Breast cancer staging
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
This article deals with breast cancer staging.
An introduction to cancer staging is in the cancer staging article. An introduction to breast pathology is in the breast pathology article.
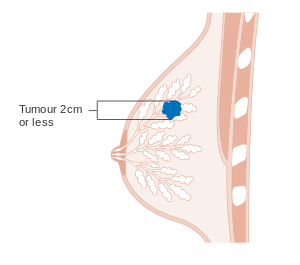
T stage
- pT1: <= 20 mm.
- pT1mic <= 1 mm.
- pT1a > 1 mm and <= 5 mm.
- pT1b > 5 mm and <= 10 mm.
- pT1c > 10 mm and <= 20 mm.
- pT2: > 20 mm and <= 50 mm
- pT3: > 50 mm.
- pT4: chest wall or skin involvement.
Notes:
- Values should be rounded to the nearest millimetre.
- Therefore:
- 1.4 mm would be pT1mic.
- 1.5 mm would be pT1a.
- Therefore:
Images
N stage
Sampling usually selective, i.e. sentinel lymph nodes only.
Indications for lymph node sampling
Indications:[3]
- Extensive DCIS.
- Biopsy suspicious for invasion or with microinvasion.
- Clinical findings (large palable mass) or radiology findings (irregular features) suggestive of invasion.
- Planned mastectomy.
Definitions
Definitions:[4]
- Isolated tumour cells: <=0.2 mm or <=200 cells -- in a single cross-section. †
- Micrometastasis: <=0.2 cm and ( >0.2 mm or >200 cells ).
- Macrometastasis: >0.2 cm.
Notes:
- † The American Cancer Society web site says "or".[4] The CAP protocol says "and/or" and notes it is all subjective.
- Isolated tumour cells are essentially ignored if the there is at least one macrometastasis.
Details
Lymph nodes:[5]
- pN0: nil.
- pN0(i+): <=0.2 mm and <200 cells.
- pN1: 1-3 axillary LNs or internal mammary LNs.
- pN1mi: <=0.2 cm and ( >0.2 mm or >=200 cells ).
- pN1a.
- pN1b.
- PN1c.
- pN2 4-9 positive LNs; internal mammary LNs or axillary LNs.
- pN3.
Sentinel lymph node sampling in breast cancer
Main articles: Sentinel lymph node and Lymph node metastasis
General
- Selective sampling of lymph nodes.
- Used for staging.
- Positive LNs = poorer prognosis.
Notes:
- If there is no palpable disease, there is no mortality benefit from axillary lymph node dissection, i.e. positive axillary lymph nodes can be left in situ without affecting outcome.[6]
- This does not negate the fact that a positive sentinel LN biopsy (vs. negative sentinel LN biopsy) portends a poorer prognosis.
Microscopic
Features:
- Atypical cells.
- Nuclear changes of malignancy:
- Nuclear enlargement + variation in size.
- Variation in shape.
- Hyperchromasia and variation in staining.
- Usually in the subcapsular sinuses.
- Nuclear changes of malignancy:
Pitfalls:
- Naevus cell rests.[7]
IHC
Some hospitals use:
- CAM5.2 (LMWK) - to look for isolated tumour cells and small lymph node metstases.
Note:
- This is falling out of favour. The prognostic significance of isolated tumour cells is measurable but relatively small.[citation needed]
M stage
Distant metastasis:
- cM0(i+) <=0.2 mm focus of tumour cells, without clinical signs and symptoms.
- pM1 focus of tumour cells > 0.2 mm.
See also
References
- ↑ URL: http://www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-staging. Accessed on: 8 July 2010.
- ↑ URL: http://www.cancerhelp.org.uk/type/breast-cancer/treatment/tnm-breast-cancer-staging. Accessed on: 9 July 2010.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2009/InvasiveBreast_09protocol.pdf. Accessed on: 2 April 2012.
- ↑ 4.0 4.1 URL: http://www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-staging. Accessed on: 8 July 2010.
- ↑ URL: http://www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-staging. Accessed on: 8 July 2010.
- ↑ Giuliano AE, Hunt KK, Ballman KV, et al. (February 2011). "Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial". JAMA 305 (6): 569–75. doi:10.1001/jama.2011.90. PMID 21304082.
- ↑ URL: http://www.breastpathology.info/Case_of_the_month/2007/COTM_1107%20discussion.html. Accessed on: 28 November 2010.