Difference between revisions of "Osteoarthritis"
Jump to navigation
Jump to search
(create) |
|||
| (48 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Osteoarthritis''' is a degenerative disease of the joint. | |||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Degenerative joint disease - severe - alt -- low mag.jpg | |||
| Width = | |||
| Caption = Severe degenerative joint disease. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = vertical clefts of the cartilage, +/-thickening of [[bone|bony]] trabeculae, subchondral cysts (where there is cartilage loss), +/-mild inflammation (lymphocytes), +/-villous hyperplasia (synovium has finger-like projections into the joint space), osteophytes (ossified projections at the edge of the articular cartilage) | |||
| Subtypes = | |||
| LMDDx = [[rheumatoid arthritis]], infectious arthritis, arthritis secondary to other disease (IBD, rheumatologic condition), trauma/deformity related, [[AVN]]-related | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = thinning/loss of cartilage, osteophyte formation, subchondral cysts, subchondral sclerosis | |||
| Grossing = [[femoral head grossing]], [[knee replacement specimen grossing]] | |||
| Site = [[joints]], e.g. [[femoral head]], knee, shoulder | |||
| Assdx = trauma to joint, [[obesity]] (for knees), congenital disease ([[SCFE]], [[Legg–Calvé–Perthes disease]]), complication of [[avascular necrosis of the femoral head]] | |||
| Syndromes = | |||
| Clinicalhx = often old, +/-history of trauma | |||
| Signs = | |||
| Symptoms = joint pain worse with activity, "morning stiffness" | |||
| Prevalence = very common | |||
| Bloodwork = | |||
| Rads = joint space narrowing, osteophyte formation, subchondral cysts, subchondral sclerosis | |||
| Endoscopy = | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = other types of [[arthritis]] | |||
| Tx = pain medications, joint replacement | |||
}} | |||
'''Osteoarthritis''', abbreviated '''OA''', is a degenerative disease of the joint. | |||
==General== | |||
Clinical: | |||
*Morning stiffness (<30 minutes).<ref name=pmid24881169>{{Cite journal | last1 = Negoescu | first1 = A. | last2 = Ostör | first2 = AJ. | title = Self-management pivotal in osteoarthritis. | journal = Practitioner | volume = 258 | issue = 1770 | pages = 25-8, 3 | month = Apr | year = 2014 | doi = | PMID = 24881169 }}</ref> | |||
*Worse with exercise.<ref>URL: [http://www.nlm.nih.gov/medlineplus/ency/article/000423.htm http://www.nlm.nih.gov/medlineplus/ency/article/000423.htm]. Accessed on: October 25, 2014.</ref> | |||
Management: | |||
*Acetaminophen (paracetamol). | |||
*Other analgesics. | |||
*Joint replacement. | |||
===Risks=== | |||
It is associated with:<ref name=pmid20302555>{{Cite journal | last1 = Martel-Pelletier | first1 = J. | last2 = Pelletier | first2 = JP. | title = Is osteoarthritis a disease involving only cartilage or other articular tissues? | journal = Eklem Hastalik Cerrahisi | volume = 21 | issue = 1 | pages = 2-14 | month = Apr | year = 2010 | doi = | PMID = 20302555 | url=http://www.ncbi.nlm.nih.gov/corehtml/query/egifs/http:--www.tevak.org-images-Eklemlinkout.png }} | |||
</ref> | |||
*Advanced age. | |||
*Trauma. | |||
*Unusual loading (bony misalignment, [[obesity]]). | |||
==Gross pathology/radiology== | ==Gross pathology/radiology== | ||
Features:<ref>{{Cite journal | last1 = Swagerty | first1 = DL. | last2 = Hellinger | first2 = D. | title = Radiographic assessment of osteoarthritis. | journal = Am Fam Physician | volume = 64 | issue = 2 | pages = 279-86 | month = Jul | year = 2001 | doi = | PMID = 11476273 | url= http://www.aafp.org/afp/2001/0715/p279.html }}</ref> | Features - joints (internal):<ref name=pmid11476273>{{Cite journal | last1 = Swagerty | first1 = DL. | last2 = Hellinger | first2 = D. | title = Radiographic assessment of osteoarthritis. | journal = Am Fam Physician | volume = 64 | issue = 2 | pages = 279-86 | month = Jul | year = 2001 | doi = | PMID = 11476273 | url= http://www.aafp.org/afp/2001/0715/p279.html }}</ref> | ||
#Loss of cartilage, especially asymmetrical. | |||
* | #*Marble-like appearance - polished appearance known as ''eburnation''. | ||
*Subchondral cysts. | #[[Osteophyte]] formation. | ||
*Subchondral | #Subchondral cysts - located where there is loss of cartilage.<ref name=pmid404905>{{Cite journal | last1 = Resnick | first1 = D. | last2 = Niwayama | first2 = G. | last3 = Coutts | first3 = RD. | title = Subchondral cysts (geodes) in arthritic disorders: pathologic and radiographic appearance of the hip joint. | journal = AJR Am J Roentgenol | volume = 128 | issue = 5 | pages = 799-806 | month = May | year = 1977 | doi = | PMID = 404905 }}</ref> | ||
#Subchondral sclerosis. | |||
Memory device ''LOSS'': | |||
*''L''oss of cartilage, ''O''steophyte formation, ''S''ubchondral cysts, ''S''ubchondral sclerosis. | |||
Notes: | |||
*Osteophytes are classically medial and lateral in the hip.<ref name=pmid12597129>{{Cite journal | last1 = Claassen | first1 = H. | last2 = Tschirner | first2 = T. | title = Topographical and histological examination of osteophytes taken from arthrotic femoral heads. | journal = Ann Anat | volume = 185 | issue = 1 | pages = 67-71 | month = Jan | year = 2003 | doi = | PMID = 12597129 }}</ref> | |||
**They tend to form in areas with high loading. | |||
*Subchondral cysts are also seen in [[rheumatoid arthritis]].<ref name=pmid404905/> | |||
Clinical findings (external): | |||
*Heberden's node - swelling of distal interphalangeal joints. | |||
==Microscopic== | |||
Features:<ref name=Ref_WMSP658>{{Ref WMSP|658}}</ref> | |||
*Vertical clefts of the cartilage - characteristic. | |||
*Thickening of [[bone|bony]] trabeculae (reactive phenomenon) due to fibrosis. | |||
*Subchondral cysts (associated with cartilage loss). | |||
*+/-Mild inflammation (lymphocytes). | |||
*+/-Villous hyperplasia - synovium has finger-like projections into the joint space. | |||
**Normal synovium has a flat surface. | |||
*Osteophytes - ossified projections at the edge of the articular cartilage (bony spurs). | |||
Note: | |||
*Cartilaginous calcification is seen with OA; however, it is thought to be due to aging.<ref name=pmid17276093>{{Cite journal | last1 = Mitsuyama | first1 = H. | last2 = Healey | first2 = RM. | last3 = Terkeltaub | first3 = RA. | last4 = Coutts | first4 = RD. | last5 = Amiel | first5 = D. | title = Calcification of human articular knee cartilage is primarily an effect of aging rather than osteoarthritis. | journal = Osteoarthritis Cartilage | volume = 15 | issue = 5 | pages = 559-65 | month = May | year = 2007 | doi = 10.1016/j.joca.2006.10.017 | PMID = 17276093 }}</ref> | |||
DDx: | |||
*Osteoarthritis secondary to another cause. | |||
**[[Avascular necrosis of the femoral head]]. | |||
**Trauma. | |||
**[[Slipped capital femoral epiphysis]] (SCFE).<ref>{{Cite journal | last1 = Abraham | first1 = E. | last2 = Gonzalez | first2 = MH. | last3 = Pratap | first3 = S. | last4 = Amirouche | first4 = F. | last5 = Atluri | first5 = P. | last6 = Simon | first6 = P. | title = Clinical implications of anatomical wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis. | journal = J Pediatr Orthop | volume = 27 | issue = 7 | pages = 788-95 | month = | year = | doi = 10.1097/BPO.0b013e3181558c94 | PMID = 17878786 }}</ref> | |||
===Grading=== | |||
A grading system exists from ''Pritzker'' and colleagues:<ref name=pmid16242352>{{Cite journal | last1 = Pritzker | first1 = KP. | last2 = Gay | first2 = S. | last3 = Jimenez | first3 = SA. | last4 = Ostergaard | first4 = K. | last5 = Pelletier | first5 = JP. | last6 = Revell | first6 = PA. | last7 = Salter | first7 = D. | last8 = van den Berg | first8 = WB. | title = Osteoarthritis cartilage histopathology: grading and staging. | journal = Osteoarthritis Cartilage | volume = 14 | issue = 1 | pages = 13-29 | month = Jan | year = 2006 | doi = 10.1016/j.joca.2005.07.014 | PMID = 16242352 }}</ref> | |||
{| class="wikitable sortable" | |||
! Grade | |||
! Key feature | |||
! Additional findings | |||
|- | |||
| Grade 0 (normal) | |||
| surface intact | |||
| normal thickness | |||
|- | |||
| Grade 1 | |||
| surface intact but uneven | |||
| +/-surface fibrillation, +/-superficial proliferation/cellular enlargement | |||
|- | |||
| Grade 2 | |||
| discontinuous surface (diffuse superficial fibrillation ''or'' surface abrasions) | |||
| +/-chondron columns disoriented | |||
|- | |||
| Grade 3 | |||
| vertical fissures (simple or branched) | |||
| +/-new collagen formation (seen with polarized light) | |||
|- | |||
| Grade 4 | |||
| erosion (cartilage loss) | |||
| +/- cartilageous cyst formation | |||
|- | |||
| Grade 5 | |||
| complete cartilage loss | |||
| no deformation | |||
|- | |||
| Grade 6 | |||
| deformed bone (osteophytes peripheral or central) | |||
| +/-deformation of articular surface +/-microfractures | |||
|} | |||
===Images=== | |||
<gallery> | |||
Image: Degenerative joint disease - severe -- very low mag.jpg | Severe DJD - very low mag. | |||
Image: Degenerative joint disease - severe - alt -- very low mag.jpg | Severe DJD - very low mag. | |||
Image: Degenerative joint disease - severe -- low mag.jpg | Severe DJD - low mag. | |||
Image: Degenerative joint disease - severe - alt -- low mag.jpg | Severe DJD - low mag. | |||
Image: Degenerative joint disease - severe -- intermed mag.jpg | Severe DJD - intermed. mag. | |||
</gallery> | |||
<gallery> | |||
Image: Degenerative joint disease -- very low mag.jpg | Moderate DJD - very low mag. | |||
Image: Degenerative joint disease -- low mag.jpg | Moderate DJD - low mag. | |||
Image: Degenerative joint disease - alt -- low mag.jpg | Moderate DJD - low mag. | |||
Image: Degenerative joint disease -- intermed mag.jpg | Moderate DJD - intermed. mag. | |||
Image: Degenerative joint disease - alt -- intermed mag.jpg | Moderate DJD - intermed. mag. | |||
</gallery> | |||
www: | |||
*[http://ars.els-cdn.com/content/image/1-s2.0-S8756328212000683-gr1.jpg Osteoarthritis showing villous hyperplasia - panel B (els-cdn.com)]. | |||
*[http://www.medpath.info/MainContent/Skeletal/3097.GIF Osteophyte (medpath.info)].<ref>URL: [http://www.medpath.info/MainContent/Skeletal/Joint_02.html http://www.medpath.info/MainContent/Skeletal/Joint_02.html]. Accessed on: 10 November 2012.</ref> | |||
*[http://images.rheumatology.org/viewphoto.php?imageId=2862378 OA (rheumatology.org)]. | |||
*[http://www.med.nyu.edu/medicine/labs/abramsonlab/images/Fig-2-cartilage_histology-orig.jpg?CSRT=6720621554912944884 OA versus normal (med.nyu.edu)].<ref>URL: [http://www.med.nyu.edu/medicine/labs/abramsonlab/basic-arth-research.html http://www.med.nyu.edu/medicine/labs/abramsonlab/basic-arth-research.html]. Accessed on: 10 November 2012.</ref> | |||
*[http://www.medic.usm.my/~pathology/bonepath/bonepath/Ostart2.jpg OA with clefting (usm.my)].<ref>URL: [http://www.medic.usm.my/~pathology/bonepath/bonepath/Osteoathritis.html http://www.medic.usm.my/~pathology/bonepath/bonepath/Osteoathritis.html]. Accessed on: 22 November 2012.</ref> | |||
*[http://images.rheumatology.org/viewphoto.php?albumId=75691&imageId=2862380 OA with clefting (rheumatology.org)]. | |||
==Sign out== | |||
===Hip=== | |||
<pre> | |||
FEMORAL HEAD, RIGHT, HIP ARTHROPLASTY: | |||
- DEGENERATIVE JOINT DISEASE. | |||
</pre> | |||
====Gross only==== | |||
<pre> | |||
FEMORAL HEAD AND JOINT CAPSULE, RIGHT, EXCISION: | |||
- DEGENERATIVE JOINT DISEASE (GROSS ONLY). | |||
</pre> | |||
<pre> | |||
FEMORAL HEAD AND JOINT CAPSULE, LEFT, EXCISION: | |||
- DEGENERATIVE JOINT DISEASE (GROSS ONLY). | |||
</pre> | |||
===Knee=== | |||
<pre> | |||
SYNOVIUM, LEFT KNEE, BIOPSY: | |||
- SYNOVIUM WITH MILD CHRONIC INFLAMMATION AND VILLOUS HYPERPLASIA -- COMPATIBLE | |||
WITH OSTEOARTHRITIS. | |||
</pre> | |||
===Micro=== | |||
The sections show thinned cartilage composed of chrondrocytes clusters separated by vertical fibrous septa. The deep aspect of the cartilage is basophilic. An osteophyte is present. | |||
The soft tissue shows a minimal, focal chronic inflammatory cells. | |||
Note: | |||
*''Noninflammatory degenerative joint disease'' is the term used by the ICD.<ref>URL: [http://www.icd9data.com/2012/Volume1/710-739/710-719/715/715.9.htm http://www.icd9data.com/2012/Volume1/710-739/710-719/715/715.9.htm]. Accessed on: 15 March 2013.</ref> | |||
==See also== | ==See also== | ||
| Line 12: | Line 184: | ||
*[[Bone]]. | *[[Bone]]. | ||
*[[Chondro-osseous tumours]]. | *[[Chondro-osseous tumours]]. | ||
*[[Arthritis]]. | |||
**[[Rheumatoid arthritis]]. | |||
==References== | ==References== | ||
{{Reflist| | {{Reflist|2}} | ||
[[Category:Soft tissue]] | [[Category:Soft tissue lesions]] | ||
[[Category:Diagnosis]] | |||
Latest revision as of 16:02, 11 May 2016
Osteoarthritis, abbreviated OA, is a degenerative disease of the joint.
| Osteoarthritis | |
|---|---|
| Diagnosis in short | |
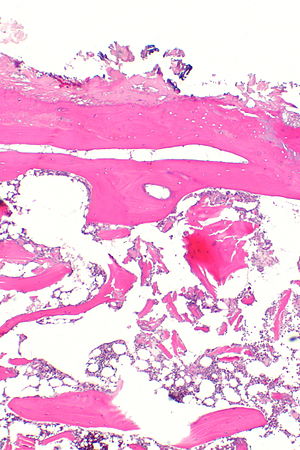 Severe degenerative joint disease. H&E stain. | |
|
| |
| LM | vertical clefts of the cartilage, +/-thickening of bony trabeculae, subchondral cysts (where there is cartilage loss), +/-mild inflammation (lymphocytes), +/-villous hyperplasia (synovium has finger-like projections into the joint space), osteophytes (ossified projections at the edge of the articular cartilage) |
| LM DDx | rheumatoid arthritis, infectious arthritis, arthritis secondary to other disease (IBD, rheumatologic condition), trauma/deformity related, AVN-related |
| Gross | thinning/loss of cartilage, osteophyte formation, subchondral cysts, subchondral sclerosis |
| Grossing notes | femoral head grossing, knee replacement specimen grossing |
| Site | joints, e.g. femoral head, knee, shoulder |
|
| |
| Associated Dx | trauma to joint, obesity (for knees), congenital disease (SCFE, Legg–Calvé–Perthes disease), complication of avascular necrosis of the femoral head |
| Clinical history | often old, +/-history of trauma |
| Symptoms | joint pain worse with activity, "morning stiffness" |
| Prevalence | very common |
| Radiology | joint space narrowing, osteophyte formation, subchondral cysts, subchondral sclerosis |
| Prognosis | benign |
| Clin. DDx | other types of arthritis |
| Treatment | pain medications, joint replacement |
General
Clinical:
Management:
- Acetaminophen (paracetamol).
- Other analgesics.
- Joint replacement.
Risks
It is associated with:[3]
- Advanced age.
- Trauma.
- Unusual loading (bony misalignment, obesity).
Gross pathology/radiology
Features - joints (internal):[4]
- Loss of cartilage, especially asymmetrical.
- Marble-like appearance - polished appearance known as eburnation.
- Osteophyte formation.
- Subchondral cysts - located where there is loss of cartilage.[5]
- Subchondral sclerosis.
Memory device LOSS:
- Loss of cartilage, Osteophyte formation, Subchondral cysts, Subchondral sclerosis.
Notes:
- Osteophytes are classically medial and lateral in the hip.[6]
- They tend to form in areas with high loading.
- Subchondral cysts are also seen in rheumatoid arthritis.[5]
Clinical findings (external):
- Heberden's node - swelling of distal interphalangeal joints.
Microscopic
Features:[7]
- Vertical clefts of the cartilage - characteristic.
- Thickening of bony trabeculae (reactive phenomenon) due to fibrosis.
- Subchondral cysts (associated with cartilage loss).
- +/-Mild inflammation (lymphocytes).
- +/-Villous hyperplasia - synovium has finger-like projections into the joint space.
- Normal synovium has a flat surface.
- Osteophytes - ossified projections at the edge of the articular cartilage (bony spurs).
Note:
- Cartilaginous calcification is seen with OA; however, it is thought to be due to aging.[8]
DDx:
- Osteoarthritis secondary to another cause.
Grading
A grading system exists from Pritzker and colleagues:[10]
| Grade | Key feature | Additional findings |
|---|---|---|
| Grade 0 (normal) | surface intact | normal thickness |
| Grade 1 | surface intact but uneven | +/-surface fibrillation, +/-superficial proliferation/cellular enlargement |
| Grade 2 | discontinuous surface (diffuse superficial fibrillation or surface abrasions) | +/-chondron columns disoriented |
| Grade 3 | vertical fissures (simple or branched) | +/-new collagen formation (seen with polarized light) |
| Grade 4 | erosion (cartilage loss) | +/- cartilageous cyst formation |
| Grade 5 | complete cartilage loss | no deformation |
| Grade 6 | deformed bone (osteophytes peripheral or central) | +/-deformation of articular surface +/-microfractures |
Images
www:
Sign out
Hip
FEMORAL HEAD, RIGHT, HIP ARTHROPLASTY: - DEGENERATIVE JOINT DISEASE.
Gross only
FEMORAL HEAD AND JOINT CAPSULE, RIGHT, EXCISION: - DEGENERATIVE JOINT DISEASE (GROSS ONLY).
FEMORAL HEAD AND JOINT CAPSULE, LEFT, EXCISION: - DEGENERATIVE JOINT DISEASE (GROSS ONLY).
Knee
SYNOVIUM, LEFT KNEE, BIOPSY: - SYNOVIUM WITH MILD CHRONIC INFLAMMATION AND VILLOUS HYPERPLASIA -- COMPATIBLE WITH OSTEOARTHRITIS.
Micro
The sections show thinned cartilage composed of chrondrocytes clusters separated by vertical fibrous septa. The deep aspect of the cartilage is basophilic. An osteophyte is present.
The soft tissue shows a minimal, focal chronic inflammatory cells.
Note:
- Noninflammatory degenerative joint disease is the term used by the ICD.[14]
See also
References
- ↑ Negoescu, A.; Ostör, AJ. (Apr 2014). "Self-management pivotal in osteoarthritis.". Practitioner 258 (1770): 25-8, 3. PMID 24881169.
- ↑ URL: http://www.nlm.nih.gov/medlineplus/ency/article/000423.htm. Accessed on: October 25, 2014.
- ↑ Martel-Pelletier, J.; Pelletier, JP. (Apr 2010). "Is osteoarthritis a disease involving only cartilage or other articular tissues?". Eklem Hastalik Cerrahisi 21 (1): 2-14. PMID 20302555. http://www.ncbi.nlm.nih.gov/corehtml/query/egifs/http:--www.tevak.org-images-Eklemlinkout.png.
- ↑ Swagerty, DL.; Hellinger, D. (Jul 2001). "Radiographic assessment of osteoarthritis.". Am Fam Physician 64 (2): 279-86. PMID 11476273. http://www.aafp.org/afp/2001/0715/p279.html.
- ↑ 5.0 5.1 Resnick, D.; Niwayama, G.; Coutts, RD. (May 1977). "Subchondral cysts (geodes) in arthritic disorders: pathologic and radiographic appearance of the hip joint.". AJR Am J Roentgenol 128 (5): 799-806. PMID 404905.
- ↑ Claassen, H.; Tschirner, T. (Jan 2003). "Topographical and histological examination of osteophytes taken from arthrotic femoral heads.". Ann Anat 185 (1): 67-71. PMID 12597129.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 658. ISBN 978-0781765275.
- ↑ Mitsuyama, H.; Healey, RM.; Terkeltaub, RA.; Coutts, RD.; Amiel, D. (May 2007). "Calcification of human articular knee cartilage is primarily an effect of aging rather than osteoarthritis.". Osteoarthritis Cartilage 15 (5): 559-65. doi:10.1016/j.joca.2006.10.017. PMID 17276093.
- ↑ Abraham, E.; Gonzalez, MH.; Pratap, S.; Amirouche, F.; Atluri, P.; Simon, P.. "Clinical implications of anatomical wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis.". J Pediatr Orthop 27 (7): 788-95. doi:10.1097/BPO.0b013e3181558c94. PMID 17878786.
- ↑ Pritzker, KP.; Gay, S.; Jimenez, SA.; Ostergaard, K.; Pelletier, JP.; Revell, PA.; Salter, D.; van den Berg, WB. (Jan 2006). "Osteoarthritis cartilage histopathology: grading and staging.". Osteoarthritis Cartilage 14 (1): 13-29. doi:10.1016/j.joca.2005.07.014. PMID 16242352.
- ↑ URL: http://www.medpath.info/MainContent/Skeletal/Joint_02.html. Accessed on: 10 November 2012.
- ↑ URL: http://www.med.nyu.edu/medicine/labs/abramsonlab/basic-arth-research.html. Accessed on: 10 November 2012.
- ↑ URL: http://www.medic.usm.my/~pathology/bonepath/bonepath/Osteoathritis.html. Accessed on: 22 November 2012.
- ↑ URL: http://www.icd9data.com/2012/Volume1/710-739/710-719/715/715.9.htm. Accessed on: 15 March 2013.