Difference between revisions of "Ganglioglioma"
Jump to navigation
Jump to search
(redirect) |
Jensflorian (talk | contribs) (created, not finished!) |
||
| Line 1: | Line 1: | ||
# | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = | |||
| Width = | |||
| Caption = | |||
| Synonyms = | |||
| Micro = | |||
| Subtypes = | |||
| LMDDx = piloid gliosis, [[pilocytic astrocytoma]], [[DNT]] | |||
| Stains = PAS-D +ve (eosinophilic granular bodies) | |||
| IHC = GFAP +ve, Synapto +ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = usually temporal +/-cystic | |||
| Grossing = | |||
| Site = brain - usu. supratentorial | |||
| Assdx = | |||
| Syndromes = associated with epilepsy | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = rare - esp. in children | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = good (WHO Grade I) | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
:'''Not''' to be confused with ''[[ganglioneuroma]]''. | |||
====General==== | |||
*Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1). | |||
*Anaplastic ganglioglioma: Grade III (ICD-O: 9505/3) | |||
*Rare (approx. 0.5% of all CNS tumors). | |||
*Usu. temporal lobe. | |||
*Predominantly children (mean age: 9 years). | |||
*Recognized as a cause of [[epilepsy]].<ref name=pmid12125968>{{Cite journal | last1 = Im | first1 = SH. | last2 = Chung | first2 = CK. | last3 = Cho | first3 = BK. | last4 = Lee | first4 = SK. | title = Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome. | journal = J Neurooncol | volume = 57 | issue = 1 | pages = 59-66 | month = Mar | year = 2002 | doi = | PMID = 12125968 }}</ref> | |||
*Favourable prognosis (survival rates up to 97%) | |||
**Insufficient data für anaplastic ganglioglioma. | |||
==Imaging== | |||
*Well-defined, T2-hyperintense. | |||
*Strong CM enhancement. | |||
*May contain cysts. | |||
*Associated with midline structures. | |||
==Gross== | |||
Features:<ref name=Ref_PSNP82>{{Ref PSNP|82}}</ref> | |||
*Usually well-circumscribed, soft. | |||
*Can be cystic with mural nodule. | |||
*Optic gliomas may present as fusiform mass. | |||
*Occ. calcium deposits and hemosiderin. | |||
==Microscopic== | |||
Features:<ref name=Ref_PSNP82-4>{{Ref PSNP|82-4}}</ref> | |||
*Classically biphasic (though either may be absent): | |||
*#Fibrillar. | |||
*#Microcystic/loose. | |||
*Hair-like fibres ~ 1 micrometer; ''pilo-'' = hair.<ref>URL: [http://dictionary.reference.com/browse/pilo- http://dictionary.reference.com/browse/pilo-]. Accessed on: 24 November 2010.</ref> | |||
**Best seen on smear or with GFAP [[IHC]]. | |||
*Rosenthal fibres - '''key feature'''. | |||
**May be rare. Not pathognomonic (see below). | |||
*Eosinophilic granular bodies. | |||
*Low cellularity - when compared to medulloblastoma and ependymoma. | |||
Notes: | |||
*+/-Microvascular proliferation. | |||
*+/-Focal necrosis. | |||
**Necrosis with pseudopalisading more likely glioblastoma. | |||
*+/-Mitoses - not significant in the context of the Dx. | |||
DDx (of Rosenthal fibers):<ref>Munoz D. 9 Mar 2009.</ref> | |||
*Chronic reactive gliosis. | |||
*Subependymoma. | |||
*Pilocytic astrocytoma. | |||
*Ganglioglioma. | |||
DDx of pilocystic astrocytoma (brief): | |||
*Piloid gliosis (esp. in sellar lesions). | |||
*[[Oligodendroglioma]]. | |||
*[[Glioblastoma]] (uncommon - but important). | |||
*Tanycytic [[Ependymoma]] | |||
*Pilocytic tumor components may be found in [[Ganglioglioma]], [[DNET]], [[RGNT]] | |||
===Images=== | |||
====Smears==== | |||
<gallery> | |||
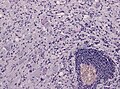
File:Ganglioglioma lymphocytic cuffing PAS.jpg | Lymphocytic cuffing in ganglioglioma (WC/jensflorian) | |||
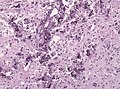
File:Ganglioglioma calcification.jpg | Calcification in ganglioglioma (WC/jensflorian) | |||
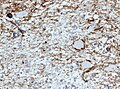
File:Ganglioglioma Cd34 x200.jpg | CD34 immunostain in ganglioglioma (WC/jensflorian) | |||
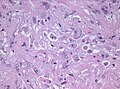
File:Anaplastic ganglioglioma HE.jpg | Pleomorphic ganglion cells in ganglioglioma (WC/jensflorian) | |||
</gallery> | |||
====Sections==== | |||
<gallery> | |||
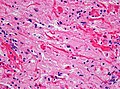
Image:Rosenthal_HE_40x.jpg | Rosenthal fibres. (WC) | |||
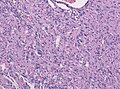
Image:Pilocytic astrocytoma cell pleomorphism.jpg | Occasional pleomorphism. (WC) | |||
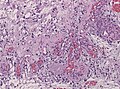
Image:Pilocytic astrocytoma endothelial proliferations.jpg | Microvascular proliferation. (WC) | |||
</gallery> | |||
www: | |||
*[http://moon.ouhsc.edu/kfung/jty1/neurotest/Q19-Ans.htm Rosenthal fibre (ouhsc.edu)]. | |||
*[http://path.upmc.edu/cases/case162.html Pilocytic astrocytoma (upmc.edu)]. | |||
*[http://path.upmc.edu/cases/case90.html Pilocytic astrocytoma - another case (upmc.edu)]. | |||
*[http://path.upmc.edu/cases/case195/images/figure3b.jpg Pilocytic astrocytoma - pennies on a plate (upmc.edu)].<ref>URL: [http://path.upmc.edu/cases/case195.html http://path.upmc.edu/cases/case195.html]. Accessed on: 8 January 2012.</ref> | |||
*[http://path.upmc.edu/cases/case397.html Pilocytic astrocytoma (upmc.edu)]. | |||
==Stains== | |||
*PAS-D: eosinophilic granular bodies +ve. | |||
==IHC== | |||
Features:<ref name=Ref_PSNP84>{{Ref PSNP|84}}</ref> | |||
*GFAP +ve (fibres). | |||
*CD68: may have a significant macrophage component. | |||
*KI-67: may be "high" (~20% ???). | |||
*Olig 2: Usually strongly present.<ref name=pmid21193945>{{Cite journal | last1 = Otero | first1 = JJ. | last2 = Rowitch | first2 = D. | last3 = Vandenberg | first3 = S. | title = OLIG2 is differentially expressed in pediatric astrocytic and in ependymal neoplasms. | journal = J Neurooncol | volume = 104 | issue = 2 | pages = 423-38 | month = Sep | year = 2011 | doi = 10.1007/s11060-010-0509-x | PMID = 21193945 }}</ref> | |||
*[[IDH1]] (R132H) -ve. | |||
*[[H3F3A]] (K27M) -ve. | |||
==Molecular== | |||
* Almost all alteration associated with the MAPK pathway.<ref>{{Cite journal | last1 = Collins | first1 = VP. | last2 = Jones | first2 = DT. | last3 = Giannini | first3 = C. | title = Pilocytic astrocytoma: pathology, molecular mechanisms and markers. | journal = Acta Neuropathol | volume = 129 | issue = 6 | pages = 775-88 | month = Jun | year = 2015 | doi = 10.1007/s00401-015-1410-7 | PMID = 25792358 }}</ref> | |||
* KIAA1549-BRAF fusion transcripts most common in sporadic PA (up to 2/3 of all cases). | |||
**DDx: Fusion reported in rare Diffuse Leptomeingeal Glioneuronal Tumors and Oligodendroglioma. | |||
* Rarely BRAF, KRAS or FGFR1 mutations, NTRK2, SRGAP3-RAF1 or FAM131B-BRAF fusions.<ref>{{Cite journal | last1 = Jones | first1 = DT. | last2 = Hutter | first2 = B. | last3 = Jäger | first3 = N. | last4 = Korshunov | first4 = A. | last5 = Kool | first5 = M. | last6 = Warnatz | first6 = HJ. | last7 = Zichner | first7 = T. | last8 = Lambert | first8 = SR. | last9 = Ryzhova | first9 = M. | title = Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. | journal = Nat Genet | volume = 45 | issue = 8 | pages = 927-32 | month = Aug | year = 2013 | doi = 10.1038/ng.2682 | PMID = 23817572 }}</ref><ref>{{Cite journal | last1 = Cin | first1 = H. | last2 = Meyer | first2 = C. | last3 = Herr | first3 = R. | last4 = Janzarik | first4 = WG. | last5 = Lambert | first5 = S. | last6 = Jones | first6 = DT. | last7 = Jacob | first7 = K. | last8 = Benner | first8 = A. | last9 = Witt | first9 = H. | title = Oncogenic FAM131B-BRAF fusion resulting from 7q34 deletion comprises an alternative mechanism of MAPK pathway activation in pilocytic astrocytoma. | journal = Acta Neuropathol | volume = 121 | issue = 6 | pages = 763-74 | month = Jun | year = 2011 | doi = 10.1007/s00401-011-0817-z | PMID = 21424530 }}</ref> | |||
*Up to 15% of all [[NF1]] patients develop a PA ("optic glioma" as predilection).<ref>{{Cite journal | last1 = Friedrich | first1 = RE. | last2 = Nuding | first2 = MA. | title = Optic Pathway Glioma and Cerebral Focal Abnormal Signal Intensity in Patients with Neurofibromatosis Type 1: Characteristics, Treatment Choices and Follow-up in 134 Affected Individuals and a Brief Review of the Literature. | journal = Anticancer Res | volume = 36 | issue = 8 | pages = 4095-121 | month = Aug | year = 2016 | doi = | PMID = 27466519 }}</ref> | |||
*Rare reports of PA in Noonan-Syndrome (PTPN11 mutation).<ref>{{Cite journal | last1 = Jones | first1 = DT. | last2 = Hutter | first2 = B. | last3 = Jäger | first3 = N. | last4 = Korshunov | first4 = A. | last5 = Kool | first5 = M. | last6 = Warnatz | first6 = HJ. | last7 = Zichner | first7 = T. | last8 = Lambert | first8 = SR. | last9 = Ryzhova | first9 = M. | title = Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. | journal = Nat Genet | volume = 45 | issue = 8 | pages = 927-32 | month = Aug | year = 2013 | doi = 10.1038/ng.2682 | PMID = 23817572 }}</ref> | |||
==Prognosis== | |||
*Excellent (10-year OS: 90%) | |||
*In thalamic/chiasmatic region not so good (incomplete resection, often [[Pilomyxoid astrocytoma]]). | |||
*Primary treatment: surgery. Incomplete resection: RT has to be considered. | |||
**Chx is given in rare cases that are still progredient<ref>{{Cite journal | last1 = Metts | first1 = RD. | last2 = Bartynski | first2 = W. | last3 = Welsh | first3 = CT. | last4 = Kinsman | first4 = S. | last5 = Bredlau | first5 = AL. | title = Bevacizumab Therapy for Pilomyxoid Astrocytoma. | journal = J Pediatr Hematol Oncol | volume = | issue = | pages = | month = Mar | year = 2017 | doi = 10.1097/MPH.0000000000000824 | PMID = 28338567 }}</ref> | |||
==See also== | |||
*[[Neuropathology tumours]]. | |||
*[[Pilocytic Astrocytoma]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Neuropathology tumours]] | |||
Revision as of 08:12, 14 September 2017
| Ganglioglioma | |
|---|---|
| Diagnosis in short | |
| LM DDx | piloid gliosis, pilocytic astrocytoma, DNT |
| Stains | PAS-D +ve (eosinophilic granular bodies) |
| IHC | GFAP +ve, Synapto +ve |
| Gross | usually temporal +/-cystic |
| Site | brain - usu. supratentorial |
|
| |
| Syndromes | associated with epilepsy |
|
| |
| Prevalence | rare - esp. in children |
| Prognosis | good (WHO Grade I) |
- Not to be confused with ganglioneuroma.
General
- Gangliolioma: Grade I WHO mixed neuronal-glial tumour (ICD-O code: 9505/1).
- Anaplastic ganglioglioma: Grade III (ICD-O: 9505/3)
- Rare (approx. 0.5% of all CNS tumors).
- Usu. temporal lobe.
- Predominantly children (mean age: 9 years).
- Recognized as a cause of epilepsy.[1]
- Favourable prognosis (survival rates up to 97%)
- Insufficient data für anaplastic ganglioglioma.
Imaging
- Well-defined, T2-hyperintense.
- Strong CM enhancement.
- May contain cysts.
- Associated with midline structures.
Gross
Features:[2]
- Usually well-circumscribed, soft.
- Can be cystic with mural nodule.
- Optic gliomas may present as fusiform mass.
- Occ. calcium deposits and hemosiderin.
Microscopic
Features:[3]
- Classically biphasic (though either may be absent):
- Fibrillar.
- Microcystic/loose.
- Hair-like fibres ~ 1 micrometer; pilo- = hair.[4]
- Best seen on smear or with GFAP IHC.
- Rosenthal fibres - key feature.
- May be rare. Not pathognomonic (see below).
- Eosinophilic granular bodies.
- Low cellularity - when compared to medulloblastoma and ependymoma.
Notes:
- +/-Microvascular proliferation.
- +/-Focal necrosis.
- Necrosis with pseudopalisading more likely glioblastoma.
- +/-Mitoses - not significant in the context of the Dx.
DDx (of Rosenthal fibers):[5]
- Chronic reactive gliosis.
- Subependymoma.
- Pilocytic astrocytoma.
- Ganglioglioma.
DDx of pilocystic astrocytoma (brief):
- Piloid gliosis (esp. in sellar lesions).
- Oligodendroglioma.
- Glioblastoma (uncommon - but important).
- Tanycytic Ependymoma
- Pilocytic tumor components may be found in Ganglioglioma, DNET, RGNT
Images
Smears
Sections
www:
- Rosenthal fibre (ouhsc.edu).
- Pilocytic astrocytoma (upmc.edu).
- Pilocytic astrocytoma - another case (upmc.edu).
- Pilocytic astrocytoma - pennies on a plate (upmc.edu).[6]
- Pilocytic astrocytoma (upmc.edu).
Stains
- PAS-D: eosinophilic granular bodies +ve.
IHC
Features:[7]
- GFAP +ve (fibres).
- CD68: may have a significant macrophage component.
- KI-67: may be "high" (~20% ???).
- Olig 2: Usually strongly present.[8]
- IDH1 (R132H) -ve.
- H3F3A (K27M) -ve.
Molecular
- Almost all alteration associated with the MAPK pathway.[9]
- KIAA1549-BRAF fusion transcripts most common in sporadic PA (up to 2/3 of all cases).
- DDx: Fusion reported in rare Diffuse Leptomeingeal Glioneuronal Tumors and Oligodendroglioma.
- Rarely BRAF, KRAS or FGFR1 mutations, NTRK2, SRGAP3-RAF1 or FAM131B-BRAF fusions.[10][11]
- Up to 15% of all NF1 patients develop a PA ("optic glioma" as predilection).[12]
- Rare reports of PA in Noonan-Syndrome (PTPN11 mutation).[13]
Prognosis
- Excellent (10-year OS: 90%)
- In thalamic/chiasmatic region not so good (incomplete resection, often Pilomyxoid astrocytoma).
- Primary treatment: surgery. Incomplete resection: RT has to be considered.
- Chx is given in rare cases that are still progredient[14]
See also
References
- ↑ Im, SH.; Chung, CK.; Cho, BK.; Lee, SK. (Mar 2002). "Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome.". J Neurooncol 57 (1): 59-66. PMID 12125968.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 82. ISBN 978-0443069826.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 82-4. ISBN 978-0443069826.
- ↑ URL: http://dictionary.reference.com/browse/pilo-. Accessed on: 24 November 2010.
- ↑ Munoz D. 9 Mar 2009.
- ↑ URL: http://path.upmc.edu/cases/case195.html. Accessed on: 8 January 2012.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 84. ISBN 978-0443069826.
- ↑ Otero, JJ.; Rowitch, D.; Vandenberg, S. (Sep 2011). "OLIG2 is differentially expressed in pediatric astrocytic and in ependymal neoplasms.". J Neurooncol 104 (2): 423-38. doi:10.1007/s11060-010-0509-x. PMID 21193945.
- ↑ Collins, VP.; Jones, DT.; Giannini, C. (Jun 2015). "Pilocytic astrocytoma: pathology, molecular mechanisms and markers.". Acta Neuropathol 129 (6): 775-88. doi:10.1007/s00401-015-1410-7. PMID 25792358.
- ↑ Jones, DT.; Hutter, B.; Jäger, N.; Korshunov, A.; Kool, M.; Warnatz, HJ.; Zichner, T.; Lambert, SR. et al. (Aug 2013). "Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma.". Nat Genet 45 (8): 927-32. doi:10.1038/ng.2682. PMID 23817572.
- ↑ Cin, H.; Meyer, C.; Herr, R.; Janzarik, WG.; Lambert, S.; Jones, DT.; Jacob, K.; Benner, A. et al. (Jun 2011). "Oncogenic FAM131B-BRAF fusion resulting from 7q34 deletion comprises an alternative mechanism of MAPK pathway activation in pilocytic astrocytoma.". Acta Neuropathol 121 (6): 763-74. doi:10.1007/s00401-011-0817-z. PMID 21424530.
- ↑ Friedrich, RE.; Nuding, MA. (Aug 2016). "Optic Pathway Glioma and Cerebral Focal Abnormal Signal Intensity in Patients with Neurofibromatosis Type 1: Characteristics, Treatment Choices and Follow-up in 134 Affected Individuals and a Brief Review of the Literature.". Anticancer Res 36 (8): 4095-121. PMID 27466519.
- ↑ Jones, DT.; Hutter, B.; Jäger, N.; Korshunov, A.; Kool, M.; Warnatz, HJ.; Zichner, T.; Lambert, SR. et al. (Aug 2013). "Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma.". Nat Genet 45 (8): 927-32. doi:10.1038/ng.2682. PMID 23817572.
- ↑ Metts, RD.; Bartynski, W.; Welsh, CT.; Kinsman, S.; Bredlau, AL. (Mar 2017). "Bevacizumab Therapy for Pilomyxoid Astrocytoma.". J Pediatr Hematol Oncol. doi:10.1097/MPH.0000000000000824. PMID 28338567.