Difference between revisions of "Lymphangioleiomyomatosis"
Jump to navigation
Jump to search
(+cat.) |
|||
| (18 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Lymphangioleiomyomatosis - intermed mag.jpg | |||
| Width = | |||
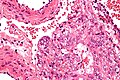
| Caption = Lymphangioleiomyomatosis. [[H&E stain]]. | |||
| Synonyms = lymphangiomyomatosis | |||
| Micro = spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei, cyst formation, thick arterial walls | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = | |||
| IHC = HMB-45 +ve, ER +ve, PR +ve, SMA +ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[lung]] - see ''[[medical lung diseases]]'' | |||
| Assdx = | |||
| Syndromes = [[tuberous sclerosis]] | |||
| Clinicalhx = almost always women of childbearing age, recurrent [[pneumothorax]] | |||
| Signs = | |||
| Symptoms = dyspnea | |||
| Prevalence = very rare | |||
| Bloodwork = | |||
| Rads = bullae/thin walled cysts distributed in all lung fields, lymphadenopathy | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = [[eosinophilic granuloma]], [[usual interstitial pneumonia]], [[emphysema]] | |||
| Tx = medical therapy, lung transplantation | |||
}} | |||
'''Lymphangioleiomyomatosis''', abbreviated '''LAM''', is a rare [[medical lung disease|lung pathology]] that predominantly afflicits women of childbearing age. | |||
It is also known as '''lymphangiomyomatosis'''. | |||
==General== | |||
*Clinical: [[dyspnea]], recurrent [[pneumothorax]]. | |||
*May be an indication for lung transplantation. | |||
*Non-neoplastic muscle proliferation versus tumour that can metastasize.<ref name=pmid20235883>{{Cite journal | last1 = Taveira-DaSilva | first1 = AM. | last2 = Pacheco-Rodriguez | first2 = G. | last3 = Moss | first3 = J. | title = The natural history of lymphangioleiomyomatosis: markers of severity, rate of progression and prognosis. | journal = Lymphat Res Biol | volume = 8 | issue = 1 | pages = 9-19 | month = Mar | year = 2010 | doi = 10.1089/lrb.2009.0024 | PMID = 20235883 }}</ref> | |||
**It has been hypothesized that LAM represent a non-malignant [[metastasis]] of a renal [[angiomyolipoma]].<ref name=pmid17003820/> | |||
Notes: | |||
*Considered to be a [[PEComa]]. | |||
Clinical DDx:<ref>{{Cite journal | last1 = Xu | first1 = KF. | last2 = Lo | first2 = BH. | title = Lymphangioleiomyomatosis: differential diagnosis and optimal management. | journal = Ther Clin Risk Manag | volume = 10 | issue = | pages = 691-700 | month = | year = 2014 | doi = 10.2147/TCRM.S50784 | PMID = 25187723 }}</ref> | |||
*[[Pulmonary Langerhans cell histiocytosis]]. | |||
*[[Lymphocytic interstitial pneumonia]] (LIP). | |||
*[[Pulmonary amyloidosis]]. | |||
*[[Birt–Hogg–Dubé syndrome]]. | |||
Treatment:<ref name=pmid25478388>{{Cite journal | last1 = Vlachostergios | first1 = PJ. | last2 = Rad | first2 = BS. | last3 = Karimi | first3 = K. | last4 = Apergis | first4 = G. | title = Angiomyolipomas, Renal Cell Carcinomas and Pulmonary Lymphangioleiomyomatosis. | journal = J Clin Diagn Res | volume = 8 | issue = 10 | pages = MJ01 | month = Oct | year = 2014 | doi = 10.7860/JCDR/2014/9733.5021 | PMID = 25478388 }}</ref> | |||
*Bronchodilators - symptomatic treatment. | |||
*mTOR inhibitors. (???) | |||
*Transplantation. | |||
===Epidemiology=== | |||
*Rare. | |||
*Usually affects women - primarily in childbearing years. | |||
**Case reports of LAM in men - usu. with [[TSC]].<ref name=pmid17431222>{{Cite journal | last1 = Schiavina | first1 = M. | last2 = Di Scioscio | first2 = V. | last3 = Contini | first3 = P. | last4 = Cavazza | first4 = A. | last5 = Fabiani | first5 = A. | last6 = Barberis | first6 = M. | last7 = Bini | first7 = A. | last8 = Altimari | first8 = A. | last9 = Cooke | first9 = RM. | title = Pulmonary lymphangioleiomyomatosis in a karyotypically normal man without tuberous sclerosis complex. | journal = Am J Respir Crit Care Med | volume = 176 | issue = 1 | pages = 96-8 | month = Jul | year = 2007 | doi = 10.1164/rccm.200610-1408CR | PMID = 17431222 }}</ref> | |||
*Associated with [[angiomyolipoma]]s. | |||
**Seen in ~30% of sporadic cases, and in ~90% of cases with tuberous sclerosis.<ref name=pmid17003820/> | |||
*Associated with [[tuberous sclerosis]] - esp. TSC2 mutations. | |||
**In the context of [[tuberous sclerosis]], [[angiomyolipoma]] of the kidney often preceeds LAM.<ref name=pmid17003820>{{cite journal |author=Rakowski SK, Winterkorn EB, Paul E, Steele DJ, Halpern EF, Thiele EA |title=Renal manifestations of tuberous sclerosis complex: Incidence, prognosis, and predictive factors |journal=Kidney Int. |volume=70 |issue=10 |pages=1777–82 |year=2006 |month=November |pmid=17003820 |doi=10.1038/sj.ki.5001853 |url=}}</ref> | |||
==Gross/Radiology== | |||
*Bullae/thin walled cysts - distributed in all lung fields. | |||
*Lymphadenopathy. | |||
Radiologic DDx (of cysts): | |||
*[[Eosinophilic granuloma]] - associated with [[smoking]]. | |||
*[[Usual interstitial pneumonia]] (UIP). | |||
*[[Emphysema]]. | |||
==Microscopic== | |||
Features:<ref>[http://emedicine.medscape.com/article/299545-diagnosis http://emedicine.medscape.com/article/299545-diagnosis]</ref> | |||
*Spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei. | |||
*Cyst formation. | |||
*Thick arterial walls. | |||
===Images=== | |||
<gallery> | |||
Image:Lymphangioleiomyomatosis - very low mag.jpg| LAM - very low mag. (WC) | |||
Image:Lymphangioleiomyomatosis - low mag.jpg| LAM - low mag. (WC) | |||
Image:Lymphangioleiomyomatosis - intermed mag.jpg| LAM - intermed. mag. (WC) | |||
Image:Lymphangioleiomyomatosis - very high mag.jpg| LAM - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://www.nature.com/modpathol/journal/v19/n6/fig_tab/3800610f3.html LAM (nature.com)]. | |||
*[http://path.upmc.edu/cases/case111.html LAM - several images (upmc.edu)]. | |||
==IHC== | |||
*HMB-45 +ve. | |||
*ER +ve. | |||
*PR +ve. | |||
*SMA +ve. | |||
==See also== | |||
*[[Medical lung diseases]]. | |||
*[[PEComa]]. | |||
*[[Multifocal micronodular pneumocyte hyperplasia associated with tuberous sclerosis]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Medical lung diseases]] | |||
Latest revision as of 02:07, 8 March 2016
| Lymphangioleiomyomatosis | |
|---|---|
| Diagnosis in short | |
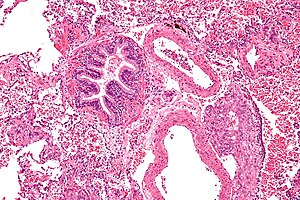 Lymphangioleiomyomatosis. H&E stain. | |
|
| |
| Synonyms | lymphangiomyomatosis |
|
| |
| LM | spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei, cyst formation, thick arterial walls |
| IHC | HMB-45 +ve, ER +ve, PR +ve, SMA +ve |
| Site | lung - see medical lung diseases |
|
| |
| Syndromes | tuberous sclerosis |
|
| |
| Clinical history | almost always women of childbearing age, recurrent pneumothorax |
| Symptoms | dyspnea |
| Prevalence | very rare |
| Radiology | bullae/thin walled cysts distributed in all lung fields, lymphadenopathy |
| Clin. DDx | eosinophilic granuloma, usual interstitial pneumonia, emphysema |
| Treatment | medical therapy, lung transplantation |
Lymphangioleiomyomatosis, abbreviated LAM, is a rare lung pathology that predominantly afflicits women of childbearing age.
It is also known as lymphangiomyomatosis.
General
- Clinical: dyspnea, recurrent pneumothorax.
- May be an indication for lung transplantation.
- Non-neoplastic muscle proliferation versus tumour that can metastasize.[1]
- It has been hypothesized that LAM represent a non-malignant metastasis of a renal angiomyolipoma.[2]
Notes:
- Considered to be a PEComa.
Clinical DDx:[3]
- Pulmonary Langerhans cell histiocytosis.
- Lymphocytic interstitial pneumonia (LIP).
- Pulmonary amyloidosis.
- Birt–Hogg–Dubé syndrome.
Treatment:[4]
- Bronchodilators - symptomatic treatment.
- mTOR inhibitors. (???)
- Transplantation.
Epidemiology
- Rare.
- Usually affects women - primarily in childbearing years.
- Associated with angiomyolipomas.
- Seen in ~30% of sporadic cases, and in ~90% of cases with tuberous sclerosis.[2]
- Associated with tuberous sclerosis - esp. TSC2 mutations.
- In the context of tuberous sclerosis, angiomyolipoma of the kidney often preceeds LAM.[2]
Gross/Radiology
- Bullae/thin walled cysts - distributed in all lung fields.
- Lymphadenopathy.
Radiologic DDx (of cysts):
- Eosinophilic granuloma - associated with smoking.
- Usual interstitial pneumonia (UIP).
- Emphysema.
Microscopic
Features:[6]
- Spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei.
- Cyst formation.
- Thick arterial walls.
Images
www:
IHC
- HMB-45 +ve.
- ER +ve.
- PR +ve.
- SMA +ve.
See also
- Medical lung diseases.
- PEComa.
- Multifocal micronodular pneumocyte hyperplasia associated with tuberous sclerosis.
References
- ↑ Taveira-DaSilva, AM.; Pacheco-Rodriguez, G.; Moss, J. (Mar 2010). "The natural history of lymphangioleiomyomatosis: markers of severity, rate of progression and prognosis.". Lymphat Res Biol 8 (1): 9-19. doi:10.1089/lrb.2009.0024. PMID 20235883.
- ↑ 2.0 2.1 2.2 Rakowski SK, Winterkorn EB, Paul E, Steele DJ, Halpern EF, Thiele EA (November 2006). "Renal manifestations of tuberous sclerosis complex: Incidence, prognosis, and predictive factors". Kidney Int. 70 (10): 1777–82. doi:10.1038/sj.ki.5001853. PMID 17003820.
- ↑ Xu, KF.; Lo, BH. (2014). "Lymphangioleiomyomatosis: differential diagnosis and optimal management.". Ther Clin Risk Manag 10: 691-700. doi:10.2147/TCRM.S50784. PMID 25187723.
- ↑ Vlachostergios, PJ.; Rad, BS.; Karimi, K.; Apergis, G. (Oct 2014). "Angiomyolipomas, Renal Cell Carcinomas and Pulmonary Lymphangioleiomyomatosis.". J Clin Diagn Res 8 (10): MJ01. doi:10.7860/JCDR/2014/9733.5021. PMID 25478388.
- ↑ Schiavina, M.; Di Scioscio, V.; Contini, P.; Cavazza, A.; Fabiani, A.; Barberis, M.; Bini, A.; Altimari, A. et al. (Jul 2007). "Pulmonary lymphangioleiomyomatosis in a karyotypically normal man without tuberous sclerosis complex.". Am J Respir Crit Care Med 176 (1): 96-8. doi:10.1164/rccm.200610-1408CR. PMID 17431222.
- ↑ http://emedicine.medscape.com/article/299545-diagnosis