Difference between revisions of "Peripheral nerve sheath tumours"
(→Perineurioma: rm pathconsultddx.com) |
|||
| (76 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
'''Peripheral nerve sheath tumours''', abbreviated '''PNSTs''', are common in [[neuropathology]] and occasionally show-up elsewhere. A very common PNST is the [[ | '''Peripheral nerve sheath tumours''', abbreviated '''PNSTs''', are common in [[neuropathology]] and occasionally show-up elsewhere. A very common PNST is the [[schwannoma]]. | ||
=Classification= | |||
A classification:<ref name=pmid17893219>{{cite journal |author=Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A |title=Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns |journal=AJNR Am J Neuroradiol |volume=28 |issue=9 |pages=1633–8 |year=2007 |month=October |pmid=17893219 |doi=10.3174/ajnr.A0682 |url=http://www.ajnr.org/cgi/reprint/28/9/1633}}</ref> | A classification:<ref name=pmid17893219>{{cite journal |author=Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A |title=Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns |journal=AJNR Am J Neuroradiol |volume=28 |issue=9 |pages=1633–8 |year=2007 |month=October |pmid=17893219 |doi=10.3174/ajnr.A0682 |url=http://www.ajnr.org/cgi/reprint/28/9/1633}}</ref> | ||
*Benign: | *Benign: | ||
| Line 11: | Line 11: | ||
**[[Malignant peripheral nerve sheath tumour]] (MPNST). | **[[Malignant peripheral nerve sheath tumour]] (MPNST). | ||
=Specific diagnoses= | |||
==Schwannoma== | ==Schwannoma== | ||
{{Main|Schwannoma}} | |||
==Perineurioma== | ==Perineurioma== | ||
{{Main|Perineurioma}} | |||
==Traumatic neuroma== | ==Traumatic neuroma== | ||
:May be referred to as ''[[neuroma]]''. | |||
{{Main|Traumatic neuroma}} | |||
==Palisaded encapsulated neuroma== | ==Palisaded encapsulated neuroma== | ||
*Abbreviated ''PEN''. | *Abbreviated ''PEN''. | ||
*[[AKA]] ''palisaded and encapsulated neuroma''. | *[[AKA]] ''palisaded and encapsulated neuroma''. | ||
*[[AKA]] ''solitary circumscribed neuroma''. | |||
===General=== | ===General=== | ||
*Flesh-colour papule - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> | *Flesh-colour [[papule]] - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> | ||
*Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | *Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | ||
*Superficial skin.<ref>S. Sade. 8 September 2011.</ref> | *Superficial skin papule.<ref>S. Sade. 8 September 2011.</ref> | ||
*It is considered hyperplastic rather than neoplastic. <ref>Rosai & Ackermann, Surgical Pathology, 10th ed. p183</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 124: | Line 40: | ||
**#Not vacuolated. | **#Not vacuolated. | ||
**#Nuclei have pointy ends. | **#Nuclei have pointy ends. | ||
**#Sometimes epitheloid appearance. | |||
*Intralesional clefts. | *Intralesional clefts. | ||
**Useful to differentiate from schwannoma. | **Useful to differentiate from schwannoma. | ||
| Line 138: | Line 55: | ||
Images: | Images: | ||
*[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | *[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | ||
<gallery> | |||
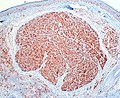
File:Palisaded_and_Encapsulated_Neuroma_(3952635881).jpg | Palisaded and encapsulated neuroma (Ed Uthman) | |||
File:Palisaded_and_Encapsulated_Neuroma,_S-100_Immunostain_(3953412396).jpg| PEN, S-100 staining (Ed Uthman) | |||
</gallery> | |||
[[File:569 dp sl 1.png| Palisading/encapcuslated neuroma]] | |||
[[File:569 dp sl 2.png| Palisading/encapcuslated neuroma]]<br> | |||
Palisading/encapsulated (Reed’s) neuroma. A. A dermal nodule shows an attenuated capsule (black arrows) about a fasciculated spindle cell lesion with artefactual clefts (green arrows). B. The bland spindled nuclei, amid clear cytoplasm with thin eosinophilic wisps, are often wavy (black arrows), with pointed ends (green arrows); leiomyomas have blunt ended nuclei and more eosinophilic cytoplasm. These benign neoplasms, unlike neurofibromas, lack an association with neurofibromatosis. | |||
===IHC=== | ===IHC=== | ||
| Line 145: | Line 71: | ||
==Neurofibroma== | ==Neurofibroma== | ||
{{Main|Neurofibroma}} | |||
Includes discussion of ''plexiform neurofibroma''. | |||
==Neurothekeoma== | |||
{{Main|Neurothekeoma}} | |||
=== | ==Malignant peripheral nerve sheath tumour== | ||
{{Main|Malignant peripheral nerve sheath tumour}} | |||
==Malignant triton tumour== | |||
*[[ | *Abbreviated ''MTT''. | ||
*[[AKA]] ''malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation''.<ref name=pmid17149968>{{Cite journal | last1 = Stasik | first1 = CJ. | last2 = Tawfik | first2 = O. | title = Malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation (malignant triton tumor). | journal = Arch Pathol Lab Med | volume = 130 | issue = 12 | pages = 1878-81 | month = Dec | year = 2006 | doi = 10.1043/1543-2165(2006)130[1878:MPNSTW]2.0.CO;2 | PMID = 17149968 }}</ref> | |||
===General=== | ===General=== | ||
*Rare. | *Rare. | ||
* | *Considered to be a variant of ''[[MPNST]]''. | ||
*Prognosis worse that conventional MPNST.<ref name=pmid17149968/> | |||
**Five year survival ~14%.<ref name=pmid22253011>{{Cite journal | last1 = McConnell | first1 = YJ. | last2 = Giacomantonio | first2 = CA. | title = Malignant triton tumors-complete surgical resection and adjuvant radiotherapy associated with improved survival. | journal = J Surg Oncol | volume = | issue = | pages = | month = Jan | year = 2012 | doi = 10.1002/jso.23042 | PMID = 22253011 }}</ref> | |||
*Diagnosis may require clinical information, i.e. individual has a history of [[neurofibromatosis type 1]] (NF1). | |||
Note: | |||
*A handful of ''benign triton tumours'' are reported; these are considered ''neuromuscular [[hamartoma]]s''.<ref name=pmid15814954>{{Cite journal | last1 = Castro | first1 = DE. | last2 = Raghuram | first2 = K. | last3 = Phillips | first3 = CD. | title = Benign triton tumor of the trigeminal nerve. | journal = AJNR Am J Neuroradiol | volume = 26 | issue = 4 | pages = 967-9 | month = Apr | year = 2005 | doi = | PMID = 15814954 }} | |||
</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name= | Features - Woodruff criteria - all three required:<ref name=pmid17149968/> | ||
# (a) Tumour arise from a peripheral nerve ''or'' (b) individual has [[NF1]] ''or'' (c) lesion a metastasis arising in the context of (a) or (b). | |||
# Schwann cell tumour characteristics. | |||
* | # Rhabdomyoblasts. | ||
* | #* Eccentric nucleus. | ||
#* Moderate amount of eosinophilic cytoplasm. | |||
#* +/-Cross-striations. | |||
DDx: | |||
* | *[[Malignant peripheral nerve sheath tumour]]. | ||
* | *[[Adult fibrosarcoma]]. | ||
*[[Synovial sarcoma]]. | |||
*[[Rhabdomyosarcoma]]. | |||
*[[Carcinosarcoma]]. | |||
*[[ | |||
*[[ | |||
*[ | |||
===IHC=== | ===IHC=== | ||
Features: | Features: | ||
* | *S100 +ve/-ve -- usu. focal if positive.<ref name=pmid17149968/> | ||
*Leu-7 +ve/-ve. | |||
* | *Myelin basic protein +ve/-ve. | ||
* | |||
Rhabdomyoblastic differentiation:<ref name=pmid17149968/> | |||
* | *Desmin. | ||
* | *Actin. | ||
*Myogenin. | |||
===EM=== | |||
*+/-Sarcomeres.<ref name=pmid17149968/> | |||
* | |||
==Morton neuroma== | |||
:[[AKA]] ''plantar interdigital neuroma''.<ref name=pmid22995258>{{Cite journal | last1 = Makki | first1 = D. | last2 = Haddad | first2 = BZ. | last3 = Mahmood | first3 = Z. | last4 = Shahid | first4 = MS. | last5 = Pathak | first5 = S. | last6 = Garnham | first6 = I. | title = Efficacy of corticosteroid injection versus size of plantar interdigital neuroma. | journal = Foot Ankle Int | volume = 33 | issue = 9 | pages = 722-6 | month = Sep | year = 2012 | doi = DOI: 10.3113/FAI.2012.0722 | PMID = 22995258 }}</ref> | |||
{{Main|Morton neuroma}} | |||
=See also= | |||
*[[Neuropathology]]. | *[[Neuropathology]]. | ||
*[[Gastrointestinal pathology]]. | *[[Gastrointestinal pathology]]. | ||
=References= | |||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Neuropathology]] | [[Category:Neuropathology]] | ||
[[Category:Peripheral nerve sheath tumours]] | |||
Latest revision as of 14:18, 29 August 2018
Peripheral nerve sheath tumours, abbreviated PNSTs, are common in neuropathology and occasionally show-up elsewhere. A very common PNST is the schwannoma.
Classification
A classification:[1]
- Benign:
- Malignant:
Specific diagnoses
Schwannoma
Perineurioma
Traumatic neuroma
- May be referred to as neuroma.
Palisaded encapsulated neuroma
General
- Flesh-colour papule - classically on the face.[2]
- Isolated finding - not associated with a systemic disease or malignancy.[3]
- Superficial skin papule.[4]
- It is considered hyperplastic rather than neoplastic. [5]
Microscopic
Features:[2]
- Encapsulated dermal spindle cell lesion.
- Fasciular arrangement.
- Neural-type spindle cells:
- Not vacuolated.
- Nuclei have pointy ends.
- Sometimes epitheloid appearance.
- Intralesional clefts.
- Useful to differentiate from schwannoma.
DDx:
- Schwannoma:[2]
- No intralesional clefts.
- More variability in the cellularity.
- May be deep.
Other considerations:
- Leiomyoma - cytoplasm not vacuolated, nuclei more elliptical.
Images:


Palisading/encapsulated (Reed’s) neuroma. A. A dermal nodule shows an attenuated capsule (black arrows) about a fasciculated spindle cell lesion with artefactual clefts (green arrows). B. The bland spindled nuclei, amid clear cytoplasm with thin eosinophilic wisps, are often wavy (black arrows), with pointed ends (green arrows); leiomyomas have blunt ended nuclei and more eosinophilic cytoplasm. These benign neoplasms, unlike neurofibromas, lack an association with neurofibromatosis.
IHC
Features:[3]
- S100 +ve.
- EMA +ve (capsule of lesion).
Neurofibroma
Includes discussion of plexiform neurofibroma.
Neurothekeoma
Malignant peripheral nerve sheath tumour
Malignant triton tumour
- Abbreviated MTT.
- AKA malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation.[6]
General
- Rare.
- Considered to be a variant of MPNST.
- Prognosis worse that conventional MPNST.[6]
- Five year survival ~14%.[7]
- Diagnosis may require clinical information, i.e. individual has a history of neurofibromatosis type 1 (NF1).
Note:
- A handful of benign triton tumours are reported; these are considered neuromuscular hamartomas.[8]
Microscopic
Features - Woodruff criteria - all three required:[6]
- (a) Tumour arise from a peripheral nerve or (b) individual has NF1 or (c) lesion a metastasis arising in the context of (a) or (b).
- Schwann cell tumour characteristics.
- Rhabdomyoblasts.
- Eccentric nucleus.
- Moderate amount of eosinophilic cytoplasm.
- +/-Cross-striations.
DDx:
- Malignant peripheral nerve sheath tumour.
- Adult fibrosarcoma.
- Synovial sarcoma.
- Rhabdomyosarcoma.
- Carcinosarcoma.
IHC
Features:
- S100 +ve/-ve -- usu. focal if positive.[6]
- Leu-7 +ve/-ve.
- Myelin basic protein +ve/-ve.
Rhabdomyoblastic differentiation:[6]
- Desmin.
- Actin.
- Myogenin.
EM
- +/-Sarcomeres.[6]
Morton neuroma
See also
References
- ↑ Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A (October 2007). "Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns". AJNR Am J Neuroradiol 28 (9): 1633–8. doi:10.3174/ajnr.A0682. PMID 17893219. http://www.ajnr.org/cgi/reprint/28/9/1633.
- ↑ 2.0 2.1 2.2 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 536. ISBN 978-0443066542.
- ↑ 3.0 3.1 3.2 Newman, MD.; Milgraum, S. (2008). "Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor.". Dermatol Online J 14 (7): 12. PMID 18718196.
- ↑ S. Sade. 8 September 2011.
- ↑ Rosai & Ackermann, Surgical Pathology, 10th ed. p183
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Stasik, CJ.; Tawfik, O. (Dec 2006). "Malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation (malignant triton tumor).". Arch Pathol Lab Med 130 (12): 1878-81. doi:10.1043/1543-2165(2006)130[1878:MPNSTW]2.0.CO;2. PMID 17149968.
- ↑ McConnell, YJ.; Giacomantonio, CA. (Jan 2012). "Malignant triton tumors-complete surgical resection and adjuvant radiotherapy associated with improved survival.". J Surg Oncol. doi:10.1002/jso.23042. PMID 22253011.
- ↑ Castro, DE.; Raghuram, K.; Phillips, CD. (Apr 2005). "Benign triton tumor of the trigeminal nerve.". AJNR Am J Neuroradiol 26 (4): 967-9. PMID 15814954.
- ↑ Makki, D.; Haddad, BZ.; Mahmood, Z.; Shahid, MS.; Pathak, S.; Garnham, I. (Sep 2012). "Efficacy of corticosteroid injection versus size of plantar interdigital neuroma.". Foot Ankle Int 33 (9): 722-6. doi:DOI: 10.3113/FAI.2012.0722. PMID 22995258.