Pseudomembranous colitis
Jump to navigation
Jump to search
| Pseudomembranous colitis | |
|---|---|
| Diagnosis in short | |
 Colonic pseudomembrane. H&E stain. | |
|
| |
| Synonyms | C. difficile colitis not the same from the perspective of pathology; however, pseudomembranous colitis is commonly used as synonym for C. difficile colitis by clinicians |
|
| |
| LM | heaped necrotic surface epithelium (described as "volanco lesions"), PMNs in lamina propria, +/-capillary fibrin thrombi |
| LM DDx | cap polyposis, signet ring cell carcinoma (uncommonly), ischemic colitis in general |
| Site | colon |
|
| |
| Symptoms | diarrhea, abdominal pain, fever |
| Prevalence | uncommon |
| Endoscopy | pseudomembranes (pale yellow (or white) irregular, raised mucosal lesions), interlesional mucosa often near normal grossly |
| Prognosis | dependent on comorbidities |
| Other | C. difficile toxin test positive (may be negative) |
| Treatment | dependent on underlying cause, antibiotics in C. difficile - occasionally surgical resection |
Pseudomembranous colitis an inflammation of the colon (colitis) with a characteristic endoscopic/gross appearance. It is closely associated with C. difficile infections; however, may be seen in a number of different situations.
General
- Pseudomembranous colitis is a histomorphologic description which has a DDx. In other words, it can be caused by a number of things.
Etiology
DDx of pseudomembranous colitis:[1]
- C. difficile.
- Known as C. difficile colitis.
- Ischemic colitis.
- Volvulus.
- Other infections.
Etiology:
- Anything that causes a severe mucosal injury.
Clostridium difficile
Main article: Clostridium difficile
Epidemiology of C. difficile pseudomembranous colitis:[2]
- Antibiotics prior to onset (classic history).[3]
- Typically hospitalized.
- Typically older individuals.
Clinical:[4]
- Diarrhea - usu. non-bloody - classic finding.
- +/-Fever.
- +/-Abdominal pain.
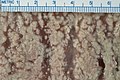
Gross
Features:[5]
- Pseudomembranes:
- Pale yellow (or white) irregular, raised mucosal lesions.
- Early lesions: typical <10 mm.
- Interlesional mucosa often near normal grossly.
Images
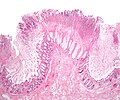
Microscopic
Features:[1]
- Heaped necrotic surface epithelium.
- Described as "volanco lesions" - this is what is seen endoscopically.
- PMNs in lamina propria.
- +/-Capillary fibrin thrombi.
Notes:
- Pseudomembranes arise from the crypts.
- Rarely have (benign) signet ring cell-like cells.[6]
DDx:
- Cap polyposis - very rare.
- Signet ring cell carcinoma.
- Ischemic colitis - in general.
Images
www:
Sign out
- It is worth mentioning that pseudomembranous colitis has a differential diagnosis when considered from the morphology.
See also
References
- ↑ 1.0 1.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 837-8. ISBN 0-7216-0187-1.
- ↑ Jones, AM.; Kuijper, EJ.; Wilcox, MH. (Feb 2013). "Clostridium difficile: a European perspective.". J Infect 66 (2): 115-28. doi:10.1016/j.jinf.2012.10.019. PMID 23103666.
- ↑ Bassetti, M.; Villa, G.; Pecori, D.; Arzese, A.; Wilcox, M. (Dec 2012). "Epidemiology, diagnosis and treatment of Clostridium difficile infection.". Expert Rev Anti Infect Ther 10 (12): 1405-23. doi:10.1586/eri.12.135. PMID 23253319.
- ↑ Gröschel, DH. (1996). "Clostridium difficile infection.". Crit Rev Clin Lab Sci 33 (3): 203-45. doi:10.3109/10408369609083061. PMID 8828001.
- ↑ URL: http://radiology.uchc.edu/eAtlas/GI/1749.htm. Accessed on: 22 May 2012.
- ↑ Abdulkader, I.; Cameselle-Teijeiro, J.; Forteza, J. (Apr 2003). "Signet-ring cells associated with pseudomembranous colitis.". Virchows Arch 442 (4): 412-4. doi:10.1007/s00428-003-0779-1. PMID 12684766.