Difference between revisions of "Mucinous breast carcinoma"
Jump to navigation
Jump to search
(→Images) |
|||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 14: | Line 14: | ||
| IF = | | IF = | ||
| Gross = pale, glistening, jelly-like appearance | | Gross = pale, glistening, jelly-like appearance | ||
| Grossing = | | Grossing = [[breast grossing]] | ||
| Staging = [[breast cancer staging]] | |||
| Site = [[breast]] - see ''[[invasive breast cancer]]'' | | Site = [[breast]] - see ''[[invasive breast cancer]]'' | ||
| Assdx = | | Assdx = | ||
| Line 36: | Line 37: | ||
==General== | ==General== | ||
*Rare. | *Rare. | ||
*2% of invasive breast carcinomas. | |||
*Good prognosis.<ref name=pmid18809061>{{Cite journal | last1 = Barkley | first1 = CR. | last2 = Ligibel | first2 = JA. | last3 = Wong | first3 = JS. | last4 = Lipsitz | first4 = S. | last5 = Smith | first5 = BL. | last6 = Golshan | first6 = M. | title = Mucinous breast carcinoma: a large contemporary series. | journal = Am J Surg | volume = 196 | issue = 4 | pages = 549-51 | month = Oct | year = 2008 | doi = 10.1016/j.amjsurg.2008.06.013 | PMID = 18809061 }}</ref> | *Good prognosis.<ref name=pmid18809061>{{Cite journal | last1 = Barkley | first1 = CR. | last2 = Ligibel | first2 = JA. | last3 = Wong | first3 = JS. | last4 = Lipsitz | first4 = S. | last5 = Smith | first5 = BL. | last6 = Golshan | first6 = M. | title = Mucinous breast carcinoma: a large contemporary series. | journal = Am J Surg | volume = 196 | issue = 4 | pages = 549-51 | month = Oct | year = 2008 | doi = 10.1016/j.amjsurg.2008.06.013 | PMID = 18809061 }}</ref> | ||
*Usually older women. | *Usually older women. | ||
| Line 50: | Line 52: | ||
*Malignant mucin producing glands. | *Malignant mucin producing glands. | ||
**Mucinous component must comprise >90% of the tumour - '''required for diagnosis'''.<ref name=pmid22006768>{{Cite journal | last1 = Dogan | first1 = E. | last2 = Aksoy | first2 = S. | last3 = Dizdar | first3 = O. | last4 = Arslan | first4 = C. | last5 = Dede | first5 = DS. | last6 = Ozisik | first6 = Y. | last7 = Altundag | first7 = K. | title = Pure mucinous carcinoma of the breast: a single center experience. | journal = J BUON | volume = 16 | issue = 3 | pages = 565-7 | month = | year = | doi = | PMID = 22006768 }}</ref> | **Mucinous component must comprise >90% of the tumour - '''required for diagnosis'''.<ref name=pmid22006768>{{Cite journal | last1 = Dogan | first1 = E. | last2 = Aksoy | first2 = S. | last3 = Dizdar | first3 = O. | last4 = Arslan | first4 = C. | last5 = Dede | first5 = DS. | last6 = Ozisik | first6 = Y. | last7 = Altundag | first7 = K. | title = Pure mucinous carcinoma of the breast: a single center experience. | journal = J BUON | volume = 16 | issue = 3 | pages = 565-7 | month = | year = | doi = | PMID = 22006768 }}</ref> | ||
** | **Small clusters of cells should float in the mucin - '''key feature'''. | ||
**Glands typically have irregular edges. | **Glands typically have irregular edges. | ||
**+/-Vessels within the mucin pools. | **+/-Vessels within the mucin pools. | ||
*Subtypes <ref>{{Cite journal | last1 = Weigelt | first1 = B. | last2 = Geyer | first2 = FC. | last3 = Horlings | first3 = HM. | last4 = Kreike | first4 = B. | last5 = Halfwerk | first5 = H. | last6 = Reis-Filho | first6 = JS. | title = Mucinous and neuroendocrine breast carcinomas are transcriptionally distinct from invasive ductal carcinomas of no special type. | journal = Mod Pathol | volume = 22 | issue = 11 | pages = 1401-14 | month = Nov | year = 2009 | doi = 10.1038/modpathol.2009.112 | PMID = 19633645 }}</ref> | |||
**Mucinous A (or paucicellular) - more mucin | |||
**Mucinous B (or hypercellular) - less mucin and neuroendocrine differentiation and argyrophilia | |||
DDx: | DDx: | ||
*[[DCIS]] with a mucinous component. | *[[DCIS]] with a mucinous component. | ||
**Mucin has a homogenous appearance, mucin lacks vascularization, mucin pools have a regular border. | **Mucin has a homogenous appearance, mucin lacks vascularization, mucin pools have a regular border. | ||
*[[Invasive ductal carcinoma of the breast]] with a mucinous component - more common than ''mucinous breast carcinoma''. | *[[Invasive ductal carcinoma of the breast]] with a mucinous component - more common than ''mucinous breast carcinoma''. Any 'no special type' component imparts a worse prognosis so the diagnosis 'mucinous carcinoma' is reserved for tumours with close to pure mucinous features. | ||
Note: | Note: | ||
*The amount of mucinous component to call ''[[mucinous carcinoma]]'' varies by anatomical site. | *The amount of mucinous component to call ''[[mucinous carcinoma]]'' varies by anatomical site. | ||
* | *A breast core biopsy that show any degree of mucinous change is an indication for excision to exclude mucinous carcinoma.<ref name=pmid12218567>{{Cite journal | last1 = Jacobs | first1 = TW. | last2 = Connolly | first2 = JL. | last3 = Schnitt | first3 = SJ. | title = Nonmalignant lesions in breast core needle biopsies: to excise or not to excise? | journal = Am J Surg Pathol | volume = 26 | issue = 9 | pages = 1095-110 | month = Sep | year = 2002 | doi = | PMID = 12218567 }}</ref> | ||
*Size and margins are assessed from edge of mucin, even if it does not contain epithelial cells | |||
*These tumors can be very difficult to assess lymphovascular invasion. Look for tumour cells in areas where lymphatics are expected ie. tumour in arc-shape around vascular bundle | |||
===Images=== | ===Images=== | ||
| Line 72: | Line 79: | ||
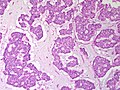
Image:Breast MucinousCarcinoma MP SNP.jpg|Mucinous Carcinoma - high power (SKB) | Image:Breast MucinousCarcinoma MP SNP.jpg|Mucinous Carcinoma - high power (SKB) | ||
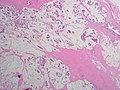
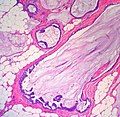
Image:Breast DCIS Mucinous Extravasation MP2 PA.JPG|Breast - Mucinous ductal carcinoma in situ with mucin extravasation - low power. Compare the profile of the involved gland to the examples above. (SKB) | Image:Breast DCIS Mucinous Extravasation MP2 PA.JPG|Breast - Mucinous ductal carcinoma in situ with mucin extravasation - low power. Compare the profile of the involved gland to the examples above. (SKB) | ||
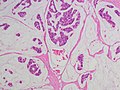
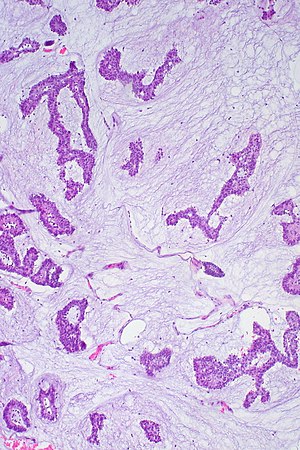
Image:Breast DCIS Mucinous Extravasation MP3 PA.JPG|Breast - Mucinous ductal carcinoma in situ with mucin extravasation - medium power. (SKB) | Image:Breast DCIS Mucinous Extravasation MP3 PA.JPG|Breast - Mucinous ductal carcinoma in situ with mucin extravasation - medium power. Notice the lack of floating tumour nests (SKB) | ||
</gallery> | </gallery> | ||
Latest revision as of 11:37, 8 September 2016
| Mucinous breast carcinoma | |
|---|---|
| Diagnosis in short | |
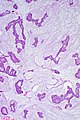
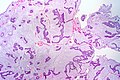
 Mucinous breast carcinoma. H&E stain. | |
|
| |
| LM | malignant mucin producing glands - where mucinous component must comprise >90% of the tumour, tumour cells should float in the mucin, glands typically have irregular edges, +/-vessels within the mucin pools |
| LM DDx | other type of breast cancer with a mucinous component (very common), other mucinous tumours |
| IHC | ER +ve, PR +ve, HER2 -ve |
| Gross | pale, glistening, jelly-like appearance |
| Grossing notes | breast grossing |
| Staging | breast cancer staging |
| Site | breast - see invasive breast cancer |
|
| |
| Prevalence | uncommon |
| Prognosis | good compared to the usual ductal carcinoma |
| Clin. DDx | other breast tumours |
Mucinous breast carcinoma is an uncommon form of breast cancer that has a good prognosis compared to the common invasive ductal carcinoma.
It is also known as mucinous carcinoma of the breast, and colloid carcinoma of the breast.
General
- Rare.
- 2% of invasive breast carcinomas.
- Good prognosis.[1]
- Usually older women.
Gross
- Pale, glistening, jelly-like appearance.
- Well-circumscribed.
Image:
Microscopic
Features:
- Malignant mucin producing glands.
- Mucinous component must comprise >90% of the tumour - required for diagnosis.[2]
- Small clusters of cells should float in the mucin - key feature.
- Glands typically have irregular edges.
- +/-Vessels within the mucin pools.
- Subtypes [3]
- Mucinous A (or paucicellular) - more mucin
- Mucinous B (or hypercellular) - less mucin and neuroendocrine differentiation and argyrophilia
DDx:
- DCIS with a mucinous component.
- Mucin has a homogenous appearance, mucin lacks vascularization, mucin pools have a regular border.
- Invasive ductal carcinoma of the breast with a mucinous component - more common than mucinous breast carcinoma. Any 'no special type' component imparts a worse prognosis so the diagnosis 'mucinous carcinoma' is reserved for tumours with close to pure mucinous features.
Note:
- The amount of mucinous component to call mucinous carcinoma varies by anatomical site.
- A breast core biopsy that show any degree of mucinous change is an indication for excision to exclude mucinous carcinoma.[4]
- Size and margins are assessed from edge of mucin, even if it does not contain epithelial cells
- These tumors can be very difficult to assess lymphovascular invasion. Look for tumour cells in areas where lymphatics are expected ie. tumour in arc-shape around vascular bundle
Images
IHC
- ER +ve.
- PR +ve.
- HER2 -ve.
See also
References
- ↑ Barkley, CR.; Ligibel, JA.; Wong, JS.; Lipsitz, S.; Smith, BL.; Golshan, M. (Oct 2008). "Mucinous breast carcinoma: a large contemporary series.". Am J Surg 196 (4): 549-51. doi:10.1016/j.amjsurg.2008.06.013. PMID 18809061.
- ↑ Dogan, E.; Aksoy, S.; Dizdar, O.; Arslan, C.; Dede, DS.; Ozisik, Y.; Altundag, K.. "Pure mucinous carcinoma of the breast: a single center experience.". J BUON 16 (3): 565-7. PMID 22006768.
- ↑ Weigelt, B.; Geyer, FC.; Horlings, HM.; Kreike, B.; Halfwerk, H.; Reis-Filho, JS. (Nov 2009). "Mucinous and neuroendocrine breast carcinomas are transcriptionally distinct from invasive ductal carcinomas of no special type.". Mod Pathol 22 (11): 1401-14. doi:10.1038/modpathol.2009.112. PMID 19633645.
- ↑ Jacobs, TW.; Connolly, JL.; Schnitt, SJ. (Sep 2002). "Nonmalignant lesions in breast core needle biopsies: to excise or not to excise?". Am J Surg Pathol 26 (9): 1095-110. PMID 12218567.