Difference between revisions of "Lymphovascular invasion"
Jump to navigation
Jump to search
(→Images) |
|||
| Line 73: | Line 73: | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
Image: CRC with LVI - elastin -- very low mag.jpg | CRC with LVI - elastin - very low mag. (WC/Nephron) | Image: CRC with LVI - elastin -- very low mag.jpg | [[colorectal carcinoma|CRC]] with LVI - elastin - very low mag. (WC/Nephron) | ||
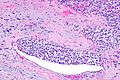
Image: CRC with LVI - elastin -- low mag.jpg | CRC with LVI - elastin - low mag. (WC/Nephron) | Image: CRC with LVI - elastin -- low mag.jpg | CRC with LVI - elastin - low mag. (WC/Nephron) | ||
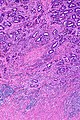
Image: CRC with LVI - elastin -- intermed mag.jpg | CRC with LVI - elastin - intermed. mag. (WC/Nephron) | Image: CRC with LVI - elastin -- intermed mag.jpg | CRC with LVI - elastin - intermed. mag. (WC/Nephron) | ||
Revision as of 00:13, 24 March 2019
Lymphovascular invasion, also lymphovascular space invasion, is (non-hematologic) malignant cells within blood vessels and/or lymphatics. It is abbreviated LVI.
The term lymphovascular invasion is preferred to vascular invasion, as it is very difficult to differentiate morphologically small lymphatics and small vascular spaces, without immunohistochemistry.
General
- LVI, in the TNM staging system, does not affect tumour stage; however, there are exceptions.
- Exceptions:
- Seminoma.
- Squamous cell carcinoma of the penis.
- Intrahepatic bile duct carcinoma (cholangiocarcinoma).[1]
- Hepatocellular carcinoma.[2]
- Exceptions:
- Absence of LVI in the context of proven lymph node metastasis = sampling error.[3]
- The prognostic significance of LVI, generally, is dependent on the tumour type and may depend on the tumour stage and lymph node status.
- Most generally -- LVI = poorer prognosis.[4]
Specific tumours and LVI
| Tumour | Prognosis | Comment |
|---|---|---|
| Urothelial carcinoma | independent predictor of a poor prognosis in bladder tumours | LVI has more predictive power than tumour stage in the urinary bladder;[5] appears to be less important in upper urinary tract disease[6] |
| Breast cancer | not an independent predictor[7] | |
| Colorectal carcinoma | independent predictor of poorer prognosis (sporadic cancers)[8] | may be used as a quality measure; 25% of cases should have vascular invasion[9] |
Microscopic
Rosen criteria for LVI (in the breast):[10][11]
- Must be outside of the tumour proper.
- LVI is usually very close -- typically within 0.1 cm.
- Contour of cells should differ from possible vessel wall.
- DCIS with retraction artifact mimicing LVI has a contour that matches its surrounding fibrous tissue.
- Endothelium (usu. flat) should be visible.
- Lymphatics are found adjacent to blood vessels - vessels should be present in the vicinity.
Memory device LUBE-O:
- LVI has a Unique contour, Blood vessels and Endothelium in the vicinity, and is Outside of the tumour.
Notes:
- Criteria for LVI vary by the site/tumour.
- In some sites, the first criterium (tumour cells outside of the tumour proper) isn't required.
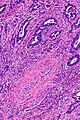
Images
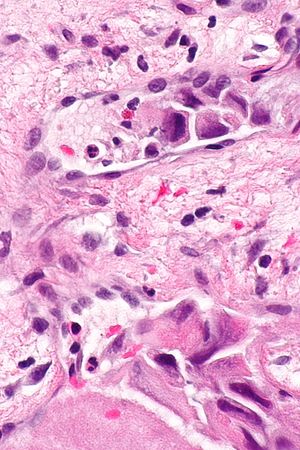
Small focus of LVI in a merkel cell carcinoma. (WC/Nephron)
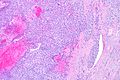
LVI - low mag. (WC/Nephron)
CRC with LVI - very low mag. (WC/Nephron)
Stains
- Movat stain - especially useful in colorectal carcinoma so one can readily identify blood vessels.[12]
- Elastin stain.
Images
CRC with LVI - elastin - very low mag. (WC/Nephron)
IHC
Vascular markers:
- CD31.
- CD34.
Markers with high specific to lymphatic spaces:
See also
References
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/IntrahepBileDucts_12protocol_3101.pdf. Accessed on: 23 May 2013.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Hepatocellular_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ Han, JS.; Molberg, KH.; Sarode, V.. "Predictors of invasion and axillary lymph node metastasis in patients with a core biopsy diagnosis of ductal carcinoma in situ: an analysis of 255 cases.". Breast J 17 (3): 223-9. doi:10.1111/j.1524-4741.2011.01069.x. PMID 21545433.
- ↑ Moreira, LF.; Kenmotsu, M.; Gochi, A.; Tanaka, N.; Orita, K. (1999). "Lymphovascular and neural invasion in low-lying rectal carcinoma.". Cancer Detect Prev 23 (2): 123-8. PMID 10101593.
- ↑ Cheng, L.; Montironi, R.; Davidson, DD.; Lopez-Beltran, A. (Jun 2009). "Staging and reporting of urothelial carcinoma of the urinary bladder.". Mod Pathol 22 Suppl 2: S70-95. doi:10.1038/modpathol.2009.1. PMID 19494855.
- ↑ Kim, HS.; Kim, M.; Jeong, CW.; Kwak, C.; Kim, HH.; Ku, JH. (Jun 2014). "Presence of lymphovascular invasion in urothelial bladder cancer specimens after transurethral resections correlates with risk of upstaging and survival: A systematic review and meta-analysis.". Urol Oncol. doi:10.1016/j.urolonc.2014.05.008. PMID 24954108.
- ↑ Ejlertsen, B.; Jensen, MB.; Rank, F.; Rasmussen, BB.; Christiansen, P.; Kroman, N.; Kvistgaard, ME.; Overgaard, M. et al. (May 2009). "Population-based study of peritumoral lymphovascular invasion and outcome among patients with operable breast cancer.". J Natl Cancer Inst 101 (10): 729-35. doi:10.1093/jnci/djp090. PMID 19436035.
- ↑ Lim, SB.; Yu, CS.; Jang, SJ.; Kim, TW.; Kim, JH.; Kim, JC. (Apr 2010). "Prognostic significance of lymphovascular invasion in sporadic colorectal cancer.". Dis Colon Rectum 53 (4): 377-84. doi:10.1007/DCR.0b013e3181cf8ae5. PMID 20305435.
- ↑ Messenger, DE.; Driman, DK.; Riddell, R.; McLeod, R.; Kirsch, R. (2012). [http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/ "Is Venous Invasion in Colorectal Cancer an Under-Reported Finding among Canadian Pathologists? Results of a Population-Based Survey of Ontario Pathologists."]. Can J Pathol 2 (4): 46-9. http://www.allegrahamilton.com/publications/ajp/cjp/p4_2/.
- ↑ Rosen, PP. (1983). "Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance.". Pathol Annu 18 Pt 2: 215-32. PMID 6674861.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2009/InvasiveBreast_09protocol.pdf. Accessed on: 5 August 2011.
- ↑ Howlett, CJ.; Tweedie, EJ.; Driman, DK. (Nov 2009). "Use of an elastic stain to show venous invasion in colorectal carcinoma: a simple technique for detection of an important prognostic factor.". J Clin Pathol 62 (11): 1021-5. doi:10.1136/jcp.2009.065615. PMID 19861561.