Difference between revisions of "Vulva"
(→Hidradenoma papilliferum: split out) |
|||
| Line 149: | Line 149: | ||
==Hidradenoma papilliferum== | ==Hidradenoma papilliferum== | ||
*[[AKA]] ''papillary hidradenoma''.<ref>Hidradenoma papilliferum. Stedman's Medical Dictionary. 27th Ed.</ref> | *[[AKA]] ''papillary hidradenoma''.<ref>Hidradenoma papilliferum. Stedman's Medical Dictionary. 27th Ed.</ref> | ||
{{Main|papillary hidradenoma}} | |||
=Vulvar neoplasia= | =Vulvar neoplasia= | ||
Revision as of 04:28, 17 February 2014
This article addresses the basics of vulva, from a pathologic perspective.
A general differential diagnosis
Benign:
- Condyloma acuminatum.
- Bartholin cyst.
- Lichen sclerosus.
- Zoon vulvitis.
- Papillary hidradenoma.
- Extramammary Paget disease.
Other:
Premalignant:
Malignant:
- Vulvar squamous cell carcinoma.
- Malignant melanoma of the vulva.
Normal vulva
Microscopic
Features:
- Stratified squamous epithelium with maturation.
- No nuclear changes.
- No inflammation.
Sign out
Mildly inflamed
VULVA, BIOPSY: - SQUAMOUS MUCOSA WITH MILD CHRONIC INFLAMMATION AND REACTIVE CHANGES. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show squamous mucosa with a mild chronic inflammatory infiltrate that consists predominantly of lymphocytes. There is mild nuclear enlargement and intracellular edema. The nuclear membranes are regular. No nuclear hyperchromasia is apparent. No mitotic activity is readily apparent.
Benign disease
This is grab bag of non-neoplastic stuffs.
Condyloma acuminatum
General
- Due to human papillomavirus (HPV).
- Transmission: sexual, non-sexual, horizontal (mother to child).[1]
- Should raise the suspicion of child abuse.
- Transmission: sexual, non-sexual, horizontal (mother to child).[1]
Note:
- Related to verruca vulgaris (common wart).
- The Bethesda system includes this in LSIL.[2]
Clinical DDx:
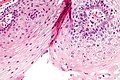
Microscopic
Features:
- Koilocytes.[4]
- Cells with an enlarged nucleus and perinuclear clearing.
- Papillomatosis.[5]
- Papillomatosis = surface elevation due to dermal papillae enlargement.[6]
- +/-Parakeratosis.
DDx:
- Classic vulvar intraepithelial neoplasia - architecture different.
Images
Sign out
SKIN LESION ("VULVAR WART"), VULVA, EXCISION:
- CONDYLOMA ACUMINATUM (GENITAL WART).
LABIA MINORA, BIOPSY: - CONDYLOMA/LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL). -- NEGATIVE FOR HIGH-GRADE DYSPLASIA.
Seborrheic keratosis-like
SKIN LESION, PERINEUM, BIOPSY: - SEBORRHEIC KERATOSIS-LIKE CONDYLOMA ACUMINATUM (GENITAL WART).
Without viral cytopathic changes
VULVAR LESIONS (x3), EXCISION: - SQUAMOUS HYPERPLASIA WITH HYPERORTHOKERATOSIS WITHOUT VIRAL CYTOPATHIC EFFECT, COMPATIBLE WITH CONDYLOMA (x3). - NEGATIVE FOR MALIGNANCY.
Micro
The sections show a polypoid fragment of skin with epithelium on three sides, acanthosis, hyperkeratosis and parakeratosis. Koilocytic changes (mild nuclear enlargement, perinuclear clearing) are seen focally. There is mild basilar nuclear enlargement and hyperchromasia. The epithelium matures to the surface and a granular layer is present.
Seborrheic keratosis-like
The sections show skin with acanthosis with papillomatous features (round bulbous rete ridges, acanthosis with penetrating fibrovascular cores) pseudohorn cysts, parakeratosis and hyperkeratosis. There is no significant basal nuclear atypia. There are no mitoses and no melanocytic nests. There is mild dermal inflammation. There is no solar elastosis. Pigment incontinence is present focally.
Lichen sclerosus
Bartholin cyst
General
- Common.
- May become infected.
Treatment:
- Drainage.
- Marsupialization.
Microscopic
Features:
- Cyst with squamous or urothelial epithelium.[7]
Images:
Sign out
Compatible with Bartholin cyst
VAGINA, CYST WALL, BIOPSY: - SOFT TISSUE WITH A MIXED INFLAMMATORY INFILTRATE RICH IN NEUTROPHILS, NO EPITHELIUM APPARENT; COMPATIBLE WITH DENUDED CYST WALL. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Zoon vulvitis
- AKA plasma cell vulvitis.
Neoplasms (non-malignant)
A short DDx:[8]
Hidradenoma papilliferum
Vulvar neoplasia
Classic vulvar intraepithelial neoplasia
- Abbreviated classic VIN or cVIN.
General
Epidemiology:
- Classic VIN, like CIN, is associated with HPV and seen in younger women.
- May be multifocal, i.e. associated with cervical (CIN) or vaginal (VAIN) lesions;[10] multifocality has a strongly association with immunosuppression.[11]
Classic VIN is graded like cervical pre-cancerous lesions:
- VIN I.
- DDx: condyloma acuminatum.[12]
- Uncommon.
- VIN II.
- Not common.
- VIN III.
- Commonly seen.
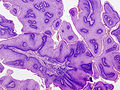
Microscopic
Features:
- Increased NC ratio.
- Multinucleation.
- Lack of maturation to surface (not very useful -- unlike in the cervix).[13]
- May have "vertical streaming" - the long axis of the cells are perpendicular to the free surface & basement membrane.
- Apical mitoses.
DDx:
- Condyloma acuminatum.
- Vulvar squamous cell carcinoma.
- Extramammary Paget disease.
- Dermatomycosis (fungal infection) - esp. candidiasis.
Images:
- VIN I - koilocytes (nih.gov).[14]
- VIN I (nih.gov).[14]
- VIN III (flickr.com).
- VIN III (WC).
- VIN (brown.edu).
IHC
- Classic VIN: p16 +ve, p53 -ve.
- Differentiated VIN: p16 -ve, p53 +ve.[15]
Note:
- p16 can be thought of as a poor man's HPV test.
Sign out
VIN I
VULVA, BIOPSY: - CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (VIN) I (MILD DYSPLASIA). - NEGATIVE FOR INVASIVE MALIGNANCY.
VIN III
VULVA, EXCISION: - CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (VIN) III (SEVERE DYSPLASIA) WITH FOCAL ULCERATION. - MARGIN FOCALLY POSITIVE FOR VIN III. - NEGATIVE FOR INVASIVE MALIGNANCY.
Differentiated vulvar intraepithelial neoplasia
General
Epidemiology:
- Associated with lichen sclerosus.
- Seen in older women.
Note:
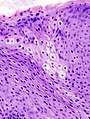
Microscopic
Features:[18]
- Thickening of the stratum spinosum (acanthosis).
- Elongation of rete ridges with bridging/anastomoses between rete ridges.
- Nuclear atypia - esp. basal layer.
- Nuclei in stratum corneum (parakeratosis).
- +/-Atypical mitoses.
Notes:
- Not graded like classic VIN.
- Mnemonic BAD LAP: basal cell atypia, anastomosing rete ridges (bridging), dVIN, lichen sclerosus, acanthosis, parakeratosis.
DDx:
- Lichen sclerosus.
- Lichen simplex chronicus (squamous hyperplasia).
Images
www:
IHC
- Differentiated VIN: p16 -ve, p53 +ve.[15]
- Classic VIN: p16 +ve, p53 -ve.
Note:
- p16 can be thought of as a poor man's HPV test.
Malignant neoplasms of the vulva
Overview
Most common malignancies of vulva:[19]
- Invasive squamous cell carcinoma.
- Malignant melanoma.
Vulvar squamous cell carcinoma
- AKA squamous cell carcinoma of the vulva.
General
- Most common vulvar malignancy.
Precursor lesions for SCC
- Vulvar intraepithelial neoplasia (VIN).
VIN can be divided into:
- Classic VIN, and
- Differentiated VIN.
- Differentiated VIN is mostly irrelevant as it is basically never seen alone, i.e. it usually accompanies cancer.
Low grade pre-cancerous lesions (VIN) are typically HPV positive, while high grade pre-cancerous lesions and cancer are less often HPV positive.[20]
Microscopic
Like SCC elsewhere.
- Microinvasion: <=1 mm stromal invasion, tumour size <=2 cm (T1a).[21]
- Depth from DE junction.
Note:
- Tumour thickness != depth of invasion.
- Thickness = granular layer or surface (no granular layer present) to deepest tumour.
- Depth of invasion = epithelial-stromal junction in "valley" of papillae.
DDx:
- Classic vulvar intraepithelial neoplasia - esp. tangential sections.
- Differentiated vulvar intraepithelial neoplasia.
Sign out
VULVA, LEFT SIDE, (INCISIONAL) BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA. -- PLEASE SEE TUMOUR SUMMARY. TUMOUR SUMMARY - VULVA Specimen Size: multiple fragments - up to 2.5 cm in aggregate. Tumour site: left vulva - around Bartholin's gland. Tumour size: at least 10 mm, cannot be determined due to fragmentation. Tumour focality: cannot be determined. Histologic type: squamous cell carcinoma with focal keratinization. Histologic Grade: G2 - moderately differentiated. Microscopic tumour extension: greater than 2 mm, assessment limited by fragmentation and tissue orientation. Tumour border: infiltrating. Lymph-Vascular Invasion: present. Additional findings: Vulvar intraepithelial neoplasia (VIN) 3 (severe dysplasia/carcinoma in situ).
See also
- Gynecologic pathology.
- Uterus.
- Cervix - cervical intraepithelial neoplasia (CIN).
- Vagina.
- Anus - anal intraepithelial neoplasia.
References
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 280 Q29. ISBN 978-1416025887.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 143. ISBN 978-0443069208.
- ↑ URL: http://emedicine.medscape.com/article/781735-differential. Accessed on: 5 July 2013.
- ↑ Huang, Z.; Yang, S.; Li, Q.; Yan, P.; Li, L. (Feb 2001). "[Evaluation the pathological diagnostic values of koilocyte in condyloma acuminatum].". Zhonghua Liu Xing Bing Xue Za Zhi 22 (1): 58-60. PMID 11860848.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 204. ISBN 978-0781765275.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1230. ISBN 0-7216-0187-1.
- ↑ http://pathologyoutlines.com/vulva.html#bartholincyst
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 456. ISBN 978-0781765275. }}
- ↑ Hidradenoma papilliferum. Stedman's Medical Dictionary. 27th Ed.
- ↑ Pai, K.; Pai, S.; Gupta, A.; Rao, P.; Renjhen, P. (Oct 2006). "Synchronous vulvar intraepithelial neoplasia (VIN) of warty type and cervical intraepithelial neoplasia (CIN): case report.". Indian J Pathol Microbiol 49 (4): 585-7. PMID 17183865.
- ↑ Ait Menguellet, S.; Collinet, P.; Houfflin Debarge, V.; Nayama, M.; Vinatier, D.; Leroy, JL. (May 2007). "Management of multicentric lesions of the lower genital tract.". Eur J Obstet Gynecol Reprod Biol 132 (1): 116-20. doi:10.1016/j.ejogrb.2006.04.011. PMID 16713062.
- ↑ Rufforny, I.; Wilkinson, EJ.; Liu, C.; Zhu, H.; Buteral, M.; Massoll, NA. (Apr 2005). "Human papillomavirus infection and p16(INK4a) protein expression in vulvar intraepithelial neoplasia and invasive squamous cell carcinoma.". J Low Genit Tract Dis 9 (2): 108-13. PMID 15870532.
- ↑ LAE. February 2009.
- ↑ 14.0 14.1 Kotsopoulos, IC.; Tampakoudis, GP.; Evaggelinos, DG.; Nikolaidou, AI.; Fytili, PA.; Kartsiounis, VC.; Gerasimidou, DK. (2011). "Implication of human papillomavirus-66 in vulvar carcinoma: a case report.". J Med Case Rep 5: 232. doi:10.1186/1752-1947-5-232. PMC 3150314. PMID 21702970. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/.
- ↑ 15.0 15.1 15.2 Pinto, AP.; Miron, A.; Yassin, Y.; Monte, N.; Woo, TY.; Mehra, KK.; Medeiros, F.; Crum, CP. (Mar 2010). "Differentiated vulvar intraepithelial neoplasia contains Tp53 mutations and is genetically linked to vulvar squamous cell carcinoma.". Mod Pathol 23 (3): 404-12. doi:10.1038/modpathol.2009.179. PMID 20062014.
- ↑ Ruhul Quddus, M.; Xu, C.; Steinhoff, MM.; Zhang, C.; Lawrence, WD.; Sung, CJ. (Jun 2005). "Simplex (differentiated) type VIN: absence of p16INK4 supports its weak association with HPV and its probable precursor role in non-HPV related vulvar squamous cancers.". Histopathology 46 (6): 718-20. doi:10.1111/j.1365-2559.2005.02036.x. PMID 15910611.
- ↑ Yang, B.; Hart, WR. (Mar 2000). "Vulvar intraepithelial neoplasia of the simplex (differentiated) type: a clinicopathologic study including analysis of HPV and p53 expression.". Am J Surg Pathol 24 (3): 429-41. PMID 10716158.
- ↑ 18.0 18.1 van de Nieuwenhof, HP.; Bulten, J.; Hollema, H.; Dommerholt, RG.; Massuger, LF.; van der Zee, AG.; de Hullu, JA.; van Kempen, LC. (Feb 2011). "Differentiated vulvar intraepithelial neoplasia is often found in lesions, previously diagnosed as lichen sclerosus, which have progressed to vulvar squamous cell carcinoma.". Mod Pathol 24 (2): 297-305. doi:10.1038/modpathol.2010.192. PMID 21057461.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 459. ISBN 978-0781765275.
- ↑ De Vuyst H, Clifford GM, Nascimento MC, Madeleine MM, Franceschi S (April 2009). "Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: a meta-analysis". Int. J. Cancer 124 (7): 1626–36. doi:10.1002/ijc.24116. PMID 19115209.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Vulva_11protocol.pdf. Accessed on: 9 March 2012.