Difference between revisions of "Ewing sarcoma"
Jump to navigation
Jump to search
m (+DDx, Ewing-like link) |
|||
| Line 8: | Line 8: | ||
| LMDDx = [[Ewing-like tumours]] (e.g. [[CIC-DUX sarcoma]]), [[small round cell tumours]] ([[lymphoma]], [[small cell osteosarcoma]], others) | | LMDDx = [[Ewing-like tumours]] (e.g. [[CIC-DUX sarcoma]]), [[small round cell tumours]] ([[lymphoma]], [[small cell osteosarcoma]], others) | ||
| Stains = [[PAS stain]] +ve, [[PASD stain]] -ve | | Stains = [[PAS stain]] +ve, [[PASD stain]] -ve | ||
| IHC = CD99 +ve, FLI-1 +ve, CD45 -ve | | IHC = [[CD99]] +ve, FLI-1 +ve, CD45 -ve | ||
| EM = | | EM = | ||
| Molecular = EWS [[Chromosomal translocations|translocation]], EWS/FLI-1 fusion gene in 90% of cases | | Molecular = EWS [[Chromosomal translocations|translocation]], EWS/FLI-1 fusion gene in 90% of cases | ||
| Line 102: | Line 102: | ||
Notes:<ref>PST. 22 February 2010.</ref> | Notes:<ref>PST. 22 February 2010.</ref> | ||
*CD99 +ve | *[[CD99]] +ve | ||
**Plasma membrane staining tumours: | **Plasma membrane staining tumours: | ||
***[[Lymphoblastic lymphoma]]/leukemia. | ***[[Lymphoblastic lymphoma]]/leukemia. | ||
Latest revision as of 12:37, 15 October 2015
| Ewing sarcoma | |
|---|---|
| Diagnosis in short | |
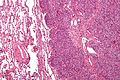
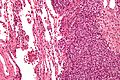
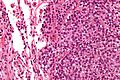
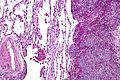
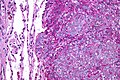
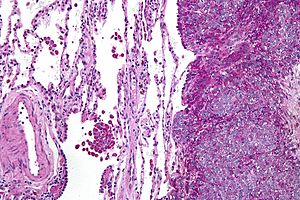 Ewing sarcoma. PAS stain. | |
|
| |
| LM | small round cell tumour, clear cytoplasm |
| LM DDx | Ewing-like tumours (e.g. CIC-DUX sarcoma), small round cell tumours (lymphoma, small cell osteosarcoma, others) |
| Stains | PAS stain +ve, PASD stain -ve |
| IHC | CD99 +ve, FLI-1 +ve, CD45 -ve |
| Molecular | EWS translocation, EWS/FLI-1 fusion gene in 90% of cases |
| Site | bone, rarely other sites |
|
| |
| Clinical history | usually <20 years old |
| Prevalence | uncommon |
Ewing sarcoma, also known as EWS/pPNET, is an uncommon bone tumour.
Confusingly, it is known as EWS/PNET. EWS is Ewing sarcoma. pPNET is peripheral primitive neuroectodermal tumour. EWS and pPNET were once thought to be different tumours.
Peripheral primitive neuroectodermal tumour should not be confused with primitive neuroectodermal tumour, commonly abbreviated PNET, a (supertentorial) brain tumour with similarities to medulloblastoma.
General
Clinical:
- Painful.
- Usually younger than 20 years.
- Second most common malignant bone tumour in children.
- Most common malignant bone tumour = osteosarcoma (AKA osteogenic sarcoma).
Poor prognostic factors:[1]
- Age (18 years-old+).
- Pelvis (extremity = good).
- >8 cm.
- Metastases.
- EWS-FL1 fusion type 2.
- >90% necrosis.
Etiology:
- Unknown origin; hypothesis: Ewing sarcoma arises from mesenchymal stem cell.[2]
Radiology
Features:[3]
- Long bones, diaphyses.
- Destructive.
- "Onion-skin" periosteal reaction.
Microscopic
Features:[4]
- Scant clear cytoplasm (contain glycogen -- PAS +ve, PAS-D -ve) - key feature.
- Round small nucleus.
- Usu. lack nucleoli.
- Usu. minimal-moderate size variation.
- Mitoses (common).
Notes:
- It is a small round cell tumour.
- Rhabdomyosarcoma occasionally has cytoplasmic clearing (due to glycogen).[5]
DDx:
- Ewing-like tumours (e.g. CIC-DUX sarcoma).
- Large cell lymphoma.
- Other small round cell tumours (e.g. small cell osteosarcoma).
Images
www:
- Ewing sarcoma - case 1 - several images (upmc.edu).
- Ewing sarcoma - case 2 - several images (upmc.edu).
IHC
Features:[6]
- CD99 +ve -- 1. diffuse, 2. plasma membrane staining; both required -- most specific.
- FLI-1 +ve.[7]
- CD45 -ve.
- Done to r/o lymphoma.
- +/-Neural markers (NSE, synaptophysin, CD57 (??? CD56 ???), S-100).
- +/-Cytokeratins.
- Caveolin-1 +ve in ~ 85% of EWS.[8]
- WT-1 -ve.[9]
Notes:[10]
Molecular diagnostics
Common features:
- EWS/FLI-1 fusion gene formation due to translocation: t(11;22)(q24;q12).[11][12]
- Often detected by RT-PCR (with EWS 5' and FLI-1 3' primers).
- Type 1 = EWS exon 7 + FLI-1 exon 6; good prognosis.
- Type 2 = others; poor prognosis.
Notes:
- The t(11;22)(q24;q12) is seen in ~90% of EWS/PNET... but also in:
- Olfactory neuroblastoma.
- Small cell osteogenic sarcoma (small cell variant of osteosarcoma).
- Polyphenotypic tumours.
- Rhabdomyosarcoma.
- Neuroblastoma (possibly).
- Several other EWS translocations exist.[13]
- ERG,[14] ETV1, E1AF and FEV.
- Lack of molecular findings does not exclude Ewing sarcoma.
- Testing:
- A break apart probe for EWS is a common way to look for pathologic change, as it covers almost all variants.
Electron microscopy
- Primitive cell junctions.
- Clear zone (glycogen lakes).
See also
References
- ↑ PST. 14 February 2011.
- ↑ Lin PP, Wang Y, Lozano G (2011). "Mesenchymal Stem Cells and the Origin of Ewing's Sarcoma". Sarcoma 2011. doi:10.1155/2011/276463. PMC 2952797. PMID 20953407. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952797/.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 650. ISBN 978-0781765275.
- ↑ PST. 22 February 2010.
- ↑ PST. 14 February 2011.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 651. ISBN 978-0781765275.
- ↑ 7.0 7.1 Rossi S, Orvieto E, Furlanetto A, Laurino L, Ninfo V, Dei Tos AP (May 2004). "Utility of the immunohistochemical detection of FLI-1 expression in round cell and vascular neoplasm using a monoclonal antibody". Mod. Pathol. 17 (5): 547–52. doi:10.1038/modpathol.3800065. PMID 15001993. http://www.nature.com/modpathol/journal/v17/n5/full/3800065a.html.
- ↑ PST. 14 February 2011.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 286. ISBN 978-0781765275.
- ↑ PST. 22 February 2010.
- ↑ URL: http://atlasgeneticsoncology.org/Tumors/Ewing5010.html. Accessed on: 23 February 2010.
- ↑ Turc-Carel C, Aurias A, Mugneret F, et al. (June 1988). "Chromosomes in Ewing's sarcoma. I. An evaluation of 85 cases of remarkable consistency of t(11;22)(q24;q12)". Cancer Genet. Cytogenet. 32 (2): 229–38. PMID 3163261.
- ↑ URL: http://www.cancerindex.org/geneweb/EWSR1.htm. Accessed on: 20 November 2011.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 165080