Difference between revisions of "Diverticular disease"
Jump to navigation
Jump to search
| Line 44: | Line 44: | ||
Complications: | Complications: | ||
*Diverticulitis. | *Diverticulitis - seen in ~25% of individuals with divertiulosis.<ref name=pmid25253951>{{Cite journal | last1 = Agarwal | first1 = AK. | last2 = Karanjawala | first2 = BE. | last3 = Maykel | first3 = JA. | last4 = Johnson | first4 = EK. | last5 = Steele | first5 = SR. | title = Routine colonic endoscopic evaluation following resolution of acute diverticulitis: is it necessary? | journal = World J Gastroenterol | volume = 20 | issue = 35 | pages = 12509-16 | month = Sep | year = 2014 | doi = 10.3748/wjg.v20.i35.12509 | PMID = 25253951 }}</ref> | ||
*Peformation - [[peritonitis]]. | *Peformation - [[peritonitis]]. | ||
*Diverticular-associated colitis - see below. | *Diverticular-associated colitis - see below. | ||
Revision as of 14:25, 9 October 2015
| Diverticular disease | |
|---|---|
| Diagnosis in short | |
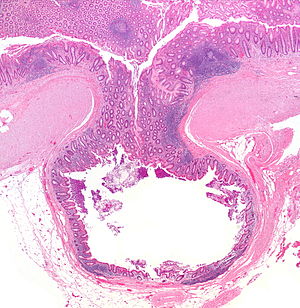 Diverticulum. H&E stain. | |
|
| |
| LM | mucosa/submucosa invaginate into the musuclaris propria |
| Gross | outpouching - best seen after sectioning |
| Grossing notes | partial colectomy for diverticular disease |
| Site | colon - classically sigmoid, other sites |
|
| |
| Associated Dx | diverticulitis, peritonitis, diverticular disease-associated colitis |
| Symptoms | usu. asymptomatic, diverticulitis presents with abdominal pain - classically left lower quadrant |
| Prevalence | common - especially elderly |
| Radiology | colonic outpouchings (typically sigmoid colon) +/-pericolic stranding |
| Clin. DDx | colorectal carcinoma, epiploic appendagitis |
| Treatment | usually conservative, surgical resection (recurrent or perforating diverticulitis) |
Diverticular disease, also diverticulosis, is a common disease of the colon. Inflammation of diverticula is known as diverticulitis.
General
- Very common.
- Typically seen in elderly patients - 50s and 60s.
Presentations:
- Incidental finding on imaging.
- Abdominal pain.
- Classically left lower quadrant.
- +/-Peritoneal signs.
- Blood per rectum.
- Large bowel obstruction.
Complications:
- Diverticulitis - seen in ~25% of individuals with divertiulosis.[1]
- Peformation - peritonitis.
- Diverticular-associated colitis - see below.
- Bowel obstruction - not common, may mimic malignancy.[2]
Diverticular disease-associated colitis
Features:[3]
- Rare.
- Definitions vary somewhat - one is: IBD-like inflammation restricted to areas with diverticular disease.
- Considerable overlap with IBD histologically - no definite histologic findings.
- Rectal biopsy may be used to differentiate from ulcerative colitis.
Gross
- Corrugated - like cardboard.
- Wall thickening (reactive).[4]
- Usually sigmoid colon.
- May be elsewhere, e.g. appendix.[5]
Endoscopic image
Microscopic
Features:
- Mucosa/submucosa invagination into the musuclaris propria (MP).
- At the site the blood vessels supplying the mucosa and submucosa penetrate the MP.[6]
Notes:
- Crypt disortion and/or granulomas should not be seen.[7]
DDx:
- Colorectal carcinoma - may cause a stricture, usually obvious on microscopy.
- Inflammatory bowel disease.
Images
www:
Sign out
SIGMOID COLON, SIGMOIDECTOMY: - DIVERTICULAR DISEASE WITHOUT DIVERTICULITIS. - NEGATIVE FOR MALIGNANCY.
SIGMOID COLON WITH EEA DONUTS, SIGMOIDECTOMY: - DIVERTICULAR DISEASE WITHOUT EVIDENCE OF ACTIVE DIVERTICULITIS. - ONE BENIGN SMALL LYMPH NODE. - NEGATIVE FOR MALIGNANCY.
Perforated
RECTO-SIGMOID, LARGE BOWEL RESECTION: - PERFORATED DIVERTICULITIS WITH SEROSITIS AND ABSCESS FORMATION. - SUBMUCOSAL FIBROSIS. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR MALIGNANCY.
SIGMOID COLON, RESECTION: - COLONIC PERFORATION ASSOCIATED WITH FAT NECROSIS, SEROSITIS AND MICROABSCESS FORMATION, IN THE SETTING OF DIVERTICULAR DISEASE. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ Agarwal, AK.; Karanjawala, BE.; Maykel, JA.; Johnson, EK.; Steele, SR. (Sep 2014). "Routine colonic endoscopic evaluation following resolution of acute diverticulitis: is it necessary?". World J Gastroenterol 20 (35): 12509-16. doi:10.3748/wjg.v20.i35.12509. PMID 25253951.
- ↑ Pereira, JM.; Sirlin, CB.; Pinto, PS.; Jeffrey, RB.; Stella, DL.; Casola, G.. "Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain.". Radiographics 24 (3): 703-15. doi:10.1148/rg.243035084. PMID 15143223.
- ↑ Mulhall, AM.; Mahid, SS.; Petras, RE.; Galandiuk, S. (Jun 2009). "Diverticular disease associated with inflammatory bowel disease-like colitis: a systematic review.". Dis Colon Rectum 52 (6): 1072-9. doi:10.1007/DCR.0b013e31819ef79a. PMID 19581849.
- ↑ Nicholson, BD.; Hyland, R.; Rembacken, BJ.; Denyer, M.; Hull, MA.; Tolan, DJ. (Aug 2011). "Colonoscopy for colonic wall thickening at computed tomography: a worthwhile pursuit?". Surg Endosc 25 (8): 2586-91. doi:10.1007/s00464-011-1591-7. PMID 21359889.
- ↑ Sohn, TJ.; Chang, YS.; Kang, JH.; Kim, DH.; Lee, TS.; Han, JK.; Kim, SH.; Hong, YO. (Jan 2013). "Clinical characteristics of acute appendiceal diverticulitis.". J Korean Surg Soc 84 (1): 33-7. doi:10.4174/jkss.2013.84.1.33. PMID 23323233.
- ↑ West, AB.. "The pathology of diverticulitis.". J Clin Gastroenterol 42 (10): 1137-8. doi:10.1097/MCG.0b013e3181862a9f. PMID 18936652.
- ↑ Goldstein, NS.; Ahmad, E. (Apr 1997). "Histology of the mucosa in sigmoid colon specimens with diverticular disease: observations for the interpretation of sigmoid colonoscopic biopsy specimens.". Am J Clin Pathol 107 (4): 438-44. PMID 9124212.
- ↑ URL: http://histology-group28.wikispaces.com/DigestiveSystemProject. Accessed on: 23 August 2011.

