Difference between revisions of "Adenocarcinoma of the lung"
Jump to navigation
Jump to search
(→Gross) |
(→IHC) |
||
| Line 109: | Line 109: | ||
==IHC== | ==IHC== | ||
Primary versus metastatic: | Primary versus metastatic: | ||
*TTF-1 +ve. | |||
*CK7 +ve. | *CK7 +ve. | ||
*CK20 -ve. | *CK20 -ve. | ||
Panel for adenocarcinoma versus SCC: | |||
*TTF-1 +ve. | *TTF-1 +ve. | ||
*Napsin A +ve. | |||
*p40 -ve.<ref name=pmid22056955>{{Cite journal | last1 = Bishop | first1 = JA. | last2 = Teruya-Feldstein | first2 = J. | last3 = Westra | first3 = WH. | last4 = Pelosi | first4 = G. | last5 = Travis | first5 = WD. | last6 = Rekhtman | first6 = N. | title = p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma. | journal = Mod Pathol | volume = 25 | issue = 3 | pages = 405-15 | month = Mar | year = 2012 | doi = 10.1038/modpathol.2011.173 | PMID = 22056955 }}</ref> | *p40 -ve.<ref name=pmid22056955>{{Cite journal | last1 = Bishop | first1 = JA. | last2 = Teruya-Feldstein | first2 = J. | last3 = Westra | first3 = WH. | last4 = Pelosi | first4 = G. | last5 = Travis | first5 = WD. | last6 = Rekhtman | first6 = N. | title = p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma. | journal = Mod Pathol | volume = 25 | issue = 3 | pages = 405-15 | month = Mar | year = 2012 | doi = 10.1038/modpathol.2011.173 | PMID = 22056955 }}</ref> | ||
*CK5/6 -ve. | |||
Others: | |||
*p63 -ve -- occasionally +ve. | *p63 -ve -- occasionally +ve. | ||
Revision as of 16:21, 18 February 2014
| Adenocarcinoma of the lung | |
|---|---|
| Diagnosis in short | |
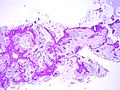
 Lung adenocarcinoma, mucinous. H&E stain. | |
|
| |
| LM | nuclear atypia, eccentrically placed nuclei, usu. abundant cytoplasm (classically with mucin vacuoles), often conspicuous nucleoli, +/-nuclear pseudoinclusions |
| IHC | CK7 +ve, TTF-1 +ve, CK20 -ve, p40 -ve, p63 -ve (usually) |
| Molecular | +/-EGFR mutations, +/-ALK chromosomal translocation (inv(2)(p21p23) -- EML4-ALK fusion) |
| Site | lung - see lung tumours |
|
| |
| Prevalence | most common primary lung tumour |
| Radiology | lung mass - typically peripheral lesion (distant from large airways), may be multifocal |
| Prognosis | moderate |
| Clin. DDx | other lung tumours - primary and metastatic |
| Treatment | surgical resection if feasible |
Adenocarcinoma of the lung, also lung adenocarcinoma, is common malignant lung tumour.
General
- Adenocarcinoma is the most common (primary lung cancer).[1]
- Adenocarcinoma is the non-smoker tumour - SCLC and squamous are more strongly associated with smoking.
Treatment:
- Lung adenocarcinoma may be treated with EGFR inhibitors (e.g. gefitinib (Iressa), erlotinib (Tarceva)).[2]
Patients that receive EGFR inhibitors classically are:[3]
- Non-smokers.
- Female.
- Asian.
- Caucasians also benefit.[4]
Gross
- Classically peripheral lesions.
- May be multifocal.
Image
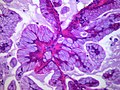
Microscopic
Features:
- Nuclear atypia.
- Eccentrically placed nuclei.
- Abundant cytoplasm - classically with mucin vacuoles.
- Often conspicuous nucleoli.
- +/-Nuclear pseudoinclusions.
Negatives:
- Lack of intercellular bridges.
Patterns:[5]
- Lepidic - tumour grows long the alveolar wall; means scaly covering.[6]
- Acinar - berry-shaped glands.
- Papillary - fibrovascular cores.
- Micropapillary - nipple shaped projections without fibrovascular cores.
- Solid - sheet of cells.
Notes:
- Lymphovascular invasion is common.
- Micropapillary predominant pattern and tumours with any amount of the lepidic pattern are associated with EGFR mutations.[7]
DDx:
- Metastatic adenocarcinoma.
- Colorectal adenocarcinoma.
- Breast adenocarcinoma.
- Squamous cell carcinoma of the lung.
- Non-small cell lung carcinoma - diagnosis should be avoid if possible.
- Malignant mesothelioma.
- Small cell carcinoma of the lung.
- Adenocarcinoma in situ.
Images
www:
- BAC mucinous type adjacent to benign (pathpedia.com).
- BAC mucinous and nonmucinous (cancergrace.org).[8]
Classification
Classification based on extent:[5]
- Adenocarcinoma in situ (AIS) - previously known as BAC.
- Subtypes: nonmucinous, mucinous, mixed mucinous/nonmucinous.
- Minimally invasive adenocarcinoma (MIA).
- Lepidic growth with up to 5 mm of invasion.
- Subtypes: nonmucinous (most common), mucinous, mixed mucinous/nonmucinous.
- Invasive adenocarcinoma:
- Subtypes: micropapillary, mucinous (previously mucinous BAC), colloid, fetal, enteric.
IHC
Primary versus metastatic:
- TTF-1 +ve.
- CK7 +ve.
- CK20 -ve.
Panel for adenocarcinoma versus SCC:
- TTF-1 +ve.
- Napsin A +ve.
- p40 -ve.[9]
- CK5/6 -ve.
Others:
- p63 -ve -- occasionally +ve.
Molecular
- ALK chromosomal translocation (inv(2)(p21p23) -- EML4-ALK fusion).[13]
- Associated with a poor prognosis.[14]
- Amenable to treatment with TKI.
- See lung carcinoma with ALK rearrangement.
Sign out
Biopsy
LUNG, LEFT, BIOPSY: - ADENOCARCINOMA, LEPIDIC GROWTH; INVASION CANNOT BE EXCLUDED IN THIS SMALL SPECIMEN.
Resection
LUNG, LEFT UPPER LOBE, LOBECTOMY: - ADENOCARCINOMA WITH AN ACINAR PATTERN, SOLID PATTERN, MICROPAPILLARY PATTERN AND LEPIDIC PATTERN -- PATTERNS IN ORDER OF PREVALENCE. - MARGINS NEGATIVE FOR MALIGNANCY. - THREE LYMPH NODES NEGATIVE FOR MALIGNANCY (3 POSITIVE/4). - PLEASE SEE TUMOUR SUMMARY.
LUNG, RIGHT UPPER LOBE, LOBECTOMY: - MULTIPLE ADENOCARCINOMAS (x2) WITH AN ACINAR PATTERN, SOLID PATTERN, MICROPAPILLARY PATTERN AND LEPIDIC PATTERN -- PATTERNS IN ORDER OF PREVALENCE. - MARGINS NEGATIVE FOR MALIGNANCY. - FOUR LYMPH NODES NEGATIVE FOR MALIGNANCY (0 POSITIVE/4). - LYMPHOVASCULAR INVASION PRESENT. - PLEASE SEE TUMOUR SUMMARY AND COMMENT. COMMENT: The histology of the two adenocarcinomas resemble one another and lymphovascular invasion is present. These findings favour that the smaller tumor is a metastasis, rather than a synchronous primary.
Micro
Adequacy: scant tissue (<0.5 cm). Gland formation: focal, poorly formed. Cell size: large. Cytoplasm: moderate-to-abundant, grey-eosinophilic. Nucleus location: eccentric. Nuclear pleomorphism: moderate. Nuclear moulding: absent. Nucleoli: present, prominent. Nuclear pseudoinclusions: present.
Number of cores: 3. Length of cores (total): 2.0 cm. Gland formation: present. Cell size: large. Cytoplasm: moderate, grey-eosinophilic. Necrosis: none apparent. Mucin: none. Nucleus location: eccentric. Nuclear pleomorphism: moderate. Nuclear moulding: absent. Nuclear pseudoinclusions: absent. Nuclear shape/arrangment: cigar-like/pseudostratified. Nucleoli: present.
Staging note
- Two small tumours in one lobe is pT3.
- Visceral pleural involvement upgrades small tumours.
See also
References
- ↑ Lutschg JH (January 2009). "Lung cancer". N. Engl. J. Med. 360 (1): 87-8; author reply 88. doi:10.1056/NEJMc082208. PMID 19118313.
- ↑ Sun Y, Ren Y, Fang Z, et al. (October 2010). "Lung adenocarcinoma from East Asian never-smokers is a disease largely defined by targetable oncogenic mutant kinases". J. Clin. Oncol. 28 (30): 4616–20. doi:10.1200/JCO.2010.29.6038. PMID 20855837.
- ↑ Job B, Bernheim A, Beau-Faller M, et al. (2010). "Genomic Aberrations in Lung Adenocarcinoma in Never Smokers". PLoS One 5 (12): e15145. doi:10.1371/journal.pone.0015145. PMC 2997777. PMID 21151896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2997777/.
- ↑ Rosell, R.; Moran, T.; Cardenal, F.; Porta, R.; Viteri, S.; Molina, MA.; Benlloch, S.; Taron, M. (Oct 2010). "Predictive biomarkers in the management of EGFR mutant lung cancer.". Ann N Y Acad Sci 1210: 45-52. doi:10.1111/j.1749-6632.2010.05775.x. PMID 20973798.
- ↑ 5.0 5.1 Travis WD, Brambilla E, Noguchi M, et al. (February 2011). "International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma". J Thorac Oncol 6 (2): 244–85. doi:10.1097/JTO.0b013e318206a221. PMID 21252716.
- ↑ URL: http://medical-dictionary.thefreedictionary.com/lepidic. Accessed on: 8 August 2013.
- ↑ Shim, HS.; Lee, da H.; Park, EJ.; Kim, SH. (Oct 2011). "Histopathologic characteristics of lung adenocarcinomas with epidermal growth factor receptor mutations in the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society lung adenocarcinoma classification.". Arch Pathol Lab Med 135 (10): 1329-34. doi:10.5858/arpa.2010-0493-OA. PMID 21970488.
- ↑ URL: http://cancergrace.org/lung/2007/05/14/bac-mucinous-and-non-mucinous/. Accessed on: 8 August 2013.
- ↑ Bishop, JA.; Teruya-Feldstein, J.; Westra, WH.; Pelosi, G.; Travis, WD.; Rekhtman, N. (Mar 2012). "p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma.". Mod Pathol 25 (3): 405-15. doi:10.1038/modpathol.2011.173. PMID 22056955.
- ↑ John, T.; Liu, G.; Tsao, MS. (Aug 2009). "Overview of molecular testing in non-small-cell lung cancer: mutational analysis, gene copy number, protein expression and other biomarkers of EGFR for the prediction of response to tyrosine kinase inhibitors.". Oncogene 28 Suppl 1: S14-23. doi:10.1038/onc.2009.197. PMID 19680292.
- ↑ URL: http://www.mycancergenome.org/mutation.php?dz=nsclc&gene=egfr&code=l858r. Accessed on: 27 April 2012.
- ↑ Pao, W.; Wang, TY.; Riely, GJ.; Miller, VA.; Pan, Q.; Ladanyi, M.; Zakowski, MF.; Heelan, RT. et al. (Jan 2005). "KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib.". PLoS Med 2 (1): e17. doi:10.1371/journal.pmed.0020017. PMID 15696205.
- ↑ Li, Y.; Ye, X.; Liu, J.; Zha, J.; Pei, L. (Jan 2011). "Evaluation of EML4-ALK fusion proteins in non-small cell lung cancer using small molecule inhibitors.". Neoplasia 13 (1): 1-11. PMID 21245935.
- ↑ Yang, P.; Kulig, K.; Boland, JM.; Erickson-Johnson, MR.; Oliveira, AM.; Wampfler, J.; Jatoi, A.; Deschamps, C. et al. (Jan 2012). "Worse disease-free survival in never-smokers with ALK+ lung adenocarcinoma.". J Thorac Oncol 7 (1): 90-7. doi:10.1097/JTO.0b013e31823c5c32. PMID 22134072.