Difference between revisions of "Ganglioglioma"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (created, not finished!) |
Jensflorian (talk | contribs) (→Molecular: wikilink) |
||
| (17 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Anaplastic ganglioglioma HE.jpg | ||
| Width = | | Width = | ||
| Caption = | | Caption = | ||
| Line 30: | Line 30: | ||
| Tx = | | Tx = | ||
}} | }} | ||
Ganglioglioma is a epilepsy-associated glioneuronal tumour with benign course. '''Not''' to be confused with ''[[ganglioneuroma]]''. | |||
====General==== | ====General==== | ||
*Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1). | *Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1). | ||
| Line 39: | Line 40: | ||
*Recognized as a cause of [[epilepsy]].<ref name=pmid12125968>{{Cite journal | last1 = Im | first1 = SH. | last2 = Chung | first2 = CK. | last3 = Cho | first3 = BK. | last4 = Lee | first4 = SK. | title = Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome. | journal = J Neurooncol | volume = 57 | issue = 1 | pages = 59-66 | month = Mar | year = 2002 | doi = | PMID = 12125968 }}</ref> | *Recognized as a cause of [[epilepsy]].<ref name=pmid12125968>{{Cite journal | last1 = Im | first1 = SH. | last2 = Chung | first2 = CK. | last3 = Cho | first3 = BK. | last4 = Lee | first4 = SK. | title = Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome. | journal = J Neurooncol | volume = 57 | issue = 1 | pages = 59-66 | month = Mar | year = 2002 | doi = | PMID = 12125968 }}</ref> | ||
*Favourable prognosis (survival rates up to 97%) | *Favourable prognosis (survival rates up to 97%) | ||
** | **Anaplastic ganglioglioma have a recurrence risk of 69%-100% and median OS: 27months<ref>{{Cite journal | last1 = Terrier | first1 = LM. | last2 = Bauchet | first2 = L. | last3 = Rigau | first3 = V. | last4 = Amelot | first4 = A. | last5 = Zouaoui | first5 = S. | last6 = Filipiak | first6 = I. | last7 = Caille | first7 = A. | last8 = Almairac | first8 = F. | last9 = Aubriot-Lorton | first9 = MH. | title = Natural course and prognosis of anaplastic gangliogliomas: a multicenter retrospective study of 43 cases from the French Brain Tumor Database. | journal = Neuro Oncol | volume = 19 | issue = 5 | pages = 678-688 | month = 05 | year = 2017 | doi = 10.1093/neuonc/now186 | PMID = 28453747 }}</ref><ref>{{Cite journal | last1 = Zanello | first1 = M. | last2 = Pages | first2 = M. | last3 = Tauziède-Espariat | first3 = A. | last4 = Saffroy | first4 = R. | last5 = Puget | first5 = S. | last6 = Lacroix | first6 = L. | last7 = Dezamis | first7 = E. | last8 = Devaux | first8 = B. | last9 = Chrétien | first9 = F. | title = Clinical, Imaging, Histopathological and Molecular Characterization of Anaplastic Ganglioglioma. | journal = J Neuropathol Exp Neurol | volume = 75 | issue = 10 | pages = 971-980 | month = Oct | year = 2016 | doi = 10.1093/jnen/nlw074 | PMID = 27539475 }}</ref> | ||
==Imaging== | ==Imaging== | ||
| Line 47: | Line 46: | ||
*Strong CM enhancement. | *Strong CM enhancement. | ||
*May contain cysts. | *May contain cysts. | ||
*Associated with | *Associated with temporal lobe. | ||
==Gross== | ==Gross== | ||
*Circumscribed lesion. | |||
* | *Usu. contrast enhancing. | ||
* | *Solid, but intracortical cysts may be present. | ||
* | *Little mass effect. | ||
* | |||
==Microscopic== | ==Microscopic== | ||
====Microscopic==== | |||
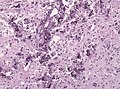
* | Features: | ||
* | *Dysplastic neurons. | ||
** | **Out of regular architecture / heterotopic location. | ||
* | **Cytomegaly | ||
**Abnormal clustering | |||
**Binucleated (very occassionally). | |||
**Perimembranous Nissl aggreation. | |||
*Atypical glia (ie neoplastic). | |||
*Eosinophilic granular bodies (more common than rosenthal fibers). | |||
*Dystrophic calcification. | |||
*Prominent capillary network. | |||
*Lymphocytic cuffing. | |||
*May contain some reticulin. | |||
*Glial component may resemble: | |||
**Fibrillary astrocytoma. | |||
**Oligodendroglioma. | |||
**Pilocytic astrocytoma. | |||
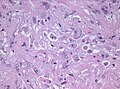
Anaplastic ganglioglioma: | |||
* | *Brisk mitotic activity | ||
* | *Necrosis | ||
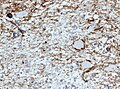
====IHC==== | |||
* | *Neurons: | ||
* | **[[MAP2]] +ve | ||
* | **Synaptophysin +ve | ||
* | ***Perikaryal surface immunoreactivity for synaptophysin.<ref name="pmid8246055">{{cite journal |authors=Lang FF, Epstein FJ, Ransohoff J, Allen JC, Wisoff J, Abbott IR, Miller DC |title=Central nervous system gangliogliomas. Part 2: Clinical outcome |journal=J. Neurosurg. |volume=79 |issue=6 |pages=867–73 |date=December 1993 |pmid=8246055 |doi=10.3171/jns.1993.79.6.0867 |url=}}</ref> | ||
*Pilocytic | ***This is however also seen in reactive changes.<ref name="pmid9591724">{{cite journal |authors=Quinn B |title=Synaptophysin staining in normal brain: importance for diagnosis of ganglioglioma |journal=Am. J. Surg. Pathol. |volume=22 |issue=5 |pages=550–6 |date=May 1998 |pmid=9591724 |doi=10.1097/00000478-199805000-00005 |url=}}</ref> | ||
** Neurofilament +ve | |||
** Chromogranin +ve | |||
*Glia: | |||
**CD34+/-ve | |||
*BRAF V600E +ve (approx. 25%, mainly ganglion cells). | |||
*MAP2: usu. absent. | |||
*MIB-1 (low, but resembles proliferative tumor component). | |||
====Molecular==== | |||
*BRAF V600E-mutated(approx. 25%).<ref>{{Cite journal | last1 = Schindler | first1 = G. | last2 = Capper | first2 = D. | last3 = Meyer | first3 = J. | last4 = Janzarik | first4 = W. | last5 = Omran | first5 = H. | last6 = Herold-Mende | first6 = C. | last7 = Schmieder | first7 = K. | last8 = Wesseling | first8 = P. | last9 = Mawrin | first9 = C. | title = Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. | journal = Acta Neuropathol | volume = 121 | issue = 3 | pages = 397-405 | month = Mar | year = 2011 | doi = 10.1007/s00401-011-0802-6 | PMID = 21274720 }}</ref> | |||
**BRAF V600E antibody stains especially neuronal cells.<ref>{{Cite journal | last1 = Koelsche | first1 = C. | last2 = Wöhrer | first2 = A. | last3 = Jeibmann | first3 = A. | last4 = Schittenhelm | first4 = J. | last5 = Schindler | first5 = G. | last6 = Preusser | first6 = M. | last7 = Lasitschka | first7 = F. | last8 = von Deimling | first8 = A. | last9 = Capper | first9 = D. | title = Mutant BRAF V600E protein in ganglioglioma is predominantly expressed by neuronal tumor cells. | journal = Acta Neuropathol | volume = 125 | issue = 6 | pages = 891-900 | month = Jun | year = 2013 | doi = 10.1007/s00401-013-1100-2 | PMID = 23435618 }}</ref> | |||
*IDH1/2 wt. | |||
*No 1p/19q codeletion. | |||
*Usu. Chr. 7 gain. | |||
*Rare cases with KIAA1459-BRAF fusion.<ref>{{Cite journal | last1 = Pekmezci | first1 = M. | last2 = Villanueva-Meyer | first2 = JE. | last3 = Goode | first3 = B. | last4 = Van Ziffle | first4 = J. | last5 = Onodera | first5 = C. | last6 = Grenert | first6 = JP. | last7 = Bastian | first7 = BC. | last8 = Chamyan | first8 = G. | last9 = Maher | first9 = OM. | title = The genetic landscape of ganglioglioma. | journal = Acta Neuropathol Commun | volume = 6 | issue = 1 | pages = 47 | month = 06 | year = 2018 | doi = 10.1186/s40478-018-0551-z | PMID = 29880043 }}</ref> | |||
** DDx: consider pilocytic astrocytoma with ganglioglioma component. <ref>{{Cite journal | last1 = Mesturoux | first1 = L. | last2 = Durand | first2 = K. | last3 = Pommepuy | first3 = I. | last4 = Robert | first4 = S. | last5 = Caire | first5 = F. | last6 = Labrousse | first6 = F. | title = Molecular Analysis of Tumor Cell Components in Pilocytic Astrocytomas, Gangliogliomas, and Oligodendrogliomas. | journal = Appl Immunohistochem Mol Morphol | volume = 24 | issue = 7 | pages = 496-500 | month = Aug | year = 2016 | doi = 10.1097/PAI.0000000000000288 | PMID = 27389560 }}</ref> | |||
*CDKN2A deletions, ATRX loss and TERT promotor mutations in anaplastic ganglioglioma.<ref>{{Cite journal | last1 = Zanello | first1 = M. | last2 = Pages | first2 = M. | last3 = Tauziède-Espariat | first3 = A. | last4 = Saffroy | first4 = R. | last5 = Puget | first5 = S. | last6 = Lacroix | first6 = L. | last7 = Dezamis | first7 = E. | last8 = Devaux | first8 = B. | last9 = Chrétien | first9 = F. | title = Clinical, Imaging, Histopathological and Molecular Characterization of Anaplastic Ganglioglioma. | journal = J Neuropathol Exp Neurol | volume = 75 | issue = 10 | pages = 971-980 | month = Oct | year = 2016 | doi = 10.1093/jnen/nlw074 | PMID = 27539475 }}</ref> | |||
**DD: consider anaplastic astrocytoma with piloid features (similiar molecular profile).<ref>{{Cite journal | last1 = Reinhardt | first1 = A. | last2 = Stichel | first2 = D. | last3 = Schrimpf | first3 = D. | last4 = Sahm | first4 = F. | last5 = Korshunov | first5 = A. | last6 = Reuss | first6 = DE. | last7 = Koelsche | first7 = C. | last8 = Huang | first8 = K. | last9 = Wefers | first9 = AK. | title = Anaplastic astrocytoma with piloid features, a novel molecular class of IDH wildtype glioma with recurrent MAPK pathway, CDKN2A/B and ATRX alterations. | journal = Acta Neuropathol | volume = 136 | issue = 2 | pages = 273-291 | month = Aug | year = 2018 | doi = 10.1007/s00401-018-1837-8 | PMID = 29564591 }} | |||
</ref> | |||
*H3F3A wildtype. | |||
**DDx: consider [[Diffuse hemispheric glioma, H3 G34-mutant]] (rare cases may contain dysplastic ganglion cells).<ref>{{Cite journal | last1 = Andreiuolo | first1 = F. | last2 = Lisner | first2 = T. | last3 = Zlocha | first3 = J. | last4 = Kramm | first4 = C. | last5 = Koch | first5 = A. | last6 = Bison | first6 = B. | last7 = Gareton | first7 = A. | last8 = Zanello | first8 = M. | last9 = Waha | first9 = A. | title = H3F3A-G34R mutant high grade neuroepithelial neoplasms with glial and dysplastic ganglion cell components. | journal = Acta Neuropathol Commun | volume = 7 | issue = 1 | pages = 78 | month = May | year = 2019 | doi = 10.1186/s40478-019-0731-5 | PMID = 31109382 }}</ref> | |||
*Rare cases with co-occurrence of K27M mutation.<ref>{{Cite journal | last1 = Pagès | first1 = M. | last2 = Beccaria | first2 = K. | last3 = Boddaert | first3 = N. | last4 = Saffroy | first4 = R. | last5 = Besnard | first5 = A. | last6 = Castel | first6 = D. | last7 = Fina | first7 = F. | last8 = Barets | first8 = D. | last9 = Barret | first9 = E. | title = Co-occurrence of histone H3 K27M and BRAF V600E mutations in paediatric midline grade I ganglioglioma. | journal = Brain Pathol | volume = | issue = | pages = | month = Dec | year = 2016 | doi = 10.1111/bpa.12473 | PMID = 27984673 }}</ref> | |||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
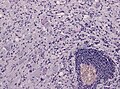
File:Ganglioglioma lymphocytic cuffing PAS.jpg | Lymphocytic cuffing in ganglioglioma (WC/jensflorian) | File:Ganglioglioma lymphocytic cuffing PAS.jpg | Lymphocytic cuffing in ganglioglioma (WC/jensflorian) | ||
| Line 95: | Line 116: | ||
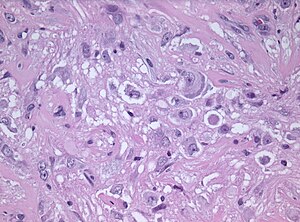
File:Anaplastic ganglioglioma HE.jpg | Pleomorphic ganglion cells in ganglioglioma (WC/jensflorian) | File:Anaplastic ganglioglioma HE.jpg | Pleomorphic ganglion cells in ganglioglioma (WC/jensflorian) | ||
</gallery> | </gallery> | ||
== | ==Prognosis== | ||
* | *Very good (10-year OS: 97%) | ||
*Primary treatment: surgery. | |||
**Seizure free outcome: 81%. | |||
**Incomplete resection as major factor for persisting epilepsia.<ref>{{Cite journal | last1 = Devaux | first1 = B. | last2 = Chassoux | first2 = F. | last3 = Landré | first3 = E. | last4 = Turak | first4 = B. | last5 = Laurent | first5 = A. | last6 = Zanello | first6 = M. | last7 = Mellerio | first7 = C. | last8 = Varlet | first8 = P. | title = Surgery for dysembryoplastic neuroepithelial tumors and gangliogliomas in eloquent areas. Functional results and seizure control. | journal = Neurochirurgie | volume = 63 | issue = 3 | pages = 227-234 | month = Jun | year = 2017 | doi = 10.1016/j.neuchi.2016.10.009 | PMID = 28506485 }}</ref> | |||
== | ====DDx:==== | ||
*[[DNT]]. | |||
*[[Oligodendroglioma]]. | |||
*[[PXA]]. | |||
*Desmoplastic infantile astrocytoma and ganglioglioma. | |||
*Cortical tuber. | |||
*[[ | *Trapped cortical neurons in diffuse astrocytoma. | ||
*[[ | *Papillary glioneuronal tumor. | ||
* | |||
* | |||
* | |||
* | |||
* | |||
==See also== | ==See also== | ||
Latest revision as of 09:01, 4 April 2022
| Ganglioglioma | |
|---|---|
| Diagnosis in short | |
 | |
| LM DDx | piloid gliosis, pilocytic astrocytoma, DNT |
| Stains | PAS-D +ve (eosinophilic granular bodies) |
| IHC | GFAP +ve, Synapto +ve |
| Gross | usually temporal +/-cystic |
| Site | brain - usu. supratentorial |
|
| |
| Syndromes | associated with epilepsy |
|
| |
| Prevalence | rare - esp. in children |
| Prognosis | good (WHO Grade I) |
Ganglioglioma is a epilepsy-associated glioneuronal tumour with benign course. Not to be confused with ganglioneuroma.
General
- Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1).
- Anaplastic ganglioglioma: Grade III (ICD-O: 9505/3)
- Rare (approx. 0.5% of all CNS tumors).
- Usu. temporal lobe.
- Predominantly children (mean age: 9 years).
- Recognized as a cause of epilepsy.[1]
- Favourable prognosis (survival rates up to 97%)
Imaging
- Well-defined, T2-hyperintense.
- Strong CM enhancement.
- May contain cysts.
- Associated with temporal lobe.
Gross
- Circumscribed lesion.
- Usu. contrast enhancing.
- Solid, but intracortical cysts may be present.
- Little mass effect.
Microscopic
Microscopic
Features:
- Dysplastic neurons.
- Out of regular architecture / heterotopic location.
- Cytomegaly
- Abnormal clustering
- Binucleated (very occassionally).
- Perimembranous Nissl aggreation.
- Atypical glia (ie neoplastic).
- Eosinophilic granular bodies (more common than rosenthal fibers).
- Dystrophic calcification.
- Prominent capillary network.
- Lymphocytic cuffing.
- May contain some reticulin.
- Glial component may resemble:
- Fibrillary astrocytoma.
- Oligodendroglioma.
- Pilocytic astrocytoma.
Anaplastic ganglioglioma:
- Brisk mitotic activity
- Necrosis
IHC
- Neurons:
- Glia:
- CD34+/-ve
- BRAF V600E +ve (approx. 25%, mainly ganglion cells).
- MAP2: usu. absent.
- MIB-1 (low, but resembles proliferative tumor component).
Molecular
- BRAF V600E-mutated(approx. 25%).[6]
- BRAF V600E antibody stains especially neuronal cells.[7]
- IDH1/2 wt.
- No 1p/19q codeletion.
- Usu. Chr. 7 gain.
- Rare cases with KIAA1459-BRAF fusion.[8]
- DDx: consider pilocytic astrocytoma with ganglioglioma component. [9]
- CDKN2A deletions, ATRX loss and TERT promotor mutations in anaplastic ganglioglioma.[10]
- DD: consider anaplastic astrocytoma with piloid features (similiar molecular profile).[11]
- H3F3A wildtype.
- DDx: consider Diffuse hemispheric glioma, H3 G34-mutant (rare cases may contain dysplastic ganglion cells).[12]
- Rare cases with co-occurrence of K27M mutation.[13]
Images
Prognosis
- Very good (10-year OS: 97%)
- Primary treatment: surgery.
- Seizure free outcome: 81%.
- Incomplete resection as major factor for persisting epilepsia.[14]
DDx:
- DNT.
- Oligodendroglioma.
- PXA.
- Desmoplastic infantile astrocytoma and ganglioglioma.
- Cortical tuber.
- Trapped cortical neurons in diffuse astrocytoma.
- Papillary glioneuronal tumor.
See also
References
- ↑ Im, SH.; Chung, CK.; Cho, BK.; Lee, SK. (Mar 2002). "Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome.". J Neurooncol 57 (1): 59-66. PMID 12125968.
- ↑ Terrier, LM.; Bauchet, L.; Rigau, V.; Amelot, A.; Zouaoui, S.; Filipiak, I.; Caille, A.; Almairac, F. et al. (05 2017). "Natural course and prognosis of anaplastic gangliogliomas: a multicenter retrospective study of 43 cases from the French Brain Tumor Database.". Neuro Oncol 19 (5): 678-688. doi:10.1093/neuonc/now186. PMID 28453747.
- ↑ Zanello, M.; Pages, M.; Tauziède-Espariat, A.; Saffroy, R.; Puget, S.; Lacroix, L.; Dezamis, E.; Devaux, B. et al. (Oct 2016). "Clinical, Imaging, Histopathological and Molecular Characterization of Anaplastic Ganglioglioma.". J Neuropathol Exp Neurol 75 (10): 971-980. doi:10.1093/jnen/nlw074. PMID 27539475.
- ↑ Lang FF, Epstein FJ, Ransohoff J, Allen JC, Wisoff J, Abbott IR, Miller DC (December 1993). "Central nervous system gangliogliomas. Part 2: Clinical outcome". J. Neurosurg. 79 (6): 867–73. doi:10.3171/jns.1993.79.6.0867. PMID 8246055.
- ↑ Quinn B (May 1998). "Synaptophysin staining in normal brain: importance for diagnosis of ganglioglioma". Am. J. Surg. Pathol. 22 (5): 550–6. doi:10.1097/00000478-199805000-00005. PMID 9591724.
- ↑ Schindler, G.; Capper, D.; Meyer, J.; Janzarik, W.; Omran, H.; Herold-Mende, C.; Schmieder, K.; Wesseling, P. et al. (Mar 2011). "Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma.". Acta Neuropathol 121 (3): 397-405. doi:10.1007/s00401-011-0802-6. PMID 21274720.
- ↑ Koelsche, C.; Wöhrer, A.; Jeibmann, A.; Schittenhelm, J.; Schindler, G.; Preusser, M.; Lasitschka, F.; von Deimling, A. et al. (Jun 2013). "Mutant BRAF V600E protein in ganglioglioma is predominantly expressed by neuronal tumor cells.". Acta Neuropathol 125 (6): 891-900. doi:10.1007/s00401-013-1100-2. PMID 23435618.
- ↑ Pekmezci, M.; Villanueva-Meyer, JE.; Goode, B.; Van Ziffle, J.; Onodera, C.; Grenert, JP.; Bastian, BC.; Chamyan, G. et al. (06 2018). "The genetic landscape of ganglioglioma.". Acta Neuropathol Commun 6 (1): 47. doi:10.1186/s40478-018-0551-z. PMID 29880043.
- ↑ Mesturoux, L.; Durand, K.; Pommepuy, I.; Robert, S.; Caire, F.; Labrousse, F. (Aug 2016). "Molecular Analysis of Tumor Cell Components in Pilocytic Astrocytomas, Gangliogliomas, and Oligodendrogliomas.". Appl Immunohistochem Mol Morphol 24 (7): 496-500. doi:10.1097/PAI.0000000000000288. PMID 27389560.
- ↑ Zanello, M.; Pages, M.; Tauziède-Espariat, A.; Saffroy, R.; Puget, S.; Lacroix, L.; Dezamis, E.; Devaux, B. et al. (Oct 2016). "Clinical, Imaging, Histopathological and Molecular Characterization of Anaplastic Ganglioglioma.". J Neuropathol Exp Neurol 75 (10): 971-980. doi:10.1093/jnen/nlw074. PMID 27539475.
- ↑ Reinhardt, A.; Stichel, D.; Schrimpf, D.; Sahm, F.; Korshunov, A.; Reuss, DE.; Koelsche, C.; Huang, K. et al. (Aug 2018). "Anaplastic astrocytoma with piloid features, a novel molecular class of IDH wildtype glioma with recurrent MAPK pathway, CDKN2A/B and ATRX alterations.". Acta Neuropathol 136 (2): 273-291. doi:10.1007/s00401-018-1837-8. PMID 29564591.
- ↑ Andreiuolo, F.; Lisner, T.; Zlocha, J.; Kramm, C.; Koch, A.; Bison, B.; Gareton, A.; Zanello, M. et al. (May 2019). "H3F3A-G34R mutant high grade neuroepithelial neoplasms with glial and dysplastic ganglion cell components.". Acta Neuropathol Commun 7 (1): 78. doi:10.1186/s40478-019-0731-5. PMID 31109382.
- ↑ Pagès, M.; Beccaria, K.; Boddaert, N.; Saffroy, R.; Besnard, A.; Castel, D.; Fina, F.; Barets, D. et al. (Dec 2016). "Co-occurrence of histone H3 K27M and BRAF V600E mutations in paediatric midline grade I ganglioglioma.". Brain Pathol. doi:10.1111/bpa.12473. PMID 27984673.
- ↑ Devaux, B.; Chassoux, F.; Landré, E.; Turak, B.; Laurent, A.; Zanello, M.; Mellerio, C.; Varlet, P. (Jun 2017). "Surgery for dysembryoplastic neuroepithelial tumors and gangliogliomas in eloquent areas. Functional results and seizure control.". Neurochirurgie 63 (3): 227-234. doi:10.1016/j.neuchi.2016.10.009. PMID 28506485.