Difference between revisions of "Urine cytopathology"
Jump to navigation
Jump to search
(+ASC in urine) |
|||
| (35 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
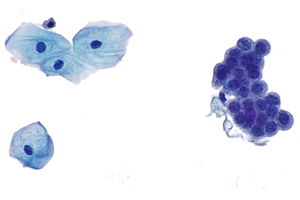
[[Image:Benign urine cytology - 2a -- very high mag.jpg|thumb|right|Urine cytology - squamous cells and urothelial cells. (WC)]] | |||
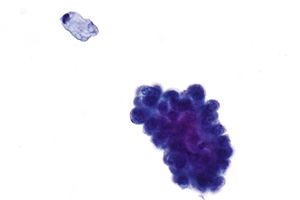
[[Image:Benign urine cytology - 3b -- very high mag.jpg|thumb|right|Urine cytology. (WC)]] | |||
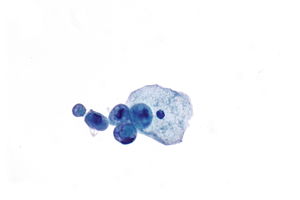
[[Image:Benign urine cytology - 4 -- very high mag.jpg|thumb|right|Urine cytology. (WC)]] | |||
'''Urine cytopathology''' is a large part of cytopathology. | '''Urine cytopathology''' is a large part of cytopathology. | ||
| Line 7: | Line 10: | ||
*Negative for malignancy. | *Negative for malignancy. | ||
*Urothelial carcinoma. | *Urothelial carcinoma. | ||
**AKA ''urothelial cell carcinoma'', abbreviated ''UCC''. | **[[AKA]] ''urothelial cell carcinoma'', abbreviated ''[[UCC]]''. | ||
*Urothelial carcinoma with squamous features. | *Urothelial carcinoma with squamous features. | ||
*Polyomavirus infection. | *Polyomavirus infection. | ||
| Line 25: | Line 28: | ||
*Large (benign) squamous component. | *Large (benign) squamous component. | ||
**Usually contamination from gential tract (in females). | **Usually contamination from gential tract (in females). | ||
===Paris system for urinary cytology=== | |||
This is a reporting standard with the following categories:<ref name=pmid27318895>{{Cite journal | last1 = Barkan | first1 = GA. | last2 = Wojcik | first2 = EM. | last3 = Nayar | first3 = R. | last4 = Savic-Prince | first4 = S. | last5 = Quek | first5 = ML. | last6 = Kurtycz | first6 = DF. | last7 = Rosenthal | first7 = DL. | title = The Paris System for Reporting Urinary Cytology: The Quest to Develop a Standardized Terminology. | journal = Acta Cytol | volume = 60 | issue = 3 | pages = 185-97 | month = | year = 2016 | doi = 10.1159/000446270 | PMID = 27318895 }}</ref> | |||
#Nondiagnostic/unsatisfactory | |||
#Negative for [[urothelial carcinoma|high-grade urothelial carcinoma]] | |||
#Atypical urothelial cells | |||
#Suspicious for high-grade urothelial carcinoma | |||
#High-grade urothelial carcinoma | |||
#Low-grade urothelial neoplasm | |||
#Other malignancy (includes both primary and secondary) and miscellaneous lesions | |||
==Normal== | ==Normal== | ||
| Line 30: | Line 43: | ||
*Benign cells are often in small clumps. | *Benign cells are often in small clumps. | ||
=== | ===Major cell types=== | ||
Practical cell typing:<ref>SM. 7 January 2010.</ref> | Practical cell typing:<ref>SM. 7 January 2010.</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 46: | Line 59: | ||
| Irregular/jagged | | Irregular/jagged | ||
|} | |} | ||
====Images==== | |||
=====Case 1===== | |||
<gallery> | |||
Image: Benign urine cytology - 4 -- very high mag.jpg | Benign - c/w renal tubular cells - very high mag. (WC) | |||
Image: Benign urine cytology - 4 - alt -- very high mag.jpg | Benign - c/w renal tubular cells - very high mag. (WC) | |||
</gallery> | |||
=====Case 2===== | |||
<gallery> | |||
Image: Benign urine cytology - 1 -- very high mag.jpg | BUC - very high mag. (WC) | |||
Image: Benign urine cytology - 1a -- very high mag.jpg | BUC - very high mag. (WC) | |||
Image: Benign urine cytology - 1b -- very high mag.jpg | BUC - very high mag. (WC) | |||
</gallery> | |||
=====Case 3===== | |||
<gallery> | |||
Image: Benign urine cytology - 3 -- high mag.jpg | BUC - high mag. (WC) | |||
Image: Benign urine cytology - 3a -- very high mag.jpg | BUC - very high mag. (WC) | |||
Image: Benign urine cytology - 3b -- very high mag.jpg | BUC - very high mag. (WC) | |||
</gallery> | |||
=====Case 4===== | |||
<gallery> | |||
Image: Benign urine cytology - 2 -- high mag.jpg | BUC - high mag. | |||
Image: Benign urine cytology - 2a -- very high mag.jpg | BUC - very high mag. | |||
Image: Benign urine cytology - 2x -- very high mag.jpg | BUC - very high mag. | |||
Image: Benign urine cytology - 2i -- very high mag.jpg | BUC - very high mag. | |||
</gallery> | |||
===Degenerative cells=== | ===Degenerative cells=== | ||
| Line 57: | Line 98: | ||
*Vacuolated cytoplasm - "moth-eaten" appearance. | *Vacuolated cytoplasm - "moth-eaten" appearance. | ||
**Normal urothelial cytoplasm is dense and has no vacuoles. | **Normal urothelial cytoplasm is dense and has no vacuoles. | ||
===Urine crystals=== | |||
{{Main|Urine crystals}} | |||
==Tabular DDx== | ==Tabular DDx== | ||
| Line 196: | Line 240: | ||
*Both have eccentric nuclei. | *Both have eccentric nuclei. | ||
==Human | ==Human polyomavirus infection== | ||
{{Main|Polyomavirus nephropathy}} | {{Main|Polyomavirus nephropathy}} | ||
===General=== | ===General=== | ||
| Line 202: | Line 246: | ||
*Associated with immunosuppression/immunodeficiency. | *Associated with immunosuppression/immunodeficiency. | ||
*BK virus related to JC virus. | *BK virus related to JC virus. | ||
*BK virus associated with [[urothelial carcinoma]].<ref name=pmid24879380>{{Cite journal | last1 = Tsai | first1 = HL. | last2 = Chang | first2 = JW. | last3 = Wu | first3 = TH. | last4 = King | first4 = KL. | last5 = Yang | first5 = LY. | last6 = Chan | first6 = YJ. | last7 = Yang | first7 = AH. | last8 = Chang | first8 = FP. | last9 = Pan | first9 = CC. | title = Outcomes of kidney transplant tourism and risk factors for de novo urothelial carcinoma. | journal = Transplantation | volume = 98 | issue = 1 | pages = 79-87 | month = Jul | year = 2014 | doi = 10.1097/TP.0000000000000023 | PMID = 24879380 }}</ref><ref name=pmid24103071>{{Cite journal | last1 = Li | first1 = JY. | last2 = Fang | first2 = D. | last3 = Yong | first3 = TY. | last4 = Klebe | first4 = S. | last5 = Juneja | first5 = R. | last6 = Gleadle | first6 = JM. | title = Transitional cell carcinoma in a renal allograft with BK nephropathy. | journal = Transpl Infect Dis | volume = 15 | issue = 6 | pages = E270-2 | month = Dec | year = 2013 | doi = 10.1111/tid.12142 | PMID = 24103071 }}</ref> | |||
DDx: | DDx: | ||
*Urothelial carcinoma. | *[[Urothelial carcinoma]]. | ||
**May exist together with urothelial carcinoma ~ nuclei 2-4x the size of not infected malignant cells.<ref name=pmid20891007>{{Cite journal | last1 = Loghavi | first1 = S. | last2 = Bose | first2 = S. | title = Polyomavirus infection and urothelial carcinoma. | journal = Diagn Cytopathol | volume = 39 | issue = 7 | pages = 531-5 | month = Jul | year = 2011 | doi = 10.1002/dc.21490 | PMID = 20891007 }}</ref> | |||
===Cytology=== | ===Cytology=== | ||
| Line 221: | Line 267: | ||
*Normal urothelial cell nucleus ~ 1.5X the size of a lymphocyte. | *Normal urothelial cell nucleus ~ 1.5X the size of a lymphocyte. | ||
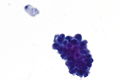
====Image==== | |||
<gallery> | |||
Image:Polyomavirus_2.jpg | Polyomavirus. (WC) | |||
</gallery> | |||
===IHC=== | ===IHC=== | ||
| Line 233: | Line 280: | ||
==Urothelial cell carcinoma== | ==Urothelial cell carcinoma== | ||
{{Main|Urothelial cell carcinoma}} | |||
*Abbreviated ''UCC''. | |||
===General=== | ===General=== | ||
*Very hard/impossible to diagnose low-grade UCC on cytology. | |||
*Very hard/impossible to | |||
**The diagnosis of low-grade UCC is based on architecture (papillae). | **The diagnosis of low-grade UCC is based on architecture (papillae). | ||
===Cytology=== | ===Cytology=== | ||
Features:<ref>{{Ref APBR|682}}</ref> | Features:<ref>{{Ref APBR|682}}</ref> | ||
#Hyperchromasia - '''low power''' feature. | #Hyperchromasia - '''low power''' feature. | ||
#Irregular nuclear membrane - '''key feature'''. | #Irregular nuclear membrane - '''key feature'''. | ||
#Increased NC ratio. | #Increased NC ratio. | ||
#*Often uniform - when comparing malignant cells. | #*Often uniform - when comparing malignant cells. | ||
#"Large nuclei" (3-4X the size of a normal urothelial cell) - '''low power''' feature. | |||
#*These are not required for the diagnosis.<ref>SM. 12 January 2010.</ref> | |||
#*Large nuclei may be seen in benign umbrella cell, where the [[NC ratio]] is normal. | |||
#Nuclear size variation, >=2X other malign. looking cells - very useful. | #Nuclear size variation, >=2X other malign. looking cells - very useful. | ||
#+/-Large irregular nucleoli - common. | #+/-Large irregular nucleoli - common. | ||
Minimal criteria: | Minimal criteria: | ||
*Criteria # | *Criteria #1-3. † | ||
Notes: | Notes: | ||
| Line 262: | Line 310: | ||
*Degeneration. | *Degeneration. | ||
*Polyomavirus. | *Polyomavirus. | ||
† Willner ''et al.'' require all of the following:<ref name=pmid33088909>{{cite journal |authors=Willner J, Matloob A, Colanta A, Khader SN |title=Educational Case: Urothelial Carcinoma: An Overview of Pathologic Diagnosis |journal=Acad Pathol |volume=7 |issue= |pages=2374289520958172 |date=2020 |pmid=33088909 |doi=10.1177/2374289520958172 |url=}}</ref> | |||
#Nucleus-to-cytoplasm ratio >0.7. | |||
#Hyperchromasia (moderate or severe). | |||
#Irregular nuclear membranes, marked. | |||
#Coarse chromatin. | |||
Willner's criteria can be remember by ''CHIN'' = '''''c'''oarse chromatin, '''h'''yperchromasia, '''i'''rregular nuclear membrane, '''N'''C ratio increased''. | |||
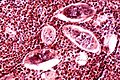
==Schistosoma== | ==Schistosoma== | ||
| Line 271: | Line 327: | ||
*S. haematobium has a "spike" approx. the size of a PMN. | *S. haematobium has a "spike" approx. the size of a PMN. | ||
Image | ====Image==== | ||
<gallery> | |||
Image:Schistosomiasis_haematobia.jpg| Schistosoma haematobium. (WC) | |||
</gallery> | |||
==Trichomonas== | |||
{{Main|Gynecologic_cytopathology#Trichomoniasis}} | |||
*Trichomonas is found in approximately 0.1% of urine cytology specimens.<ref>{{cite journal |authors=Doxtader EE, Elsheikh TM |title=Diagnosis of trichomoniasis in men by urine cytology |journal=Cancer Cytopathol |volume=125 |issue=1 |pages=55–59 |date=January 2017 |pmid=27636204 |doi=10.1002/cncy.21778 |url=}}</ref> | |||
==Atypical squamous cells in urine== | |||
*Atypical squamous cells in urine cytology specimens are rare ~ 0.3%.<ref>{{cite journal |authors=Velez Torres JM, Zhao J, Epstein JI, Kryvenko ON |title=Condyloma acuminatum of the urinary tract demonstrates atypical squamous cells in urine cytology |journal=Hum Pathol |volume=130 |issue= |pages=110–116 |date=December 2022 |pmid=36244465 |doi=10.1016/j.humpath.2022.10.006 |url=}}</ref> | |||
*An older series describes an association with SCC/UCC of the bladder and SCC of the cervix.<ref>{{cite journal |authors=Owens CL, Ali SZ |title=Atypical squamous cells in exfoliative urinary cytology: clinicopathologic correlates |journal=Diagn Cytopathol |volume=33 |issue=6 |pages=394–8 |date=December 2005 |pmid=16299739 |doi=10.1002/dc.20344 |url=}}</ref> | |||
<pre> | |||
Atypical squamous cells present, see comment. | |||
Benign urothelial cells present in background. | |||
Negative for High-Grade Urothelial Carcinoma. | |||
Comment: | |||
Due to the atypical squamous cells, consideration of further work-up is suggested within the clinical context, based on reported associations.[1] | |||
1. Diagn Cytopathol. 2005 Dec;33(6):394-8. doi: 10.1002/dc.20344 - https://pubmed.ncbi.nlm.nih.gov/16299739/ | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Cytopathology]]. | *[[Cytopathology]]. | ||
| Line 282: | Line 358: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
==External links== | |||
*[http://www.cytologystuff.com/study/nongynintro3.htm Urine cytology (cytologystuff.com)]. | |||
[[Category:Cytopathology]] | [[Category:Cytopathology]] | ||
Latest revision as of 22:45, 30 January 2024
Urine cytopathology is a large part of cytopathology.
This article deals only with urine cytopathology. An introduction to cytopathology is in the cytopathology article.
DDx
Common
- Negative for malignancy.
- Urothelial carcinoma.
- Urothelial carcinoma with squamous features.
- Polyomavirus infection.
- Acute inflammation.
- Chronic inflammation.
Rare
Usually not reported
- Candida.
- Quite common.
- Large (benign) squamous component.
- Usually contamination from gential tract (in females).
Paris system for urinary cytology
This is a reporting standard with the following categories:[1]
- Nondiagnostic/unsatisfactory
- Negative for high-grade urothelial carcinoma
- Atypical urothelial cells
- Suspicious for high-grade urothelial carcinoma
- High-grade urothelial carcinoma
- Low-grade urothelial neoplasm
- Other malignancy (includes both primary and secondary) and miscellaneous lesions
Normal
General
- Benign cells are often in small clumps.
Major cell types
Practical cell typing:[2]
| Nucleus | Cell border | |
|---|---|---|
| Urothelium | Larger | Smooth/elliptical |
| Squamous epithelium | Smaller | Irregular/jagged |
Images
Case 1
Case 2
Case 3
Case 4
Degenerative cells
Features:
- Nucleus protrudes through cell membrane.
- Chromatin degeration:
- "Cobweb" appearance - white holes/pale staining.
- White holes/frayed appearance.
- Small clumps of chromatin at the edge of nuclear membrane.
- Frayed cell membrane/irregular cell membrane.
- Vacuolated cytoplasm - "moth-eaten" appearance.
- Normal urothelial cytoplasm is dense and has no vacuoles.
Urine crystals
Main article: Urine crystals
Tabular DDx
Urothelial carcinoma versus benign urothelium
| Urothelial carcinoma | Benign urothelium | Use of feature | Utility | |
|---|---|---|---|---|
| Nuclear hyperchromasia | Present | Absent | r/i & r/o UC | Strong |
| Nuclear-to-cytoplasmic (NC) ratio | ~1:1.2 | ~1:2 | r/i & r/o UC; 1:>=2 suggests benign | Strong |
| Nuclear membrane irregularity (NMI) | +/- | Absent | r/i UC; presence strong predictor of malignancy (absence of NMI of little value) | Moderate |
| Cytoplasm | Green/grey | Green or grey & granular | r/o UC; granular (suggests degeneration) | Moderate |
| Coarse chromatin (CC) | Present | +/- | r/o UC; absence of CC suggest benign | Moderate |
| Nucleoli | In scattered cells | +/- in reactive | Not useful | Nil for diagnosing UC |
| Nuclear size | >2.5X normal | Usu. <=2X normal | Alone not much value, many large cells benign, many small cells malignant | Limited value, NC ratio much better measure |
Degeneration versus UC[3]
| Urothelial carcinoma | Degeneration | |
|---|---|---|
| Architecture | Usually single cells | Often small clusters |
| Cell borders | Sharp | Fuzzy/frayed |
| Cytoplasm | Green, solid | Grey, lacy/moth eaten |
| Nuclear membrane | Irregular | Usually regular |
| Chromatin | Granular/coarse | Granular/coarse |
Polyomavirus versus urothelial carcinoma
| Urothelial carcinoma | Polyoma virus | |
|---|---|---|
| Architecture | Often single cells | Single cells |
| Nucleus size | Often 3-4X normal urothelial cell | 2X normal urothelial cell nucleus (should not be larger) |
| Chromatin | Clumped or "dancing" | Ground glass inclusions/smudged |
| Nuclear membrane | Usually irregular | Regular |
Urothelial carcinoma vs adenocarcinoma
The default diagnosis is urothelial carcinoma as this is the most likely if there is no prior history of malignancy.
| Urothelial carcinoma | Adenocarcinoma | |
|---|---|---|
| Vacuoles | None | Present - mucin filled |
| Cytoplasm | Dense appearing | Fluffy |
| Chromatin | Coarse - clumped or "dancing" | Fine |
| History | None | History of adenocarcinoma |
| Nucleoli | Often present, multiple | Usually only one - every tumour cell |
Notes:
- Both have eccentric nuclei.
Human polyomavirus infection
Main article: Polyomavirus nephropathy
General
- Caused by Human polyomavirus, AKA BK virus.[4]
- Associated with immunosuppression/immunodeficiency.
- BK virus related to JC virus.
- BK virus associated with urothelial carcinoma.[5][6]
DDx:
- Urothelial carcinoma.
- May exist together with urothelial carcinoma ~ nuclei 2-4x the size of not infected malignant cells.[7]
Cytology
- "Decoy cells":
- Usually 2x the size of a normal urothelial cell nucleus.
- Single cells - important feature.
- Scant "degenerative-appearing" cytoplasm.
- High NC ratio.
- Intranuclear inclusions - key feature.
- Central smudging (or "wash-out") of the chromatin/"Ground glass" chromatin.
- Surrounded by clear halo just deep to the nuclear membrane.
- Nuclear membrane clumping.
Notes:
- Normal urothelial cell nucleus ~ 1.5X the size of a lymphocyte.
Image
IHC
- JC/BK virus.[10]
"Inflammation" in urine specimens
- One should resist the temptation to call "inflammation" in urine specimens, as processing concentrates the WBCs.
- If the quantity of WBCs is truly "excessive"... then it ought to be called.
Urothelial cell carcinoma
Main article: Urothelial cell carcinoma
- Abbreviated UCC.
General
- Very hard/impossible to diagnose low-grade UCC on cytology.
- The diagnosis of low-grade UCC is based on architecture (papillae).
Cytology
Features:[11]
- Hyperchromasia - low power feature.
- Irregular nuclear membrane - key feature.
- Increased NC ratio.
- Often uniform - when comparing malignant cells.
- "Large nuclei" (3-4X the size of a normal urothelial cell) - low power feature.
- Nuclear size variation, >=2X other malign. looking cells - very useful.
- +/-Large irregular nucleoli - common.
Minimal criteria:
- Criteria #1-3. †
Notes:
- Coarse chromatin may be benign.
- Fine/non-granular chromatin suggests benign.
- One does not usually call squamous cell carcinoma on cytology.
- If features of squamous differentiation are present one calls urothelial carcinoma with squamous features.
DDx:
- Degeneration.
- Polyomavirus.
† Willner et al. require all of the following:[13]
- Nucleus-to-cytoplasm ratio >0.7.
- Hyperchromasia (moderate or severe).
- Irregular nuclear membranes, marked.
- Coarse chromatin.
Willner's criteria can be remember by CHIN = coarse chromatin, hyperchromasia, irregular nuclear membrane, NC ratio increased.
Schistosoma
- Associated with squamous cell carcinoma of the bladder.
Histology
Features of ova:
- Elliptical ~80 micrometres max dimension.
- S. haematobium has a "spike" approx. the size of a PMN.
Image
Trichomonas
Main article: Gynecologic_cytopathology#Trichomoniasis
- Trichomonas is found in approximately 0.1% of urine cytology specimens.[14]
Atypical squamous cells in urine
- Atypical squamous cells in urine cytology specimens are rare ~ 0.3%.[15]
- An older series describes an association with SCC/UCC of the bladder and SCC of the cervix.[16]
Atypical squamous cells present, see comment. Benign urothelial cells present in background. Negative for High-Grade Urothelial Carcinoma. Comment: Due to the atypical squamous cells, consideration of further work-up is suggested within the clinical context, based on reported associations.[1] 1. Diagn Cytopathol. 2005 Dec;33(6):394-8. doi: 10.1002/dc.20344 - https://pubmed.ncbi.nlm.nih.gov/16299739/
See also
References
- ↑ Barkan, GA.; Wojcik, EM.; Nayar, R.; Savic-Prince, S.; Quek, ML.; Kurtycz, DF.; Rosenthal, DL. (2016). "The Paris System for Reporting Urinary Cytology: The Quest to Develop a Standardized Terminology.". Acta Cytol 60 (3): 185-97. doi:10.1159/000446270. PMID 27318895.
- ↑ SM. 7 January 2010.
- ↑ Adapted from GS. 2 February 2010.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q26). ISBN 978-1416025887.
- ↑ Tsai, HL.; Chang, JW.; Wu, TH.; King, KL.; Yang, LY.; Chan, YJ.; Yang, AH.; Chang, FP. et al. (Jul 2014). "Outcomes of kidney transplant tourism and risk factors for de novo urothelial carcinoma.". Transplantation 98 (1): 79-87. doi:10.1097/TP.0000000000000023. PMID 24879380.
- ↑ Li, JY.; Fang, D.; Yong, TY.; Klebe, S.; Juneja, R.; Gleadle, JM. (Dec 2013). "Transitional cell carcinoma in a renal allograft with BK nephropathy.". Transpl Infect Dis 15 (6): E270-2. doi:10.1111/tid.12142. PMID 24103071.
- ↑ Loghavi, S.; Bose, S. (Jul 2011). "Polyomavirus infection and urothelial carcinoma.". Diagn Cytopathol 39 (7): 531-5. doi:10.1002/dc.21490. PMID 20891007.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681-2 (Q26). ISBN 978-1416025887.
- ↑ SB. 27 January 2010.
- ↑ http://www.acta-cytol.com/toc/auto_abstract.php?id=22895
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.
- ↑ SM. 12 January 2010.
- ↑ Willner J, Matloob A, Colanta A, Khader SN (2020). "Educational Case: Urothelial Carcinoma: An Overview of Pathologic Diagnosis". Acad Pathol 7: 2374289520958172. doi:10.1177/2374289520958172. PMID 33088909.
- ↑ Doxtader EE, Elsheikh TM (January 2017). "Diagnosis of trichomoniasis in men by urine cytology". Cancer Cytopathol 125 (1): 55–59. doi:10.1002/cncy.21778. PMID 27636204.
- ↑ Velez Torres JM, Zhao J, Epstein JI, Kryvenko ON (December 2022). "Condyloma acuminatum of the urinary tract demonstrates atypical squamous cells in urine cytology". Hum Pathol 130: 110–116. doi:10.1016/j.humpath.2022.10.006. PMID 36244465.
- ↑ Owens CL, Ali SZ (December 2005). "Atypical squamous cells in exfoliative urinary cytology: clinicopathologic correlates". Diagn Cytopathol 33 (6): 394–8. doi:10.1002/dc.20344. PMID 16299739.