Ganglioglioma
| Ganglioglioma | |
|---|---|
| Diagnosis in short | |
| LM DDx | piloid gliosis, pilocytic astrocytoma, DNT |
| Stains | PAS-D +ve (eosinophilic granular bodies) |
| IHC | GFAP +ve, Synapto +ve |
| Gross | usually temporal +/-cystic |
| Site | brain - usu. supratentorial |
|
| |
| Syndromes | associated with epilepsy |
|
| |
| Prevalence | rare - esp. in children |
| Prognosis | good (WHO Grade I) |
- Not to be confused with ganglioneuroma.
General
- Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1).
- Anaplastic ganglioglioma: Grade III (ICD-O: 9505/3)
- Rare (approx. 0.5% of all CNS tumors).
- Usu. temporal lobe.
- Predominantly children (mean age: 9 years).
- Recognized as a cause of epilepsy.[1]
- Favourable prognosis (survival rates up to 97%)
- Insufficient data für anaplastic ganglioglioma.
Imaging
- Well-defined, T2-hyperintense.
- Strong CM enhancement.
- May contain cysts.
- Associated with midline structures.
Gross
- Circumscribed lesion.
- Usu. contrast enhancing.
- Solid, but intracortical cysts may be present.
- Little mass effect.
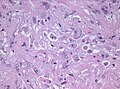
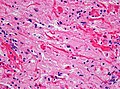
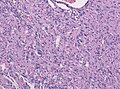
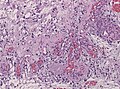
Microscopic
Features:[2]
- Classically biphasic (though either may be absent):
- Fibrillar.
- Microcystic/loose.
- Hair-like fibres ~ 1 micrometer; pilo- = hair.[3]
- Best seen on smear or with GFAP IHC.
- Rosenthal fibres - key feature.
- May be rare. Not pathognomonic (see below).
- Eosinophilic granular bodies.
- Low cellularity - when compared to medulloblastoma and ependymoma.
Notes:
- +/-Microvascular proliferation.
- +/-Focal necrosis.
- Necrosis with pseudopalisading more likely glioblastoma.
- +/-Mitoses - not significant in the context of the Dx.
DDx (of Rosenthal fibers):[4]
- Chronic reactive gliosis.
- Subependymoma.
- Pilocytic astrocytoma.
- Ganglioglioma.
DDx of pilocystic astrocytoma (brief):
- Piloid gliosis (esp. in sellar lesions).
- Oligodendroglioma.
- Glioblastoma (uncommon - but important).
- Tanycytic Ependymoma
- Pilocytic tumor components may be found in Ganglioglioma, DNET, RGNT
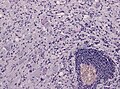
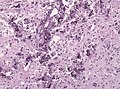
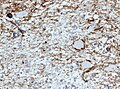
Images
Smears
Sections
www:
- Rosenthal fibre (ouhsc.edu).
- Pilocytic astrocytoma (upmc.edu).
- Pilocytic astrocytoma - another case (upmc.edu).
- Pilocytic astrocytoma - pennies on a plate (upmc.edu).[5]
- Pilocytic astrocytoma (upmc.edu).
Stains
- PAS-D: eosinophilic granular bodies +ve.
IHC
Features:[6]
- GFAP +ve (fibres).
- CD68: may have a significant macrophage component.
- KI-67: may be "high" (~20% ???).
- Olig 2: Usually strongly present.[7]
- IDH1 (R132H) -ve.
- H3F3A (K27M) -ve.
Molecular
- Almost all alteration associated with the MAPK pathway.[8]
- KIAA1549-BRAF fusion transcripts most common in sporadic PA (up to 2/3 of all cases).
- DDx: Fusion reported in rare Diffuse Leptomeingeal Glioneuronal Tumors and Oligodendroglioma.
- Rarely BRAF, KRAS or FGFR1 mutations, NTRK2, SRGAP3-RAF1 or FAM131B-BRAF fusions.[9][10]
- Up to 15% of all NF1 patients develop a PA ("optic glioma" as predilection).[11]
- Rare reports of PA in Noonan-Syndrome (PTPN11 mutation).[12]
Prognosis
- Excellent (10-year OS: 90%)
- In thalamic/chiasmatic region not so good (incomplete resection, often Pilomyxoid astrocytoma).
- Primary treatment: surgery. Incomplete resection: RT has to be considered.
- Chx is given in rare cases that are still progredient[13]
See also
References
- ↑ Im, SH.; Chung, CK.; Cho, BK.; Lee, SK. (Mar 2002). "Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome.". J Neurooncol 57 (1): 59-66. PMID 12125968.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 82-4. ISBN 978-0443069826.
- ↑ URL: http://dictionary.reference.com/browse/pilo-. Accessed on: 24 November 2010.
- ↑ Munoz D. 9 Mar 2009.
- ↑ URL: http://path.upmc.edu/cases/case195.html. Accessed on: 8 January 2012.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 84. ISBN 978-0443069826.
- ↑ Otero, JJ.; Rowitch, D.; Vandenberg, S. (Sep 2011). "OLIG2 is differentially expressed in pediatric astrocytic and in ependymal neoplasms.". J Neurooncol 104 (2): 423-38. doi:10.1007/s11060-010-0509-x. PMID 21193945.
- ↑ Collins, VP.; Jones, DT.; Giannini, C. (Jun 2015). "Pilocytic astrocytoma: pathology, molecular mechanisms and markers.". Acta Neuropathol 129 (6): 775-88. doi:10.1007/s00401-015-1410-7. PMID 25792358.
- ↑ Jones, DT.; Hutter, B.; Jäger, N.; Korshunov, A.; Kool, M.; Warnatz, HJ.; Zichner, T.; Lambert, SR. et al. (Aug 2013). "Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma.". Nat Genet 45 (8): 927-32. doi:10.1038/ng.2682. PMID 23817572.
- ↑ Cin, H.; Meyer, C.; Herr, R.; Janzarik, WG.; Lambert, S.; Jones, DT.; Jacob, K.; Benner, A. et al. (Jun 2011). "Oncogenic FAM131B-BRAF fusion resulting from 7q34 deletion comprises an alternative mechanism of MAPK pathway activation in pilocytic astrocytoma.". Acta Neuropathol 121 (6): 763-74. doi:10.1007/s00401-011-0817-z. PMID 21424530.
- ↑ Friedrich, RE.; Nuding, MA. (Aug 2016). "Optic Pathway Glioma and Cerebral Focal Abnormal Signal Intensity in Patients with Neurofibromatosis Type 1: Characteristics, Treatment Choices and Follow-up in 134 Affected Individuals and a Brief Review of the Literature.". Anticancer Res 36 (8): 4095-121. PMID 27466519.
- ↑ Jones, DT.; Hutter, B.; Jäger, N.; Korshunov, A.; Kool, M.; Warnatz, HJ.; Zichner, T.; Lambert, SR. et al. (Aug 2013). "Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma.". Nat Genet 45 (8): 927-32. doi:10.1038/ng.2682. PMID 23817572.
- ↑ Metts, RD.; Bartynski, W.; Welsh, CT.; Kinsman, S.; Bredlau, AL. (Mar 2017). "Bevacizumab Therapy for Pilomyxoid Astrocytoma.". J Pediatr Hematol Oncol. doi:10.1097/MPH.0000000000000824. PMID 28338567.