Difference between revisions of "Neuroendocrine tumour of the appendix"
Jump to navigation
Jump to search
(→IHC) |
m (→Sign out: tweak) |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 15: | Line 15: | ||
*<1.0 cm - do not metastasize. | *<1.0 cm - do not metastasize. | ||
*1.0-2.0 cm - rarely metastasize. | *1.0-2.0 cm - rarely metastasize. | ||
Management: | |||
*Simple resection, e.g. appendectomy, sufficient for most tumours <2 cm.<ref name=pmid25840530>{{Cite journal | last1 = Nussbaum | first1 = DP. | last2 = Speicher | first2 = PJ. | last3 = Gulack | first3 = BC. | last4 = Keenan | first4 = JE. | last5 = Ganapathi | first5 = AM. | last6 = Englum | first6 = BR. | last7 = Tyler | first7 = DS. | last8 = Blazer | first8 = DG. | title = Management of 1- to 2-cm Carcinoid Tumors of the Appendix: Using the National Cancer Data Base to Address Controversies in General Surgery. | journal = J Am Coll Surg | volume = 220 | issue = 5 | pages = 894-903 | month = May | year = 2015 | doi = 10.1016/j.jamcollsurg.2015.01.005 | PMID = 25840530 }}</ref><ref name=pmid18338494>{{Cite journal | last1 = Fornaro | first1 = R. | last2 = Frascio | first2 = M. | last3 = Sticchi | first3 = C. | last4 = De Salvo | first4 = L. | last5 = Stabilini | first5 = C. | last6 = Mandolfino | first6 = F. | last7 = Ricci | first7 = B. | last8 = Gianetta | first8 = E. | title = Appendectomy or right hemicolectomy in the treatment of appendiceal carcinoid tumors? | journal = Tumori | volume = 93 | issue = 6 | pages = 587-90 | month = | year = | doi = | PMID = 18338494 }}</ref> | |||
==Gross== | ==Gross== | ||
| Line 109: | Line 112: | ||
The low-grade neuroendocrine tumour (in the planes of section) is in the tip and | The low-grade neuroendocrine tumour (in the planes of section) is in the tip and | ||
separate from the appendiceal perforation site/acute appendicitis. | separate from the appendiceal perforation site/acute appendicitis. | ||
The specimen was submitted in total. | |||
</pre> | </pre> | ||
Latest revision as of 14:41, 22 August 2019
Neuroendocrine tumour of the appendix is a common tumour of the vermiform appendix. It is also known as appendiceal neuroendocrine tumour, abbreviated appendiceal NET.
It was previously known as appendiceal carcinoid.
General
- Most common tumour of the appendix.[1]
- Not really common though - one is seen in approximately 300 appendectomies.[2]
Presentation
- Often found incidentally, may be microscopic.
- May cause obstruction leading to mucocele or acute appendicitis.
- May precipitate torsion.
Size matters in appendiceal NETs:[3]
- <1.0 cm - do not metastasize.
- 1.0-2.0 cm - rarely metastasize.
Management:
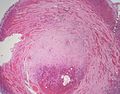
Gross
- Classically found in the tip of the appendix.
- Characteristic yellow cut surface post-fixation.
- Circumscribed but not encapsulated.
- Firm (due to desmoplasia).
- Centred in the submucosa.
- Nodules that do not usually cause erosion of the overlying mucosa.
Image
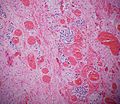
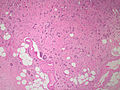
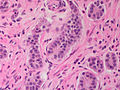
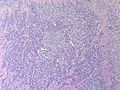
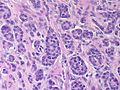
Microscopic
Features:
- Classically subepithelial/mural.
- Various growth patterns:
- Nested (insular).
- Trabecular.
- Palisading.
- Ribbons, rosettes.
- Fibrous stroma in between cell groups.
- Cytomorphology:
- Monotonous appearance with scanty mitoses.
- Round central nuclei.
- Stippled chromatin (AKA salt-and-pepper chromatin and coarse chromatin).
- Eosinophilic granular cytoplasm.
DDx:
- Colorectal adenocarcinoma.
- Adenocarcinoid.
- Crypt cell carcinoma, also known as goblet cell carcinoid.
- Metastatic adenocarcinoma.
- Normal ganglion cells in the Meissner plexus (submucosa) and Auerbach plexus (located between the inner and outer layers of the muscularis propria).
Special Types
- Tubular carcinoid.
- Neuroendocrine cells forming tubules (no cell nests).
- Some tubules can contain mucin.
- Can be confused with adenocarcinoma.
- Features suggesting tubular carcinoid (over adenocarcinoma):
- Arises from base of crypts, with no disruption of surface epithelium.
- No associated epithelial precursor (no adenomatous change).
- Neuroendocrine cytologic features, without prominent atypia.
- IHC (NE markers +ve).
- Goblet cell carcinoid - dealt with in the article crypt cell carcinoma.
- Signet-ring cells forming glandular structures.
- Possibly also with extra-cellular mucin.[citation needed]
Images
www:
- Appendiceal carcinoid (humpath.com).
- Carcinoid of the appendix (brown.edu).
- Appendiceal carcinoid (flickr.com/Qiao).
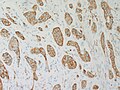
IHC
Features:
- Chromogranin A -ve/+ve.
- Synaptophysin +ve.
- Keratin positive.[citation needed]
- S100 positive for appendix.[citation needed]
Others:
- CK7 and CK20 variable.[6]
Sign out
Vermiform Appendix, Appendectomy:
- Low-grade neuroendocrine tumour (carcinoid tumour), see comment.
-- Margins clear.
-- Please see synoptic report.
- Perforated acute appendicitis with periappendicitis.
Comment:
The tumour stains as follows:
POSITIVE: AE1/AE3, chromogranin A, synaptophysin, CD56.
NEGATIVE: CK7, CK20, S100.
PROLIFERATION (Ki-67): <3%.
The low-grade neuroendocrine tumour (in the planes of section) is in the tip and
separate from the appendiceal perforation site/acute appendicitis.
The specimen was submitted in total.
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 435. ISBN 978-1416054542.
- ↑ Mitra, B.; Pal, M.; Paul, B.; Saha, TN.; Maiti, A. (2013). "Goblet cell carcinoid of appendix: A rare case with literature review.". Int J Surg Case Rep 4 (3): 334-7. doi:10.1016/j.ijscr.2013.01.007. PMID 23416502.
- ↑ Modlin, IM.; Lye, KD.; Kidd, M. (Feb 2003). "A 5-decade analysis of 13,715 carcinoid tumors.". Cancer 97 (4): 934-59. doi:10.1002/cncr.11105. PMID 12569593.
- ↑ Nussbaum, DP.; Speicher, PJ.; Gulack, BC.; Keenan, JE.; Ganapathi, AM.; Englum, BR.; Tyler, DS.; Blazer, DG. (May 2015). "Management of 1- to 2-cm Carcinoid Tumors of the Appendix: Using the National Cancer Data Base to Address Controversies in General Surgery.". J Am Coll Surg 220 (5): 894-903. doi:10.1016/j.jamcollsurg.2015.01.005. PMID 25840530.
- ↑ Fornaro, R.; Frascio, M.; Sticchi, C.; De Salvo, L.; Stabilini, C.; Mandolfino, F.; Ricci, B.; Gianetta, E.. "Appendectomy or right hemicolectomy in the treatment of appendiceal carcinoid tumors?". Tumori 93 (6): 587-90. PMID 18338494.
- ↑ Matsukuma, KE.; Montgomery, EA. (Jul 2012). "Tubular carcinoids of the appendix: the CK7/CK20 immunophenotype can be a diagnostic pitfall.". J Clin Pathol 65 (7): 666-8. doi:10.1136/jclinpath-2011-200639. PMID 22461652.