Difference between revisions of "Vermiform appendix"
(→Adenovirus appendicitis: split out) |
|||
| Line 160: | Line 160: | ||
==Mucinous tumours of the appendix== | ==Mucinous tumours of the appendix== | ||
{{ | {{Main|Mucinous tumours of the appendix}} | ||
| | This grouping includes ''mucinous cystadenoma'' and ''mucinous cystadenocarcinoma''. | ||
}} | |||
==Goblet cell carcinoid== | ==Goblet cell carcinoid== | ||
Revision as of 01:16, 4 April 2014
The vermiform appendix, usually just appendix, is a little thingy that is attached to the cecum. Taking it out is the bread 'n butter of general surgery.
The appendix is a vestigial structure that is thought to have arisen from a larger cecum. Larger cecae are often seen in herbivores and thought to facilitate better digestion of plant matter.[1]
Normal
Normal vermiform appendix
General
- Seen in:
- Right hemicolectomies.
- Surgeries for ovarian mucinous tumours.
Gross
- Shiny serosal surface.
- No exudate.
- Normal diameter.
- 6.6 +/- 1.5 mm -- based on CT.[2]
Microscopic
Features:
- +/-Lymphoid hyperplasia - mucosa or submucosa.
- Normal colorectal-type mucosa.
- Fatty submucosa.
- Benign smooth muscle.
- Serosa.
Negatives:
- No neutrophils in the muscularis propria.
- No lesion in appendiceal tip.
- No serosal inflammation (periappendicitis).
- No organisms in the appendiceal lumen, e.g. Enterobius vermicularis.
DDx:
- Adenovirus appendicitis.
- Cryptosporidiosis.
- Mild colitis.
Sign out
VERMIFORM APPENDIX WITHIN NORMAL LIMITS.
Negative appendectomy
General
- Common.
- Use for quality control among general surgeons.[citation needed]
Gross
See normal vermiform appendix.
Microscopic
See normal vermiform appendix.
Notes:
- Should be submitted in total.
DDx:
- Acute appendicitis.
- Adenovirus appendicitis.
- Appendiceal neuroendocrine tumour.
- Non-appendiceal pathology - see DDx of acute appendicitis.
- Isolated periappendicitis.
Sign out
VERMIFORM APPENDIX, APPENDECTOMY: - APPENDIX NEGATIVE FOR ACUTE APPENDICITIS AND NEGATIVE FOR ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX, APPENDECTOMY: - APPENDIX WITH LYMPHOID HYPERPLASIA AND FOCAL MUCOSAL EROSIONS. - NEGATIVE FOR ACUTE APPENDICITIS. - NEGATIVE FOR ACUTE PERIAPPENDICITIS.
Micro
The sections show appendiceal wall with focal mucosa erosions and several intraluminal neutrophil clusters. Lymphoid hyperplasia is present. Fecal material is present within the lumen of the appendix.
There are no neutrophils within the muscularis propria. There is no serositis. There is no distortion of the crypt architecture. No granulomas are identified. No cryptitis is identified.
Inflammatory pathologies
Acute appendicitis
Adenovirus appendicitis
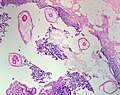
Enterobius vermicularis
- AKA pinworm.
General
- May be found in the appendix.
- The incidence is higher in normal appendices than inflamed ones.[3][4]
- Clinically mimics appendicitis.[5]
Microscopic
Features:
- Usu. the appendiceal wall has no inflammation, i.e. there is no appendicitis.[3][4]
- Enterobius vermicularis organisms.
Image
Granulomatous appendicitis
General
Most common cause:
- Yersinia appendicitis.[6]
DDx:[7]
- Yersinia appendicitis.[6]
- Yersinia = gram negative rod (red on Gram stain).
- "Safety pin"-like appearance[8] - approximately 0.5 micrometers diameter x 2 micrometers length.
- Other micro-organism (TB, fungus).
- Crohn's disease.
- Sarcoidosis.
- Foreign body reaction.
- Interval (delayed) appendectomy.
- Approximately 60% of delayed appendectomies have granulomas.[9]
Microscopic
Features:
- Granulomas.
- +/-"Safety pin"-like organisms (Yersinia).
Image(s):
Inflammatory bowel disease
Periappendicitis
General
Definition: inflammation of tissues around the (vermiform) appendix.[10]
- May be seen in association of appendicitis or alone.
Microscopic
Features:
- Acute inflammation of the serosa.
- Neutrophils in the serosa.
DDx:
Tumours of the appendix
Adenocarcinoma
- Like colorectal adenocarcinoma - see colorectal tumours.
Mucinous tumours of the appendix
This grouping includes mucinous cystadenoma and mucinous cystadenocarcinoma.
Goblet cell carcinoid
Neuroendocrine tumour of the appendix
- Previously known as appendiceal carcinoid.
- AKA appendiceal neuroendocrine tumour, abbreviated appendiceal NET.
General
- Most common tumour of the appendix.[13]
- Not really common though - one is seen in approximately 300 appendectomies.[14]
Size matters in appendiceal NETs:[15]
- <1.0 cm - do not metastasize.
- 1.0-2.0 cm - rarely metastasize.
Gross
- Classically found in the tip of the appendix.
Image:
Microscopic
Features:
- Nests of cells - with fibrous stroma in between.
- May have a trabecular architecture.
- Stippled chromatin AKA salt-and-pepper chromatin, coarse chromatin.
- Classically subepithelial/mural.
DDx:
- Colorectal adenocarcinoma.
- Crypt cell carcinoma (goblet cell carcinoid).
- Metastatic adenocarcinoma.
Images
www:
- Appendiceal carcinoid (humpath.com).
- Carcinoid of the appendix (brown.edu).
- Appendiceal carcinoid (flickr.com/Qiao).
IHC
Features:
- Chromogranin A -ve/+ve.
- Synaptophysin +ve.
See: neuroendocrine tumours.
See also
References
- ↑ Dawkins, R. (2009). The Greatest Show on Earth: The Evidence for Evolution (1st ed.). Free Press. pp. 115. ISBN 978-1416594789.
- ↑ Charoensak, A.; Pongpornsup, S.; Suthikeeree, W. (Dec 2010). "Wall thickness and outer diameter of the normal appendix in adults using 64 slices multidetector CT.". J Med Assoc Thai 93 (12): 1437-42. PMID 21344807.
- ↑ 3.0 3.1 Wiebe, BM. (Mar 1991). "Appendicitis and Enterobius vermicularis.". Scand J Gastroenterol 26 (3): 336-8. PMID 1853157.
- ↑ 4.0 4.1 Dahlstrom, JE.; Macarthur, EB. (Oct 1994). "Enterobius vermicularis: a possible cause of symptoms resembling appendicitis.". Aust N Z J Surg 64 (10): 692-4. PMID 7945067.
- ↑ Ariyarathenam AV, Nachimuthu S, Tang TY, Courtney ED, Harris SA, Harris AM (2010). "Enterobius vermicularis infestation of the appendix and management at the time of laparoscopic appendectomy: case series and literature review". Int J Surg 8 (6): 466–9. doi:10.1016/j.ijsu.2010.06.007. PMID 20637320.
- ↑ 6.0 6.1 Lamps LW, Madhusudhan KT, Greenson JK, et al. (April 2001). "The role of Yersinia enterocolitica and Yersinia pseudotuberculosis in granulomatous appendicitis: a histologic and molecular study". Am. J. Surg. Pathol. 25 (4): 508–15. PMID 11257626.
- ↑ http://granuloma.homestead.com/appendicitis.html
- ↑ URL: http://www.cdc.gov/ncidod/dvbid/plague/p1.htm. Accessed on: 30 June 2011.
- ↑ Guo, G.; Greenson, JK. (Aug 2003). "Histopathology of interval (delayed) appendectomy specimens: strong association with granulomatous and xanthogranulomatous appendicitis.". Am J Surg Pathol 27 (8): 1147-51. PMID 12883248.
- ↑ URL: http://www.medilexicon.com/medicaldictionary.php?t=66889. Accessed on: 1 June 2011.
- ↑ Fink, AS.; Kosakowski, CA.; Hiatt, JR.; Cochran, AJ. (Jun 1990). "Periappendicitis is a significant clinical finding.". Am J Surg 159 (6): 564-8. PMID 2349982.
- ↑ O'Neil, MB.; Moore, DB. (Sep 1977). "Periappendicitis: Clinical reality or pathologic curiosity?". Am J Surg 134 (3): 356-7. PMID 900337.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 435. ISBN 978-1416054542.
- ↑ Mitra, B.; Pal, M.; Paul, B.; Saha, TN.; Maiti, A. (2013). "Goblet cell carcinoid of appendix: A rare case with literature review.". Int J Surg Case Rep 4 (3): 334-7. doi:10.1016/j.ijscr.2013.01.007. PMID 23416502.
- ↑ Modlin, IM.; Lye, KD.; Kidd, M. (Feb 2003). "A 5-decade analysis of 13,715 carcinoid tumors.". Cancer 97 (4): 934-59. doi:10.1002/cncr.11105. PMID 12569593.