Hyperplastic polyp
The hyperplastic polyp of the colon and rectum is a very common. It is commonly abbreviated HP.
| Hyperplastic polyp | |
|---|---|
| Diagnosis in short | |
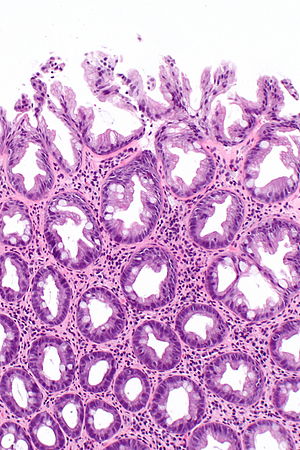 Hyperplastic polyp. H&E stain. | |
|
| |
| LM | serrated architecture at the surface without glandular abnormalities |
| Subtypes | microvesicular serrated polyps (MVSPs), goblet cell serrated polyps (GCSPs) |
| LM DDx | sessile serrated adenoma, normal colon, other gastrointestinal polyps |
| Gross | usually rectum or sigmoid, typically < 5mm |
| Site | cecum, colon, rectum |
|
| |
| Syndromes | serrated polyposis syndrome |
|
| |
| Symptoms | asymptomatic |
| Prevalence | very common |
| Endoscopy | pedunculated or sessile |
| Prognosis | good |
| Clin. DDx | normal colon, sessile serrated adenoma |
| Hyperplastic polyp | |
|---|---|
| External resources | |
| EHVSC | 10190 |
- The stomach lesion is dealt with in hyperplastic polyp of the stomach.
General
- Most common type of polyp:
- Approximately 90% of all colonic polyps.[1]
- May be part of serrated polyposis syndrome (previously known as hyperplastic polyposis syndrome).[2]
Gross
Features:[3]
- Flat lesion, usually <= 5mm.
- Typically in the distal large bowel (rectum, sigmoid colon).
Microscopic
Features:[1]
- Irregular crypt architecture - tortuosity.
- Serrated epithelial cells (at the surface of the gland) - only colorectal polyps - key feature.
- Serrated appearance = saw-tooth appearance, epithelium has jagged edge.
Notes:
- Significant negatives:
- No nuclear atypia; glands darker staining deep... lighter staining luminal.
- In the colon goblet cells should be present (as is usual).
- Inflammation -- cryptitis or even crypt abscesses -- is considered to arise due to trauma.[citation needed]
- It is usually not reported.
DDx:
- Sessile serrated adenoma.
- Normal colon.
- Xanthomatous polyp with hyperplastic features.[4]
Images
www:
Subclassification
- Usually not subclassified as there is no demonstrated prognostic significance;[2] the subtyping is an academic exercise.
HPs may be subclassified into two groups:[2]
- Microvesicular serrated polyps (MVSPs).
- Goblet cell serrated polyps (GCSPs).
Features of the HP subtypes:[2]
| Subtype | Histology | Mutations | Clinical relevance |
| Microvesicular | microvesicles at the surface, serration at the surface to the mid portion of glands |
BRAF V600E, CIMP | possible sessile serrated adenoma precursor |
| Goblet cell | superficial goblet cells, serration at the surface |
KRAS | unknown; probably benign |
Notes:
- CIMP = CpG island methylation phenotype.
IHC
- Chromogranin A increased scattered Chromogranin A-positive cells (in relation to normal colorectal mucosa).
- Sessile serrated adenoma is completely negative for Chromogranin A.
Sign out
POLYP, RECTUM, POLYPECTOMY: - HYPERPLASTIC POLYP.
POLYP, SIGMOID COLON, POLYPECTOMY: - HYPERPLASTIC POLYP.
POLYP, DESCENDING COLON, POLYPECTOMY: - HYPERPLASTIC POLYP.
POLYP, TRANSVERSE COLON, POLYPECTOMY: - HYPERPLASTIC POLYP.
COLONIC POLYP, 35 CM, POLYPECTOMY: - HYPERPLASTIC POLYP.
POLYP, LARGE BOWEL AT 10 CM, EXCISION: - HYPERPLASTIC POLYP.
Numerous hyperplastic polyps
COLONIC POLYP(S), POLYPECTOMY: - HYPERPLASTIC POLYP, SEE COMMENT. COMMENT: Eight pieces of tissue were received. On microscopy eight pieces of tissue are identified and all eight (individually) have the diagnostic features of a hyperplastic polyp. If these fragments all represent individual polyps and more polyps of this type are present in the individual, it raises the possibility of a serrated polyposis syndrome.
Superficial changes only
TRANSVERSE COLON (POLYP), BIOPSY: - COLORECTAL-TYPE MUCOSA WITH SURFACE HYPERPLASTIC CHANGE. - NEGATIVE FOR DYSPLASIA.
Micro
Goblet cell type
The sections show colonic-type mucosa with superficial serrations rich in goblet cells. There are no serrations in the crypt base and there is no crypt base dilation. No dysplasia is present.
Generic
The sections show colonic-type mucosa with superficial serrations. There are no serrations in the crypt base and there is no crypt base dilation. No dysplasia is present.
Alternate
The sections show two tissue fragments of colorectal-type mucosa. One fragment has no pathologic change. The second fragment has the changes of a hyperplastic polyp (superficial serrations, no serrations in the crypt base, no crypt base dilation).
Minimal crypt base dilation
The sections show colonic-type mucosa with superficial serrations. Rare serrations are seen focally near the crypt base. Rare mild crypt base dilation is seen. No hockey stick-shaped glands are identified. No crypt branching is seen. No dysplasia is present.
See also
References
- ↑ 1.0 1.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 858. ISBN 0-7216-0187-1.
- ↑ 2.0 2.1 2.2 2.3 Huang, CS.; Farraye, FA.; Yang, S.; O'Brien, MJ. (Feb 2011). "The clinical significance of serrated polyps.". Am J Gastroenterol 106 (2): 229-40; quiz 241. doi:10.1038/ajg.2010.429. PMID 21045813.
- ↑ Rex, DK.; Ahnen, DJ.; Baron, JA.; Batts, KP.; Burke, CA.; Burt, RW.; Goldblum, JR.; Guillem, JG. et al. (Sep 2012). "Serrated lesions of the colorectum: review and recommendations from an expert panel.". Am J Gastroenterol 107 (9): 1315-29; quiz 1314, 1330. doi:10.1038/ajg.2012.161. PMID 22710576.
- ↑ Nakasono, M.; Hirokawa, M.; Muguruma, N.; Okahisa, T.; Okamura, S.; Ito, S.; Miyamoto, H.; Wada, S. et al. (Jan 2004). "Colorectal xanthomas with polypoid lesion: report of 25 cases.". APMIS 112 (1): 3-10. PMID 14961968.