SEE COMMENT. - UROTHELIAL MUCOSA WITH A MILD INFLAMMATORY INFILTRATE. - NEGATIVE FOR MALIGNANCY. COMMENT: This is morphologically consistent with a post-TURP granuloma.
See also
References
- ↑ Shiau, Carolyn; Toren, Andrew (2006). Toronto Notes 2006: Comprehensive Medical Reference (Review for MCCQE 1 and USMLE Step 2) (22nd edition (2006) ed.). Toronto Notes for Medical Students, Inc.. pp. U5. ISBN 978-0968592861.
- ↑ Sharp, VJ.; Barnes, KT.; Erickson, BA. (Dec 2013). "Assessment of asymptomatic microscopic hematuria in adults.". Am Fam Physician 88 (11): 747-54. PMID 24364522.
- ↑ Westwood J, Geraghty R, Jones P, Rai BP, Somani BK (November 2018). "Rezum: a new transurethral water vapour therapy for benign prostatic hyperplasia". Ther Adv Urol 10 (11): 327–333. doi:10.1177/1756287218793084. PMC 6180381. PMID 30344644. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6180381/.
- ↑ Campobasso D, Marchioni M, Altieri V, Greco F, De Nunzio C, Destefanis P, Ricciardulli S, Bergamaschi F, Fasolis G, Varvello F, Voce S, Palmieri F, Divan C, Malossini G, Oriti R, Tuccio A, Ruggera L, Tubaro A, Delicato G, Laganà A, Dadone C, De Rienzo G, Frattini A, Pucci L, Carrino M, Montefiore F, Germani S, Miano R, Schips L, Rabito S, Ferrari G, Cindolo L (January 2020). "GreenLight Photoselective Vaporization of the Prostate: One Laser for Different Prostate Sizes". J Endourol 34 (1): 54–62. doi:10.1089/end.2019.0478. PMID 31617419.
- ↑ Skrzypczyk, MA.; Dobruch, J.; Nyk, L.; Szostek, P.; Szempliński, S.; Borówka, A. (2014). "Should all specimens taken during surgical treatment of patients with benign prostatic hyperplasia be assessed by a pathologist?". Cent European J Urol 67 (3): 227-32. doi:10.5173/ceju.2014.03.art2. PMID 25247076.
- ↑ Hansel, DE.; Herawi, M.; Montgomery, E.; Epstein, JI. (Jan 2007). "Spindle cell lesions of the adult prostate.". Mod Pathol 20 (1): 148-58. doi:10.1038/modpathol.3800676. PMID 17170745.