Difference between revisions of "Lymphovascular invasion"
Jump to navigation
Jump to search
(expand) |
|||
| (35 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
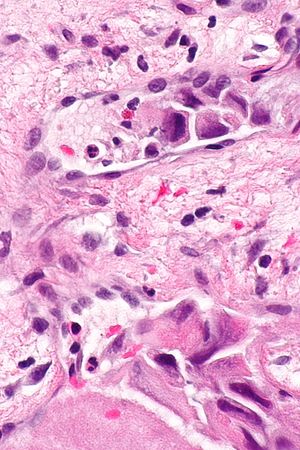
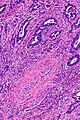
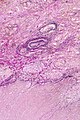
[[Image:Laryngeal squamous carcinoma - LVI -- very high mag.jpg|thumb|right|Lymphovascular invasion in a case of [[laryngeal cancer]]. [[H&E stain]].]] | |||
'''Lymphovascular invasion''', also '''lymphovascular space invasion''', is (non-hematologic) malignant cells within [[blood vessels]] and/or lymphatics. It is abbreviated '''LVI'''. | '''Lymphovascular invasion''', also '''lymphovascular space invasion''', is (non-hematologic) malignant cells within [[blood vessels]] and/or lymphatics. It is abbreviated '''LVI'''. | ||
The term ''lymphovascular invasion'' is preferred to ''[[vascular invasion]]'', as it is very difficult to differentiate morphologically small lymphatics and small vascular spaces, without [[immunohistochemistry]]. | |||
'' | |||
==General== | |||
*LVI, in the [[TNM staging system]], does '''not''' affect tumour stage; however, there are exceptions. | |||
**Exceptions: | |||
***[[Seminoma]]. | |||
***[[Squamous cell carcinoma of the penis]]. | |||
***Intrahepatic bile duct carcinoma ([[cholangiocarcinoma]]).<ref>URL: [http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/IntrahepBileDucts_12protocol_3101.pdf http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/IntrahepBileDucts_12protocol_3101.pdf]. Accessed on: 23 May 2013.</ref> | |||
***[[Hepatocellular carcinoma]].<ref>URL: [http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Hepatocellular_11protocol.pdf http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Hepatocellular_11protocol.pdf]. Accessed on: 6 April 2012.</ref> | |||
*Absence of LVI in the context of proven [[lymph node metastasis]] = sampling error.<ref name=pmid21545433>{{Cite journal | last1 = Han | first1 = JS. | last2 = Molberg | first2 = KH. | last3 = Sarode | first3 = V. | title = Predictors of invasion and axillary lymph node metastasis in patients with a core biopsy diagnosis of ductal carcinoma in situ: an analysis of 255 cases. | journal = Breast J | volume = 17 | issue = 3 | pages = 223-9 | month = | year = | doi = 10.1111/j.1524-4741.2011.01069.x | PMID = 21545433 }}</ref> | |||
*The prognostic significance of LVI, generally, is dependent on the tumour type and may depend on the tumour stage and lymph node status. | |||
**Most generally -- LVI = poorer prognosis.<ref name=pmid10101593>{{Cite journal | last1 = Moreira | first1 = LF. | last2 = Kenmotsu | first2 = M. | last3 = Gochi | first3 = A. | last4 = Tanaka | first4 = N. | last5 = Orita | first5 = K. | title = Lymphovascular and neural invasion in low-lying rectal carcinoma. | journal = Cancer Detect Prev | volume = 23 | issue = 2 | pages = 123-8 | month = | year = 1999 | doi = | PMID = 10101593 }}</ref> | |||
===Specific tumours and LVI=== | |||
{| class="wikitable sortable" | |||
!Tumour | |||
!Prognosis | |||
!Comment | |||
|- | |||
| [[Urothelial carcinoma]] | |||
| independent predictor of a poor prognosis in bladder tumours | |||
| LVI has more predictive power than [[tumour stage]] in the [[urinary bladder]];<ref name=pmid19494855>{{Cite journal | last1 = Cheng | first1 = L. | last2 = Montironi | first2 = R. | last3 = Davidson | first3 = DD. | last4 = Lopez-Beltran | first4 = A. | title = Staging and reporting of urothelial carcinoma of the urinary bladder. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S70-95 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.1 | PMID = 19494855 | URL = http://www.nature.com/modpathol/journal/v22/n2s/full/modpathol20091a.html }}</ref> appears to be less important in upper urinary tract disease<ref name=pmid24954108>{{Cite journal | last1 = Kim | first1 = HS. | last2 = Kim | first2 = M. | last3 = Jeong | first3 = CW. | last4 = Kwak | first4 = C. | last5 = Kim | first5 = HH. | last6 = Ku | first6 = JH. | title = Presence of lymphovascular invasion in urothelial bladder cancer specimens after transurethral resections correlates with risk of upstaging and survival: A systematic review and meta-analysis. | journal = Urol Oncol | volume = | issue = | pages = | month = Jun | year = 2014 | doi = 10.1016/j.urolonc.2014.05.008 | PMID = 24954108 }}</ref> | |||
|- | |||
| [[Breast cancer]] | |||
| not an independent predictor<ref name=pmid19436035>{{Cite journal | last1 = Ejlertsen | first1 = B. | last2 = Jensen | first2 = MB. | last3 = Rank | first3 = F. | last4 = Rasmussen | first4 = BB. | last5 = Christiansen | first5 = P. | last6 = Kroman | first6 = N. | last7 = Kvistgaard | first7 = ME. | last8 = Overgaard | first8 = M. | last9 = Toftdahl | first9 = DB. | title = Population-based study of peritumoral lymphovascular invasion and outcome among patients with operable breast cancer. | journal = J Natl Cancer Inst | volume = 101 | issue = 10 | pages = 729-35 | month = May | year = 2009 | doi = 10.1093/jnci/djp090 | PMID = 19436035 }}</ref> | |||
| | |||
|- | |||
| [[Colorectal carcinoma]] | |||
| independent predictor of poorer prognosis (sporadic cancers)<ref name=pmid20305435>{{Cite journal | last1 = Lim | first1 = SB. | last2 = Yu | first2 = CS. | last3 = Jang | first3 = SJ. | last4 = Kim | first4 = TW. | last5 = Kim | first5 = JH. | last6 = Kim | first6 = JC. | title = Prognostic significance of lymphovascular invasion in sporadic colorectal cancer. | journal = Dis Colon Rectum | volume = 53 | issue = 4 | pages = 377-84 | month = Apr | year = 2010 | doi = 10.1007/DCR.0b013e3181cf8ae5 | PMID = 20305435 }}</ref> | |||
| may be used as a [[quality]] measure; 25% of cases should have vascular invasion<ref>{{Cite journal | last1 = Messenger | first1 = DE. | last2 = Driman | first2 = DK. | last3 = Riddell | first3 = R. | last4 = McLeod | first4 = R. | last5 = Kirsch | first5 = R. | title = Is Venous Invasion in Colorectal Cancer an Under-Reported Finding | |||
among Canadian Pathologists? Results of a Population-Based Survey | |||
of Ontario Pathologists. | journal = Can J Pathol | volume = 2 | issue = 4 | pages = 46-9 | month = | year = 2012 | doi = | PMID = | url = http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/ }} </ref> | |||
|- | |||
|} | |||
==Microscopic== | ==Microscopic== | ||
| Line 18: | Line 52: | ||
Notes: | Notes: | ||
*Criteria for LVI vary by the site/tumour. | *Criteria for LVI vary by the site/tumour. | ||
**In some sites, the first criterium isn't required. | **In some sites, the first criterium (tumour cells outside of the tumour proper) isn't required. | ||
===Images=== | |||
<gallery> | |||
Image:Merkel_cell_carcinoma_-_high_mag.jpg | Small focus of LVI in a [[merkel cell carcinoma]]. (WC/Nephron) | |||
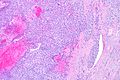
Image: Seminoma LVI -- low mag.jpg | [[LVI]] - low mag. (WC/Nephron) | |||
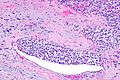
Image: Seminoma LVI -- intermed mag.jpg | LVI - intermed. mag. (WC/Nephron) | |||
</gallery> | |||
<gallery> | |||
Image: CRC with LVI - HE -- very low mag.jpg | [[colorectal carcinoma|CRC]] with LVI - very low mag. (WC/Nephron) | |||
Image: CRC with LVI - HE -- low mag.jpg | CRC with LVI - low mag. (WC/Nephron) | |||
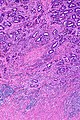
Image: CRC with LVI - HE -- intermed mag.jpg | CRC with LVI - intermed. mag. (WC/Nephron) | |||
Image: CRC with LVI - HE - alt -- high mag.jpg | CRC with LVI - high mag. (WC/Nephron) | |||
Image: CRC with LVI - HE -- very high mag.jpg | CRC with LVI - very high mag. (WC/Nephron) | |||
</gallery> | |||
==Stains== | ==Stains== | ||
*[[Movat stain]] - especially useful in [[ | *[[Movat stain]] - especially useful in [[colorectal carcinoma]] so one can readily identify [[blood vessel]]s.<ref name=pmid19861561>{{Cite journal | last1 = Howlett | first1 = CJ. | last2 = Tweedie | first2 = EJ. | last3 = Driman | first3 = DK. | title = Use of an elastic stain to show venous invasion in colorectal carcinoma: a simple technique for detection of an important prognostic factor. | journal = J Clin Pathol | volume = 62 | issue = 11 | pages = 1021-5 | month = Nov | year = 2009 | doi = 10.1136/jcp.2009.065615 | PMID = 19861561 }}</ref> | ||
*Elastin stain. | |||
===Images=== | |||
<gallery> | |||
Image: CRC with LVI - elastin -- very low mag.jpg | [[colorectal carcinoma|CRC]] with LVI - elastin - very low mag. (WC/Nephron) | |||
Image: CRC with LVI - elastin -- low mag.jpg | CRC with LVI - elastin - low mag. (WC/Nephron) | |||
Image: CRC with LVI - elastin -- intermed mag.jpg | CRC with LVI - elastin - intermed. mag. (WC/Nephron) | |||
Image: CRC with LVI - elastin - alt -- high mag.jpg | CRC with LVI - elastin - high mag. (WC/Nephron) | |||
Image: CRC with LVI - elastin -- very high mag.jpg | CRC with LVI - elastin - very high mag. (WC/Nephron) | |||
</gallery> | |||
==IHC== | ==IHC== | ||
| Line 29: | Line 86: | ||
Markers with high specific to lymphatic spaces: | Markers with high specific to lymphatic spaces: | ||
*D2-40. | *[[D2-40]]. | ||
==See also== | ==See also== | ||
*[[Cancer]]. | *[[Cancer]]. | ||
*[[Intravascular lymphoma]]. | |||
*[[Perineural invasion]]. | |||
*[[Angioinvasion]]. | |||
*[[MELF]]. | |||
==References== | ==References== | ||
Latest revision as of 15:58, 5 March 2020
Lymphovascular invasion, also lymphovascular space invasion, is (non-hematologic) malignant cells within blood vessels and/or lymphatics. It is abbreviated LVI.
The term lymphovascular invasion is preferred to vascular invasion, as it is very difficult to differentiate morphologically small lymphatics and small vascular spaces, without immunohistochemistry.
General
- LVI, in the TNM staging system, does not affect tumour stage; however, there are exceptions.
- Exceptions:
- Seminoma.
- Squamous cell carcinoma of the penis.
- Intrahepatic bile duct carcinoma (cholangiocarcinoma).[1]
- Hepatocellular carcinoma.[2]
- Exceptions:
- Absence of LVI in the context of proven lymph node metastasis = sampling error.[3]
- The prognostic significance of LVI, generally, is dependent on the tumour type and may depend on the tumour stage and lymph node status.
- Most generally -- LVI = poorer prognosis.[4]
Specific tumours and LVI
| Tumour | Prognosis | Comment |
|---|---|---|
| Urothelial carcinoma | independent predictor of a poor prognosis in bladder tumours | LVI has more predictive power than tumour stage in the urinary bladder;[5] appears to be less important in upper urinary tract disease[6] |
| Breast cancer | not an independent predictor[7] | |
| Colorectal carcinoma | independent predictor of poorer prognosis (sporadic cancers)[8] | may be used as a quality measure; 25% of cases should have vascular invasion[9] |
Microscopic
Rosen criteria for LVI (in the breast):[10][11]
- Must be outside of the tumour proper.
- LVI is usually very close -- typically within 0.1 cm.
- Contour of cells should differ from possible vessel wall.
- DCIS with retraction artifact mimicing LVI has a contour that matches its surrounding fibrous tissue.
- Endothelium (usu. flat) should be visible.
- Lymphatics are found adjacent to blood vessels - vessels should be present in the vicinity.
Memory device LUBE-O:
- LVI has a Unique contour, Blood vessels and Endothelium in the vicinity, and is Outside of the tumour.
Notes:
- Criteria for LVI vary by the site/tumour.
- In some sites, the first criterium (tumour cells outside of the tumour proper) isn't required.
Images
Small focus of LVI in a merkel cell carcinoma. (WC/Nephron)
LVI - low mag. (WC/Nephron)
CRC with LVI - very low mag. (WC/Nephron)
Stains
- Movat stain - especially useful in colorectal carcinoma so one can readily identify blood vessels.[12]
- Elastin stain.
Images
CRC with LVI - elastin - very low mag. (WC/Nephron)
IHC
Vascular markers:
- CD31.
- CD34.
Markers with high specific to lymphatic spaces:
See also
References
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/IntrahepBileDucts_12protocol_3101.pdf. Accessed on: 23 May 2013.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Hepatocellular_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ Han, JS.; Molberg, KH.; Sarode, V.. "Predictors of invasion and axillary lymph node metastasis in patients with a core biopsy diagnosis of ductal carcinoma in situ: an analysis of 255 cases.". Breast J 17 (3): 223-9. doi:10.1111/j.1524-4741.2011.01069.x. PMID 21545433.
- ↑ Moreira, LF.; Kenmotsu, M.; Gochi, A.; Tanaka, N.; Orita, K. (1999). "Lymphovascular and neural invasion in low-lying rectal carcinoma.". Cancer Detect Prev 23 (2): 123-8. PMID 10101593.
- ↑ Cheng, L.; Montironi, R.; Davidson, DD.; Lopez-Beltran, A. (Jun 2009). "Staging and reporting of urothelial carcinoma of the urinary bladder.". Mod Pathol 22 Suppl 2: S70-95. doi:10.1038/modpathol.2009.1. PMID 19494855.
- ↑ Kim, HS.; Kim, M.; Jeong, CW.; Kwak, C.; Kim, HH.; Ku, JH. (Jun 2014). "Presence of lymphovascular invasion in urothelial bladder cancer specimens after transurethral resections correlates with risk of upstaging and survival: A systematic review and meta-analysis.". Urol Oncol. doi:10.1016/j.urolonc.2014.05.008. PMID 24954108.
- ↑ Ejlertsen, B.; Jensen, MB.; Rank, F.; Rasmussen, BB.; Christiansen, P.; Kroman, N.; Kvistgaard, ME.; Overgaard, M. et al. (May 2009). "Population-based study of peritumoral lymphovascular invasion and outcome among patients with operable breast cancer.". J Natl Cancer Inst 101 (10): 729-35. doi:10.1093/jnci/djp090. PMID 19436035.
- ↑ Lim, SB.; Yu, CS.; Jang, SJ.; Kim, TW.; Kim, JH.; Kim, JC. (Apr 2010). "Prognostic significance of lymphovascular invasion in sporadic colorectal cancer.". Dis Colon Rectum 53 (4): 377-84. doi:10.1007/DCR.0b013e3181cf8ae5. PMID 20305435.
- ↑ Messenger, DE.; Driman, DK.; Riddell, R.; McLeod, R.; Kirsch, R. (2012). [http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/ "Is Venous Invasion in Colorectal Cancer an Under-Reported Finding among Canadian Pathologists? Results of a Population-Based Survey of Ontario Pathologists."]. Can J Pathol 2 (4): 46-9. http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/.
- ↑ Rosen, PP. (1983). "Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance.". Pathol Annu 18 Pt 2: 215-32. PMID 6674861.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2009/InvasiveBreast_09protocol.pdf. Accessed on: 5 August 2011.
- ↑ Howlett, CJ.; Tweedie, EJ.; Driman, DK. (Nov 2009). "Use of an elastic stain to show venous invasion in colorectal carcinoma: a simple technique for detection of an important prognostic factor.". J Clin Pathol 62 (11): 1021-5. doi:10.1136/jcp.2009.065615. PMID 19861561.