Difference between revisions of "Renal transplant pathology"
Jump to navigation
Jump to search
(create - split-out from medical kidney diseases) |
(→Polyomavirus nephropathy: split out) |
||
| (32 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Renal transplant pathology''' is grouped with the ''[[medical kidney diseases]]'', as this | '''Renal transplant pathology''', also '''kidney tranplant pathology''', is grouped with the ''[[medical kidney diseases]]'', as this usually precedes the transplant. Also, many renal transplants have recurrence of the pathology that lead to renal failure. | ||
=Rejection | =Rejection= | ||
There is a consensus on categories - known as "Banff 97". | |||
== | ==Overview== | ||
* | Allograft biopsy categories (Banff 97):<ref name=Ref_DARP400>{{Ref DARP|400}}</ref> | ||
*Mean graft survival is ~4 years for C4d+ interstitial capillaries vs. ~8 years for C4d- renal grafts.<ref name=pmid11135088>Impact of humoral alloreactivity early after transplantation on the long-term survival of renal allografts. Lederer SR, Kluth-Pepper B, Schneeberger H, Albert E, Land W, Feucht HE. Kidney Int. 2001 Jan;59(1):334-41. PMID 11135088.</ref> | {| class="wikitable" | ||
! Type | |||
! Key morphologic finding | |||
|- | |||
| Normal | |||
| no inflammation | |||
|- | |||
| Suspicious for acute rejection | |||
| focal mild tubulitis (1-4 mononuclear cells/tubular cross section) | |||
|- | |||
| Acute/active rejection | |||
| tubulitis (>4 mononuclear cells/tubular cross section); see separate table for grading | |||
|- | |||
| Chronic/sclerosing allograft nephropathy | |||
| interstitial fibrosis and tubular atrophy; see separate table for grading | |||
|} | |||
===Acute/active rejection=== | |||
Acute/active rejection in allograft biopsies (Banff 97):<ref name=Ref_DARP400>{{Ref DARP|400}}</ref> | |||
{| class="wikitable" | |||
! Grade | |||
! Key morphologic finding | |||
|- | |||
| IA | |||
| 4< mononuclear cell/tubular cross section ''or'' 10 tubular cells <10; >25% of parenchyma | |||
|- | |||
| IB | |||
| >10 mononuclear cell/tubular cross section ''or'' 10 tubular cells; >25% of parenchyma | |||
|- | |||
| IIA | |||
| mild-to-moderate intimal arteritis; <=25% of luminal area | |||
|- | |||
| IIB | |||
| severe intimal arteritis; >25% of luminal area | |||
|- | |||
| III | |||
| transmural arteritis and/or [[fibrinoid necrosis]] | |||
|} | |||
===Chronic/sclerosing allograft nephropathy=== | |||
Chronic rejection (Banff 97):<ref name=Ref_DARP400>{{Ref DARP|400}}</ref> | |||
{| class="wikitable" | |||
! Grade | |||
! Key morphologic finding | |||
|- | |||
| Grade 1 | |||
| mild interstitial fibrosis and tubular atrophy | |||
|- | |||
| Grade 2 | |||
| moderate interstitial fibrosis and tubular atrophy | |||
|- | |||
| Grade 3 | |||
| severe interstitial fibrosis and tubular atrophy | |||
|} | |||
==C4d staining== | |||
===General=== | |||
*Acute rejection associated with C4d staining.<ref name=pmid1747954>Vascular deposition of complement-split products in kidney allografts with cell-mediated rejection. Feucht HE, Felber E, Gokel MJ, Hillebrand G, Nattermann U, Brockmeyer C, Held E, Riethmüller G, Land W, Albert E. Clin Exp Immunol. 1991 Dec;86(3):464-70. PMID 1747954.</ref> | |||
*Mean graft survival is ~4 years for C4d +ve interstitial capillaries vs. ~8 years for C4d -ve renal grafts.<ref name=pmid11135088>Impact of humoral alloreactivity early after transplantation on the long-term survival of renal allografts. Lederer SR, Kluth-Pepper B, Schneeberger H, Albert E, Land W, Feucht HE. Kidney Int. 2001 Jan;59(1):334-41. PMID 11135088.</ref> | |||
===Microscopic=== | |||
Features:<ref>URL: [http://www.humpath.com/spip.php?article14451 http://www.humpath.com/spip.php?article14451]. Accessed on: 22 November 2011.</ref> | |||
*Diffuse cytoplasmic C4d staining of the peritubular capillaries. | |||
Image: | |||
*[http://www.humpath.com/spip.php?article14451 Positive C4d staining (humpath.com)]. | |||
==Acute rejection== | ==Acute rejection== | ||
| Line 21: | Line 82: | ||
=Infection= | =Infection= | ||
==Polyomavirus== | ==Polyomavirus nephropathy== | ||
:See also: ''[[Urine_cytopathology#Human_polyomavirus_infection]]'' and ''[[Polyomavirus]]''. | |||
{{Main|Polyomavirus nephropathy}} | |||
=Transplant-related pathology= | =Transplant-related pathology= | ||
==Transplant glomerulopathy== | ==Transplant glomerulopathy== | ||
Microscopic: | *Abbreviated ''TG''. | ||
===General=== | |||
*Pathology that arises in the glomeruli of transplanted kidneys. | |||
*Considered to be a form of ''chronic antibody-mediated rejection''.<ref name=pmid21960169>{{Cite journal | last1 = Haas | first1 = M. | title = Transplant glomerulopathy: it's not always about chronic rejection. | journal = Kidney Int | volume = 80 | issue = 8 | pages = 801-3 | month = Oct | year = 2011 | doi = 10.1038/ki.2011.192 | PMID = 21960169 }}</ref> | |||
===Microscopic=== | |||
Features:<ref name=Ref_DARP411>{{Ref DARP|411}}</ref> | |||
*Irregular GBM thickening - '''key feature'''. | |||
*Tram-tracking of basement membrane. | *Tram-tracking of basement membrane. | ||
*Increased mesangial matrix. | |||
*Segmental and global glomerular sclerosis. | |||
DDx (tram-tracking): | DDx (tram-tracking):<ref name=pmid21960169/> | ||
*[[MPGN]]. | *[[MPGN]] (hepatitis C). | ||
*[[Thrombotic microangiopathy]] (TMA). | *[[Thrombotic microangiopathy]] (TMA). | ||
====Images==== | |||
<gallery> | |||
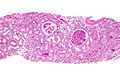
Image:Transplant_glomerulopathy_-_intermed_mag.jpg | Transplant glomerulopathy - intermed. mag. (WC/Nephron) | |||
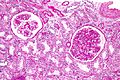
Image:Transplant_glomerulopathy_-_high_mag.jpg | Transplant glomerulopathy - high mag. (WC/Nephron) | |||
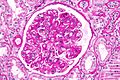
Image:Transplant_glomerulopathy_-_very_high_mag.jpg | Transplant glomerulopathy - very high mag. (WC/Nephron) | |||
</gallery> | |||
==Chronic allograft nephropathy== | |||
*Abbreviated ''CAN''. | |||
*[[AKA]] ''chronic/sclerosing allograft nephropathy''. | |||
===General=== | |||
*Month-years post-transplant. | |||
*Gradual decline in graft function - typically with hypertension and hematuria.<ref name=pmid15954891>{{Cite journal | last1 = Joosten | first1 = SA. | last2 = Sijpkens | first2 = YW. | last3 = van Kooten | first3 = C. | last4 = Paul | first4 = LC. | title = Chronic renal allograft rejection: pathophysiologic considerations. | journal = Kidney Int | volume = 68 | issue = 1 | pages = 1-13 | month = Jul | year = 2005 | doi = 10.1111/j.1523-1755.2005.00376.x | PMID = 15954891 }} | |||
</ref> | |||
*Leading cause of chronic graft failure.<ref name=pmid10469349>{{Cite journal | last1 = Paul | first1 = LC. | title = Chronic allograft nephropathy: An update. | journal = Kidney Int | volume = 56 | issue = 3 | pages = 783-93 | month = Sep | year = 1999 | doi = 10.1046/j.1523-1755.1999.00611.x | PMID = 10469349 }}</ref> | |||
===Microscopic=== | |||
Features:<ref name=Ref_DARP411>{{Ref DARP|411}}</ref> | |||
*Arterial & arteriolar luminal narrowing - '''key feature'''. | |||
**Due to intimal and medial thickening. | |||
*Interstitial fibrosis and renal tubular atrophy. | |||
===Images=== | |||
<gallery> | |||
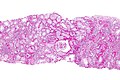
Image:Chronic_allograft_nephropathy_-_intermed_mag.jpg | CAN - intermed. mag. (WC/Nephron) | |||
</gallery> | |||
==Calcineurin-inhibitor toxicity== | ==Calcineurin-inhibitor toxicity== | ||
*Calcineurin-inhibitors (e.g. cyclosporine,<ref name=pmid10354295>{{cite journal |author=Zarifian A, Meleg-Smith S, O'donovan R, Tesi RJ, Batuman V |title=Cyclosporine-associated thrombotic microangiopathy in renal allografts |journal=Kidney Int. |volume=55 |issue=6 |pages=2457–66 |year=1999 |month=June |pmid=10354295 |doi=10.1046/j.1523-1755.1999.00492.x |url=}}</ref> | ===General=== | ||
*Calcineurin-inhibitors (e.g. cyclosporine,<ref name=pmid10354295>{{cite journal |author=Zarifian A, Meleg-Smith S, O'donovan R, Tesi RJ, Batuman V |title=Cyclosporine-associated thrombotic microangiopathy in renal allografts |journal=Kidney Int. |volume=55 |issue=6 |pages=2457–66 |year=1999 |month=June |pmid=10354295 |doi=10.1046/j.1523-1755.1999.00492.x |url=}}</ref> tacrolimus<ref name=Ref_FoRP203>{{Ref FoRP|203}}</ref>) toxicity can induce a [[thrombotic microangiopathy]]. | |||
===Microscopic=== | |||
Features: | |||
*Hyaline arteriopathy with a peripheral and nodular distribution (chronic toxicity). | *Hyaline arteriopathy with a peripheral and nodular distribution (chronic toxicity). | ||
*+/-Thrombotic microangiopathy - see ''[[Thrombotic_microangiopathy#Microscopic|microscopic for TMA]]''. | |||
=See also= | =See also= | ||
*[[Medical kidney diseases]]. | *[[Medical kidney diseases]]. | ||
*[[Kidney]]. | *[[Kidney]]. | ||
*[[Lung transplant pathology]]. | |||
*[[Heart transplant pathology]]. | |||
=References= | =References= | ||
Latest revision as of 17:17, 29 June 2016
Renal transplant pathology, also kidney tranplant pathology, is grouped with the medical kidney diseases, as this usually precedes the transplant. Also, many renal transplants have recurrence of the pathology that lead to renal failure.
Rejection
There is a consensus on categories - known as "Banff 97".
Overview
Allograft biopsy categories (Banff 97):[1]
| Type | Key morphologic finding |
|---|---|
| Normal | no inflammation |
| Suspicious for acute rejection | focal mild tubulitis (1-4 mononuclear cells/tubular cross section) |
| Acute/active rejection | tubulitis (>4 mononuclear cells/tubular cross section); see separate table for grading |
| Chronic/sclerosing allograft nephropathy | interstitial fibrosis and tubular atrophy; see separate table for grading |
Acute/active rejection
Acute/active rejection in allograft biopsies (Banff 97):[1]
| Grade | Key morphologic finding |
|---|---|
| IA | 4< mononuclear cell/tubular cross section or 10 tubular cells <10; >25% of parenchyma |
| IB | >10 mononuclear cell/tubular cross section or 10 tubular cells; >25% of parenchyma |
| IIA | mild-to-moderate intimal arteritis; <=25% of luminal area |
| IIB | severe intimal arteritis; >25% of luminal area |
| III | transmural arteritis and/or fibrinoid necrosis |
Chronic/sclerosing allograft nephropathy
Chronic rejection (Banff 97):[1]
| Grade | Key morphologic finding |
|---|---|
| Grade 1 | mild interstitial fibrosis and tubular atrophy |
| Grade 2 | moderate interstitial fibrosis and tubular atrophy |
| Grade 3 | severe interstitial fibrosis and tubular atrophy |
C4d staining
General
- Acute rejection associated with C4d staining.[2]
- Mean graft survival is ~4 years for C4d +ve interstitial capillaries vs. ~8 years for C4d -ve renal grafts.[3]
Microscopic
Features:[4]
- Diffuse cytoplasmic C4d staining of the peritubular capillaries.
Image:
Acute rejection
- Acute rejection has a standardized classification Banff classification.[5]
Diagnosis of acute rejection requires:
- Serology.
- IHC (C4d).
- This is somewhat debated.
- Morphology.
Infection
Polyomavirus nephropathy
- See also: Urine_cytopathology#Human_polyomavirus_infection and Polyomavirus.
Main article: Polyomavirus nephropathy
Transplant glomerulopathy
- Abbreviated TG.
General
- Pathology that arises in the glomeruli of transplanted kidneys.
- Considered to be a form of chronic antibody-mediated rejection.[6]
Microscopic
Features:[7]
- Irregular GBM thickening - key feature.
- Tram-tracking of basement membrane.
- Increased mesangial matrix.
- Segmental and global glomerular sclerosis.
DDx (tram-tracking):[6]
- MPGN (hepatitis C).
- Thrombotic microangiopathy (TMA).
Images
Chronic allograft nephropathy
- Abbreviated CAN.
- AKA chronic/sclerosing allograft nephropathy.
General
- Month-years post-transplant.
- Gradual decline in graft function - typically with hypertension and hematuria.[8]
- Leading cause of chronic graft failure.[9]
Microscopic
Features:[7]
- Arterial & arteriolar luminal narrowing - key feature.
- Due to intimal and medial thickening.
- Interstitial fibrosis and renal tubular atrophy.
Images
Calcineurin-inhibitor toxicity
General
- Calcineurin-inhibitors (e.g. cyclosporine,[10] tacrolimus[11]) toxicity can induce a thrombotic microangiopathy.
Microscopic
Features:
- Hyaline arteriopathy with a peripheral and nodular distribution (chronic toxicity).
- +/-Thrombotic microangiopathy - see microscopic for TMA.
See also
References
- ↑ 1.0 1.1 1.2 Fogo, Agnes B.; Kashgarian, Michael (2005). Diagnostic Atlas of Renal Pathology: A Companion to Brenner and Rector's The Kidney 7E (1st ed.). Saunders. pp. 400. ISBN 978-1416028710.
- ↑ Vascular deposition of complement-split products in kidney allografts with cell-mediated rejection. Feucht HE, Felber E, Gokel MJ, Hillebrand G, Nattermann U, Brockmeyer C, Held E, Riethmüller G, Land W, Albert E. Clin Exp Immunol. 1991 Dec;86(3):464-70. PMID 1747954.
- ↑ Impact of humoral alloreactivity early after transplantation on the long-term survival of renal allografts. Lederer SR, Kluth-Pepper B, Schneeberger H, Albert E, Land W, Feucht HE. Kidney Int. 2001 Jan;59(1):334-41. PMID 11135088.
- ↑ URL: http://www.humpath.com/spip.php?article14451. Accessed on: 22 November 2011.
- ↑ Racusen LC, Solez K, Colvin RB, et al. (February 1999). "The Banff 97 working classification of renal allograft pathology". Kidney Int. 55 (2): 713–23. doi:10.1046/j.1523-1755.1999.00299.x. PMID 9987096. http://www.nature.com/ki/journal/v55/n2/full/4490631a.html.
- ↑ 6.0 6.1 Haas, M. (Oct 2011). "Transplant glomerulopathy: it's not always about chronic rejection.". Kidney Int 80 (8): 801-3. doi:10.1038/ki.2011.192. PMID 21960169.
- ↑ 7.0 7.1 Fogo, Agnes B.; Kashgarian, Michael (2005). Diagnostic Atlas of Renal Pathology: A Companion to Brenner and Rector's The Kidney 7E (1st ed.). Saunders. pp. 411. ISBN 978-1416028710.
- ↑ Joosten, SA.; Sijpkens, YW.; van Kooten, C.; Paul, LC. (Jul 2005). "Chronic renal allograft rejection: pathophysiologic considerations.". Kidney Int 68 (1): 1-13. doi:10.1111/j.1523-1755.2005.00376.x. PMID 15954891.
- ↑ Paul, LC. (Sep 1999). "Chronic allograft nephropathy: An update.". Kidney Int 56 (3): 783-93. doi:10.1046/j.1523-1755.1999.00611.x. PMID 10469349.
- ↑ Zarifian A, Meleg-Smith S, O'donovan R, Tesi RJ, Batuman V (June 1999). "Cyclosporine-associated thrombotic microangiopathy in renal allografts". Kidney Int. 55 (6): 2457–66. doi:10.1046/j.1523-1755.1999.00492.x. PMID 10354295.
- ↑ Fogo, Agnes; Bruijn, Jan A.; Cohen, Arthur H.; Colvin, Robert B.;Jennette, J. Charles (2006). Fundamentals of Renal Pathology (1st ed.). Springer. pp. 203. ISBN 978-0387311265.