Difference between revisions of "Malignant peripheral nerve sheath tumour"
Jump to navigation
Jump to search
(→Images) |
Jensflorian (talk | contribs) (→IHC: update) |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = Malignant_peripheral_nerve_sheath_tumour_-_high_mag.jpg | | Image = Malignant_peripheral_nerve_sheath_tumour_-_high_mag.jpg | ||
| Width = | | Width = | ||
| Caption = MPNST. [[H&E stain]]. | | Caption = MPNST. [[H&E stain]]. | ||
| Line 30: | Line 30: | ||
'''Malignant peripheral nerve sheath tumour''', abbreviated '''MPNST''', is an uncommon malignant tumour of the nerve sheath. | '''Malignant peripheral nerve sheath tumour''', abbreviated '''MPNST''', is an uncommon malignant tumour of the nerve sheath. | ||
It is also known '''neurofibrosarcoma'''<ref name=pmid21317712>{{Cite journal | last1 = Mills | first1 = AM. | last2 = Karamchandani | first2 = JR. | last3 = Vogel | first3 = H. | last4 = Longacre | first4 = TA. | title = Endocervical fibroblastic malignant peripheral nerve sheath tumor (neurofibrosarcoma): report of a novel entity possibly related to endocervical CD34 fibrocytes. | journal = Am J Surg Pathol | volume = 35 | issue = 3 | pages = 404-12 | month = Mar | year = 2011 | doi = 10.1097/PAS.0b013e318208f72e | PMID = 21317712 }}</ref> | It is also known '''neurofibrosarcoma'''<ref name=pmid21317712>{{Cite journal | last1 = Mills | first1 = AM. | last2 = Karamchandani | first2 = JR. | last3 = Vogel | first3 = H. | last4 = Longacre | first4 = TA. | title = Endocervical fibroblastic malignant peripheral nerve sheath tumor (neurofibrosarcoma): report of a novel entity possibly related to endocervical CD34 fibrocytes. | journal = Am J Surg Pathol | volume = 35 | issue = 3 | pages = 404-12 | month = Mar | year = 2011 | doi = 10.1097/PAS.0b013e318208f72e | PMID = 21317712 }}</ref>, '''neurogenic sarcoma'''.<ref name=pmid23139572>{{Cite journal | last1 = Sham | first1 = ME. | last2 = Ghorpade | first2 = A. | last3 = Shetty | first3 = S. | last4 = Hari | first4 = . | last5 = Vinay | first5 = . | title = Malignant peripheral nerve cell tumour. | journal = J Maxillofac Oral Surg | volume = 9 | issue = 1 | pages = 68-71 | month = Mar | year = 2010 | doi = 10.1007/s12663-010-0019-6 | PMID = 23139572 }}</ref> and '''malignant schwannoma''' - these terms are however depreceated.<ref>{WHOCNS2007}</ref> | ||
==General== | ==General== | ||
*Malignant - as the name implies. | *Malignant - as the name implies. | ||
*Usually assoc. with a peripheral nerve.{ | *Usually assoc. with a peripheral nerve.<ref>{WHOCNS2007}</ref> | ||
*May be seen in the context of [[neurofibromatosis type 1]]. | *May be seen in the context of [[neurofibromatosis type 1]] or radiation induced.<ref>{{Cite journal | last1 = Ducatman | first1 = BS. | last2 = Scheithauer | first2 = BW. | last3 = Piepgras | first3 = DG. | last4 = Reiman | first4 = HM. | last5 = Ilstrup | first5 = DM. | title = Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. | journal = Cancer | volume = 57 | issue = 10 | pages = 2006-21 | month = May | year = 1986 | doi = | PMID = 3082508 }}</ref> | ||
*Approx 50-70% arise from (mostly plexiform) [[neurofibroma]]s. | |||
*Usu. adults | |||
*Approx. 5% of all malignant soft tissue lesions. | |||
<gallery> | |||
File:MPNST.PNG | MPNST in a NF1 case (WC/Filip em). | |||
File:MPNST Pathology gross.jpg | MPNST gross pathology (Flickr/drbloodmoney). | |||
</gallery> | |||
==Microscopic== | ==Microscopic== | ||
Features: | Features:<ref>{{Cite journal | last1 = Pekmezci | first1 = M. | last2 = Reuss | first2 = DE. | last3 = Hirbe | first3 = AC. | last4 = Dahiya | first4 = S. | last5 = Gutmann | first5 = DH. | last6 = von Deimling | first6 = A. | last7 = Horvai | first7 = AE. | last8 = Perry | first8 = A. | title = Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas. | journal = Mod Pathol | volume = 28 | issue = 2 | pages = 187-200 | month = Feb | year = 2015 | doi = 10.1038/modpathol.2014.109 | PMID = 25189642 }}</ref> | ||
*Cellular - usu. spindle cells. | *Cellular - usu. spindle cells. | ||
**Very rarely epithelioid.<ref name=pmid22082606>{{Cite journal | last1 = Carter | first1 = JM. | last2 = O'Hara | first2 = C. | last3 = Dundas | first3 = G. | last4 = Gilchrist | first4 = D. | last5 = Collins | first5 = MS. | last6 = Eaton | first6 = K. | last7 = Judkins | first7 = AR. | last8 = Biegel | first8 = JA. | last9 = Folpe | first9 = AL. | title = Epithelioid malignant peripheral nerve sheath tumor arising in a schwannoma, in a patient with neuroblastoma-like schwannomatosis and a novel germline SMARCB1 mutation. | journal = Am J Surg Pathol | volume = 36 | issue = 1 | pages = 154-60 | month = Jan | year = 2012 | doi = 10.1097/PAS.0b013e3182380802 | PMID = 22082606 }}</ref> | **Very rarely epithelioid.<ref name=pmid22082606>{{Cite journal | last1 = Carter | first1 = JM. | last2 = O'Hara | first2 = C. | last3 = Dundas | first3 = G. | last4 = Gilchrist | first4 = D. | last5 = Collins | first5 = MS. | last6 = Eaton | first6 = K. | last7 = Judkins | first7 = AR. | last8 = Biegel | first8 = JA. | last9 = Folpe | first9 = AL. | title = Epithelioid malignant peripheral nerve sheath tumor arising in a schwannoma, in a patient with neuroblastoma-like schwannomatosis and a novel germline SMARCB1 mutation. | journal = Am J Surg Pathol | volume = 36 | issue = 1 | pages = 154-60 | month = Jan | year = 2012 | doi = 10.1097/PAS.0b013e3182380802 | PMID = 22082606 }}</ref> | ||
| Line 44: | Line 52: | ||
*Mitoses. | *Mitoses. | ||
*+/-Herring bone pattern. | *+/-Herring bone pattern. | ||
*Perivascular hypercellularity. | |||
*Tumor herniation into vascular lumens. | |||
*"Pseudocapsule" with tumour invasion of adjacent tissue. | |||
Notes: | Notes: | ||
| Line 52: | Line 63: | ||
*Plexiform schwannoma. | *Plexiform schwannoma. | ||
*[[Malignant triton tumour]]. | *[[Malignant triton tumour]]. | ||
**aka. MPNST with mesenchymal differentiation. | |||
DDx of herring bone: | DDx of herring bone: | ||
| Line 63: | Line 75: | ||
Image:Malignant_peripheral_nerve_sheath_tumour_-_high_mag.jpg | MPNST - high mag. (WC) | Image:Malignant_peripheral_nerve_sheath_tumour_-_high_mag.jpg | MPNST - high mag. (WC) | ||
Image:Malignant_peripheral_nerve_sheath_tumour_-_very_high_mag.jpg | MPNST - very high mag. (WC) | Image:Malignant_peripheral_nerve_sheath_tumour_-_very_high_mag.jpg | MPNST - very high mag. (WC) | ||
File:MPNST chondroid differentiation.jpg | MPNST with chondroid dedifferentiation (Triton tumor). (WC) | |||
</gallery> | </gallery> | ||
www: | www: | ||
| Line 69: | Line 82: | ||
===Grading=== | ===Grading=== | ||
*Can be graded histologically,<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref> and this is prognostic.<ref name=pmid16923196>{{cite journal |author=Kar M, Deo SV, Shukla NK, ''et al.'' |title=Malignant peripheral nerve sheath tumors (MPNST)--clinicopathological study and treatment outcome of twenty-four cases |journal=World J Surg Oncol |volume=4 |issue= |pages=55 |year=2006 |pmid=16923196 |pmc=1560134 |doi=10.1186/1477-7819-4-55 |url=}}</ref> | *Can be graded histologically, according WHO<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref> and this is prognostic.<ref name=pmid16923196>{{cite journal |author=Kar M, Deo SV, Shukla NK, ''et al.'' |title=Malignant peripheral nerve sheath tumors (MPNST)--clinicopathological study and treatment outcome of twenty-four cases |journal=World J Surg Oncol |volume=4 |issue= |pages=55 |year=2006 |pmid=16923196 |pmc=1560134 |doi=10.1186/1477-7819-4-55 |url=}}</ref> | ||
*grade IV: Presence of necrosis (3/4 of all MPNST). | |||
*grade III: Mitotic count exceeds 4/1 HPF. | |||
*grade II: nuclear size (<3x of neurofibroma cell), hyperchromatic nuclei. | |||
**overlap with cellular ("atypical") neurofibroma (DDx). | |||
Sarcoma grading system<ref name=pmid6693192>{{cite journal |author=Trojani M, Contesso G, Coindre JM, ''et al.'' |title=Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system |journal=Int. J. Cancer |volume=33 |issue=1 |pages=37–42 |year=1984 |month=January |pmid=6693192 |doi= |url=}}</ref> - based on: | Sarcoma grading system<ref name=pmid6693192>{{cite journal |author=Trojani M, Contesso G, Coindre JM, ''et al.'' |title=Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system |journal=Int. J. Cancer |volume=33 |issue=1 |pages=37–42 |year=1984 |month=January |pmid=6693192 |doi= |url=}}</ref> - based on: | ||
| Line 80: | Line 98: | ||
*S-100 +ve ~ 30% of tumours. | *S-100 +ve ~ 30% of tumours. | ||
*SOX10 +ve ~ 50% of tumours. | *SOX10 +ve ~ 50% of tumours. | ||
*Neurofibromin (NFC) -ve (88% in NF1, 43% sporadic MPNST)<ref>{{Cite journal | last1 = Reuss | first1 = DE. | last2 = Habel | first2 = A. | last3 = Hagenlocher | first3 = C. | last4 = Mucha | first4 = J. | last5 = Ackermann | first5 = U. | last6 = Tessmer | first6 = C. | last7 = Meyer | first7 = J. | last8 = Capper | first8 = D. | last9 = Moldenhauer | first9 = G. | title = Neurofibromin specific antibody differentiates malignant peripheral nerve sheath tumors (MPNST) from other spindle cell neoplasms. | journal = Acta Neuropathol | volume = 127 | issue = 4 | pages = 565-72 | month = Apr | year = 2014 | doi = 10.1007/s00401-014-1246-6 | PMID = 24464231 }}</ref> | |||
*H3K27me -ve<ref>{{Cite journal | last1 = Schaefer | first1 = IM. | last2 = Fletcher | first2 = CD. | last3 = Hornick | first3 = JL. | title = Loss of H3K27 trimethylation distinguishes malignant peripheral nerve sheath tumors from histologic mimics. | journal = Mod Pathol | volume = 29 | issue = 1 | pages = 4-13 | month = Jan | year = 2016 | doi = 10.1038/modpathol.2015.134 | PMID = 26585554 }}</ref> | |||
*MIB-1 ≥20% is highly predictive of malignant peripheral nerve sheath tumor (87% sensitivity and 96% specificity).<ref>{{Cite journal | last1 = Pekmezci | first1 = M. | last2 = Reuss | first2 = DE. | last3 = Hirbe | first3 = AC. | last4 = Dahiya | first4 = S. | last5 = Gutmann | first5 = DH. | last6 = von Deimling | first6 = A. | last7 = Horvai | first7 = AE. | last8 = Perry | first8 = A. | title = Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas. | journal = Mod Pathol | volume = 28 | issue = 2 | pages = 187-200 | month = Feb | year = 2015 | doi = 10.1038/modpathol.2014.109 | PMID = 25189642 }}</ref> | |||
Others:<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref> | Others:<ref name=pmid14508395>{{cite journal |author=Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH |title=Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions |journal=Am. J. Surg. Pathol. |volume=27 |issue=10 |pages=1337–45 |year=2003 |month=October |pmid=14508395 |doi= |url=}}</ref> | ||
*p53. | *p53. | ||
*p16. | *p16 -ve.<ref>{{Cite journal | last1 = Pekmezci | first1 = M. | last2 = Reuss | first2 = DE. | last3 = Hirbe | first3 = AC. | last4 = Dahiya | first4 = S. | last5 = Gutmann | first5 = DH. | last6 = von Deimling | first6 = A. | last7 = Horvai | first7 = AE. | last8 = Perry | first8 = A. | title = Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas. | journal = Mod Pathol | volume = 28 | issue = 2 | pages = 187-200 | month = Feb | year = 2015 | doi = 10.1038/modpathol.2014.109 | PMID = 25189642 }}</ref> | ||
*p27. | *p27. | ||
* | *p75NTR +ve (80%). | ||
*EGFR +ve <ref> {{Cite journal | last1 = Pekmezci | first1 = M. | last2 = Reuss | first2 = DE. | last3 = Hirbe | first3 = AC. | last4 = Dahiya | first4 = S. | last5 = Gutmann | first5 = DH. | last6 = von Deimling | first6 = A. | last7 = Horvai | first7 = AE. | last8 = Perry | first8 = A. | title = Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas. | journal = Mod Pathol | volume = 28 | issue = 2 | pages = 187-200 | month = Feb | year = 2015 | doi = 10.1038/modpathol.2014.109 | PMID = 25189642 }}</ref> | |||
==Molecular== | |||
Features:<ref>{{Cite journal | last1 = Röhrich | first1 = M. | last2 = Koelsche | first2 = C. | last3 = Schrimpf | first3 = D. | last4 = Capper | first4 = D. | last5 = Sahm | first5 = F. | last6 = Kratz | first6 = A. | last7 = Reuss | first7 = J. | last8 = Hovestadt | first8 = V. | last9 = Jones | first9 = DT. | title = Methylation-based classification of benign and malignant peripheral nerve sheath tumors. | journal = Acta Neuropathol | volume = | issue = | pages = | month = Feb | year = 2016 | doi = 10.1007/s00401-016-1540-6 | PMID = 26857854 }}</ref><ref>{{Cite journal | last1 = Hirbe | first1 = AC. | last2 = Dahiya | first2 = S. | last3 = Miller | first3 = CA. | last4 = Li | first4 = T. | last5 = Fulton | first5 = RS. | last6 = Zhang | first6 = X. | last7 = McDonald | first7 = S. | last8 = DeSchryver | first8 = K. | last9 = Duncavage | first9 = EJ. | title = Whole Exome Sequencing Reveals the Order of Genetic Changes during Malignant Transformation and Metastasis in a Single Patient with NF1-plexiform Neurofibroma. | journal = Clin Cancer Res | volume = 21 | issue = 18 | pages = 4201-11 | month = Sep | year = 2015 | doi = 10.1158/1078-0432.CCR-14-3049 | PMID = 25925892 }}</ref> | |||
* Atypical neurofibromas and low-grade MPNST have a common methylation profile and frequent losses of CDKN2A. | |||
* A subset of MPNST show loss of trimethylation of histone H3 at lysine 27 (H3K27me3). | |||
* P53 and beta-spectrin mutations during progression reported. | |||
==See also== | ==See also== | ||
*[[Peripheral nerve sheath tumours]]. | *[[Peripheral nerve sheath tumours]]. | ||
Latest revision as of 09:28, 27 April 2017
| Malignant peripheral nerve sheath tumour | |
|---|---|
| Diagnosis in short | |
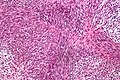
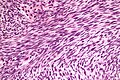
 MPNST. H&E stain. | |
|
| |
| LM | spindle cell lesion (or very rarely epithelioid lesion) with nuclear atypia, mitotic activity, +/-herring bone pattern |
| Subtypes | malignant triton tumour |
| LM DDx | synovial sarcoma, fibrosarcoma, cellular schwannoma, plexiform schwannoma |
| Site | soft tissue |
|
| |
| Associated Dx | neurofibroma, plexiform neurofibroma |
| Syndromes | neurofibromatosis type 1 |
|
| |
| Signs | mass |
| Prognosis | poor |
Malignant peripheral nerve sheath tumour, abbreviated MPNST, is an uncommon malignant tumour of the nerve sheath.
It is also known neurofibrosarcoma[1], neurogenic sarcoma.[2] and malignant schwannoma - these terms are however depreceated.[3]
General
- Malignant - as the name implies.
- Usually assoc. with a peripheral nerve.[4]
- May be seen in the context of neurofibromatosis type 1 or radiation induced.[5]
- Approx 50-70% arise from (mostly plexiform) neurofibromas.
- Usu. adults
- Approx. 5% of all malignant soft tissue lesions.
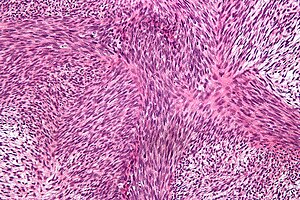
Microscopic
Features:[6]
- Cellular - usu. spindle cells.
- Very rarely epithelioid.[7]
- Nuclear atypia.
- Mitoses.
- +/-Herring bone pattern.
- Perivascular hypercellularity.
- Tumor herniation into vascular lumens.
- "Pseudocapsule" with tumour invasion of adjacent tissue.
Notes:
- May be diagnosed in a poorly diff. tumour if patient has NF1.
DDx:
- Cellular schwannoma.
- Plexiform schwannoma.
- Malignant triton tumour.
- aka. MPNST with mesenchymal differentiation.
DDx of herring bone:
- MPNST.
- Synovial sarcoma.
- Fibrosarcoma.
Images
www:
Grading
- Can be graded histologically, according WHO[8] and this is prognostic.[9]
- grade IV: Presence of necrosis (3/4 of all MPNST).
- grade III: Mitotic count exceeds 4/1 HPF.
- grade II: nuclear size (<3x of neurofibroma cell), hyperchromatic nuclei.
- overlap with cellular ("atypical") neurofibroma (DDx).
Sarcoma grading system[10] - based on:
- Tumour differentiation.
- Mitotic rate.
- Necrosis.
IHC
Features:[11]
- S-100 +ve ~ 30% of tumours.
- SOX10 +ve ~ 50% of tumours.
- Neurofibromin (NFC) -ve (88% in NF1, 43% sporadic MPNST)[12]
- H3K27me -ve[13]
- MIB-1 ≥20% is highly predictive of malignant peripheral nerve sheath tumor (87% sensitivity and 96% specificity).[14]
Others:[8]
Molecular
- Atypical neurofibromas and low-grade MPNST have a common methylation profile and frequent losses of CDKN2A.
- A subset of MPNST show loss of trimethylation of histone H3 at lysine 27 (H3K27me3).
- P53 and beta-spectrin mutations during progression reported.
See also
References
- ↑ Mills, AM.; Karamchandani, JR.; Vogel, H.; Longacre, TA. (Mar 2011). "Endocervical fibroblastic malignant peripheral nerve sheath tumor (neurofibrosarcoma): report of a novel entity possibly related to endocervical CD34 fibrocytes.". Am J Surg Pathol 35 (3): 404-12. doi:10.1097/PAS.0b013e318208f72e. PMID 21317712.
- ↑ Sham, ME.; Ghorpade, A.; Shetty, S.; Hari, .; Vinay, . (Mar 2010). "Malignant peripheral nerve cell tumour.". J Maxillofac Oral Surg 9 (1): 68-71. doi:10.1007/s12663-010-0019-6. PMID 23139572.
- ↑ {WHOCNS2007}
- ↑ {WHOCNS2007}
- ↑ Ducatman, BS.; Scheithauer, BW.; Piepgras, DG.; Reiman, HM.; Ilstrup, DM. (May 1986). "Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases.". Cancer 57 (10): 2006-21. PMID 3082508.
- ↑ Pekmezci, M.; Reuss, DE.; Hirbe, AC.; Dahiya, S.; Gutmann, DH.; von Deimling, A.; Horvai, AE.; Perry, A. (Feb 2015). "Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas.". Mod Pathol 28 (2): 187-200. doi:10.1038/modpathol.2014.109. PMID 25189642.
- ↑ Carter, JM.; O'Hara, C.; Dundas, G.; Gilchrist, D.; Collins, MS.; Eaton, K.; Judkins, AR.; Biegel, JA. et al. (Jan 2012). "Epithelioid malignant peripheral nerve sheath tumor arising in a schwannoma, in a patient with neuroblastoma-like schwannomatosis and a novel germline SMARCB1 mutation.". Am J Surg Pathol 36 (1): 154-60. doi:10.1097/PAS.0b013e3182380802. PMID 22082606.
- ↑ 8.0 8.1 Zhou H, Coffin CM, Perkins SL, Tripp SR, Liew M, Viskochil DH (October 2003). "Malignant peripheral nerve sheath tumor: a comparison of grade, immunophenotype, and cell cycle/growth activation marker expression in sporadic and neurofibromatosis 1-related lesions". Am. J. Surg. Pathol. 27 (10): 1337–45. PMID 14508395.
- ↑ Kar M, Deo SV, Shukla NK, et al. (2006). "Malignant peripheral nerve sheath tumors (MPNST)--clinicopathological study and treatment outcome of twenty-four cases". World J Surg Oncol 4: 55. doi:10.1186/1477-7819-4-55. PMC 1560134. PMID 16923196. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560134/.
- ↑ Trojani M, Contesso G, Coindre JM, et al. (January 1984). "Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system". Int. J. Cancer 33 (1): 37–42. PMID 6693192.
- ↑ Nonaka D, Chiriboga L, Rubin BP (September 2008). "Sox10: a pan-schwannian and melanocytic marker". Am. J. Surg. Pathol. 32 (9): 1291–8. doi:10.1097/PAS.0b013e3181658c14. PMID 18636017.
- ↑ Reuss, DE.; Habel, A.; Hagenlocher, C.; Mucha, J.; Ackermann, U.; Tessmer, C.; Meyer, J.; Capper, D. et al. (Apr 2014). "Neurofibromin specific antibody differentiates malignant peripheral nerve sheath tumors (MPNST) from other spindle cell neoplasms.". Acta Neuropathol 127 (4): 565-72. doi:10.1007/s00401-014-1246-6. PMID 24464231.
- ↑ Schaefer, IM.; Fletcher, CD.; Hornick, JL. (Jan 2016). "Loss of H3K27 trimethylation distinguishes malignant peripheral nerve sheath tumors from histologic mimics.". Mod Pathol 29 (1): 4-13. doi:10.1038/modpathol.2015.134. PMID 26585554.
- ↑ Pekmezci, M.; Reuss, DE.; Hirbe, AC.; Dahiya, S.; Gutmann, DH.; von Deimling, A.; Horvai, AE.; Perry, A. (Feb 2015). "Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas.". Mod Pathol 28 (2): 187-200. doi:10.1038/modpathol.2014.109. PMID 25189642.
- ↑ Pekmezci, M.; Reuss, DE.; Hirbe, AC.; Dahiya, S.; Gutmann, DH.; von Deimling, A.; Horvai, AE.; Perry, A. (Feb 2015). "Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas.". Mod Pathol 28 (2): 187-200. doi:10.1038/modpathol.2014.109. PMID 25189642.
- ↑ Pekmezci, M.; Reuss, DE.; Hirbe, AC.; Dahiya, S.; Gutmann, DH.; von Deimling, A.; Horvai, AE.; Perry, A. (Feb 2015). "Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas.". Mod Pathol 28 (2): 187-200. doi:10.1038/modpathol.2014.109. PMID 25189642.
- ↑ Röhrich, M.; Koelsche, C.; Schrimpf, D.; Capper, D.; Sahm, F.; Kratz, A.; Reuss, J.; Hovestadt, V. et al. (Feb 2016). "Methylation-based classification of benign and malignant peripheral nerve sheath tumors.". Acta Neuropathol. doi:10.1007/s00401-016-1540-6. PMID 26857854.
- ↑ Hirbe, AC.; Dahiya, S.; Miller, CA.; Li, T.; Fulton, RS.; Zhang, X.; McDonald, S.; DeSchryver, K. et al. (Sep 2015). "Whole Exome Sequencing Reveals the Order of Genetic Changes during Malignant Transformation and Metastasis in a Single Patient with NF1-plexiform Neurofibroma.". Clin Cancer Res 21 (18): 4201-11. doi:10.1158/1078-0432.CCR-14-3049. PMID 25925892.