Difference between revisions of "Ganglioglioma"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (infobox) |
Jensflorian (talk | contribs) (update) |
||
| Line 30: | Line 30: | ||
| Tx = | | Tx = | ||
}} | }} | ||
Ganglioglioma is a epilepsy-associated glioneuronal tumour with benign course. '''Not''' to be confused with ''[[ganglioneuroma]]''. | |||
====General==== | ====General==== | ||
*Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1). | *Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1). | ||
| Line 40: | Line 41: | ||
*Favourable prognosis (survival rates up to 97%) | *Favourable prognosis (survival rates up to 97%) | ||
**Insufficient data für anaplastic ganglioglioma. | **Insufficient data für anaplastic ganglioglioma. | ||
==Imaging== | ==Imaging== | ||
| Line 47: | Line 46: | ||
*Strong CM enhancement. | *Strong CM enhancement. | ||
*May contain cysts. | *May contain cysts. | ||
*Associated with | *Associated with temporal lobe. | ||
==Gross== | ==Gross== | ||
| Line 56: | Line 55: | ||
==Microscopic== | ==Microscopic== | ||
====Microscopic==== | |||
* | Features: | ||
* | *Dysplastic neurons. | ||
* | **Out of regular architecture / abnormal location. | ||
** | **Cytomegaly | ||
* | **Clustering | ||
** | **Binucleated (very occassionally). | ||
*Atypical glia. | |||
*Eosinophilic granular bodies. | *Eosinophilic granular bodies. | ||
* | *Calcification. | ||
*Prominent capillary network. | |||
*Lymphocytic cuffing. | |||
*May contain some reticulin. | |||
*Glial component may resemble: | |||
**Fibrillary astrocytoma. | |||
**Oligodendroglioma. | |||
**Pilocytic astrocytoma. | |||
Anaplastic ganglioglioma: | |||
* | *Brisk mitotic activity | ||
*Necrosis | |||
====IHC==== | |||
* | *Neurons: | ||
* | **[[MAP2]] +ve | ||
* | **Synaptophysin +ve | ||
* | ** Neurofilament +ve | ||
*Glia: | |||
**CD34+/-ve | |||
*BRAF V600E +ve (approx. 25%, mainly ganglion cells). | |||
====Molecular==== | |||
* | *BRAF V600E-mutated(approx. 25%). | ||
* | *IDH1/2 wt. | ||
* | *No 1p/19q codeletion. | ||
* | *Usu. Chr. 7 gain. | ||
* | *CDKN2A deletions in anaplastic ganglioglioma. | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
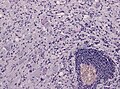
File:Ganglioglioma lymphocytic cuffing PAS.jpg | Lymphocytic cuffing in ganglioglioma (WC/jensflorian) | File:Ganglioglioma lymphocytic cuffing PAS.jpg | Lymphocytic cuffing in ganglioglioma (WC/jensflorian) | ||
| Line 94: | Line 102: | ||
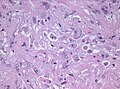
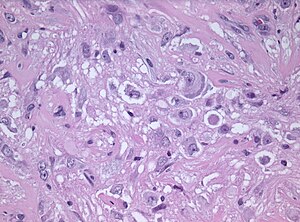
File:Anaplastic ganglioglioma HE.jpg | Pleomorphic ganglion cells in ganglioglioma (WC/jensflorian) | File:Anaplastic ganglioglioma HE.jpg | Pleomorphic ganglion cells in ganglioglioma (WC/jensflorian) | ||
</gallery> | </gallery> | ||
== | ==Prognosis== | ||
* | *Good (10-year OS: 90%), but epilepsy may continue. | ||
*Primary treatment: surgery. | |||
== | ====DDx:==== | ||
*[[DNT]]. | |||
*[[Oligodendroglioma]]. | |||
*Trapped cortical neurons in diffuse astrocytoma. | |||
*Papillary glioneuronal tumor. | |||
*Dysembryoplastic neuroepithelial tumor. | |||
*[[ | |||
*[[ | |||
* | |||
* | |||
* | |||
==See also== | ==See also== | ||
Revision as of 10:10, 14 September 2017
| Ganglioglioma | |
|---|---|
| Diagnosis in short | |
 | |
| LM DDx | piloid gliosis, pilocytic astrocytoma, DNT |
| Stains | PAS-D +ve (eosinophilic granular bodies) |
| IHC | GFAP +ve, Synapto +ve |
| Gross | usually temporal +/-cystic |
| Site | brain - usu. supratentorial |
|
| |
| Syndromes | associated with epilepsy |
|
| |
| Prevalence | rare - esp. in children |
| Prognosis | good (WHO Grade I) |
Ganglioglioma is a epilepsy-associated glioneuronal tumour with benign course. Not to be confused with ganglioneuroma.
General
- Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1).
- Anaplastic ganglioglioma: Grade III (ICD-O: 9505/3)
- Rare (approx. 0.5% of all CNS tumors).
- Usu. temporal lobe.
- Predominantly children (mean age: 9 years).
- Recognized as a cause of epilepsy.[1]
- Favourable prognosis (survival rates up to 97%)
- Insufficient data für anaplastic ganglioglioma.
Imaging
- Well-defined, T2-hyperintense.
- Strong CM enhancement.
- May contain cysts.
- Associated with temporal lobe.
Gross
- Circumscribed lesion.
- Usu. contrast enhancing.
- Solid, but intracortical cysts may be present.
- Little mass effect.
Microscopic
Microscopic
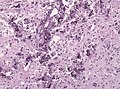
Features:
- Dysplastic neurons.
- Out of regular architecture / abnormal location.
- Cytomegaly
- Clustering
- Binucleated (very occassionally).
- Atypical glia.
- Eosinophilic granular bodies.
- Calcification.
- Prominent capillary network.
- Lymphocytic cuffing.
- May contain some reticulin.
- Glial component may resemble:
- Fibrillary astrocytoma.
- Oligodendroglioma.
- Pilocytic astrocytoma.
Anaplastic ganglioglioma:
- Brisk mitotic activity
- Necrosis
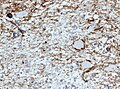
IHC
- Neurons:
- MAP2 +ve
- Synaptophysin +ve
- Neurofilament +ve
- Glia:
- CD34+/-ve
- BRAF V600E +ve (approx. 25%, mainly ganglion cells).
Molecular
- BRAF V600E-mutated(approx. 25%).
- IDH1/2 wt.
- No 1p/19q codeletion.
- Usu. Chr. 7 gain.
- CDKN2A deletions in anaplastic ganglioglioma.
Images
Prognosis
- Good (10-year OS: 90%), but epilepsy may continue.
- Primary treatment: surgery.
DDx:
- DNT.
- Oligodendroglioma.
- Trapped cortical neurons in diffuse astrocytoma.
- Papillary glioneuronal tumor.
- Dysembryoplastic neuroepithelial tumor.